Acne Fulminans Is a Very Rare and Extremely Severe Form of Acne that Affects Young Caucasian Males

The Essential Info
Acne fulminans is an extremely rare, severe form of acne that presents numerous painful nodules and/or cysts covering large areas of the skin along with symptoms that affect the whole body, such as fever, fatigue, and muscle pain.
Notably, nodules and cysts in acne fulminans fill with blood and rapidly turn into open wounds that often leave massive, disfiguring scars. The disease debuts explosively and almost always affects young white males.
Treatment normally consists of a combination of oral corticosteroids and isotretinoin (Accutane®).

The Science
Definition
Acne fulminans is an extremely rare, severe form of acne with an explosive onset that normally affects white males between 13 – 22 years old, and comes with systemic symptoms (symptoms that affect the whole body) like fever, fatigue, and pain in the muscles and joints.1,2
Due to its severity, acne fulminans often leaves massive, disfiguring scars.
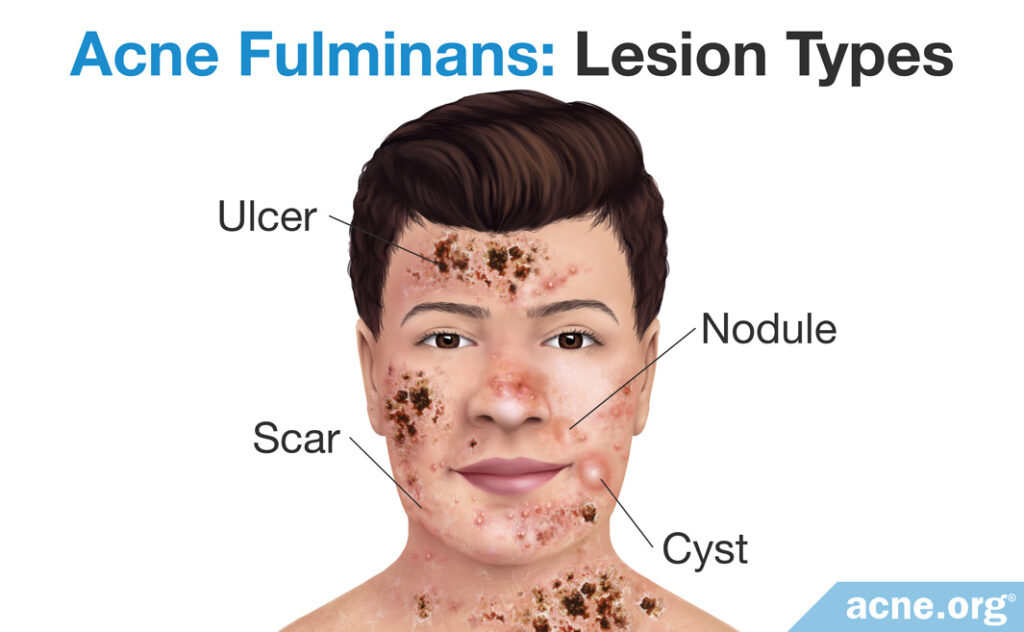
This type of acne falls under the umbrella term nodulocystic acne, which is used to refer to any type of acne that features large lesions (over 5mm in diameter) called nodules and/or cysts. The nodules and cysts in acne fulminans are unique in that they fill with blood and rapidly turn into open wounds called ulcers.
Incidence
Acne fulminans is extremely rare. Fewer than 200 cases have been documented so far.3 The disease usually affects Caucasian males who are 13 – 22 years of age who have regular acne at first. On a few occasions, acne fulminans has been diagnosed in females.
Causes
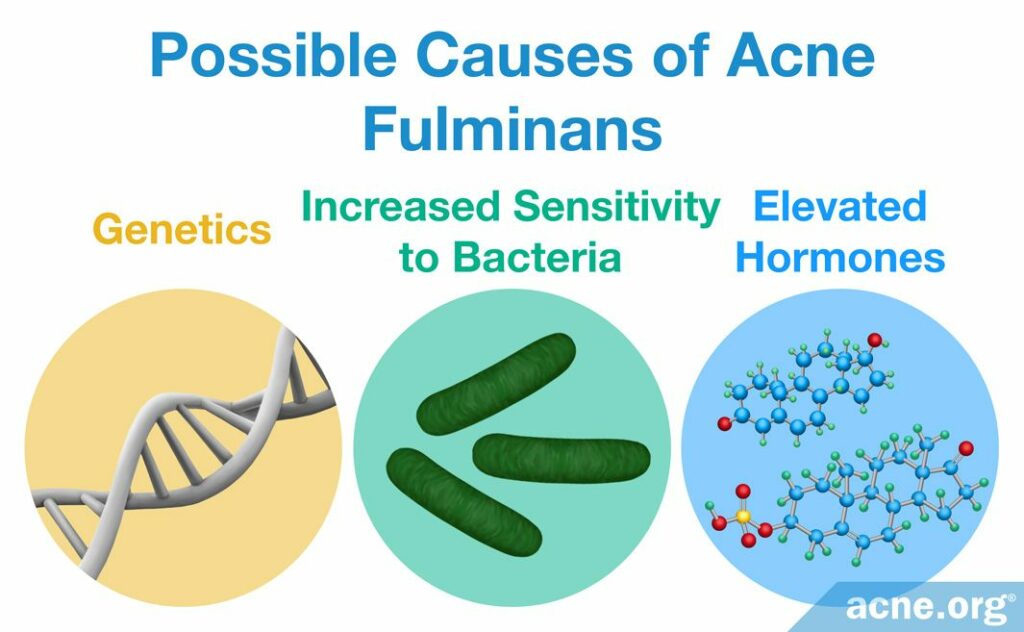
Nobody knows what causes acne fulminans, but evidence suggests that the following three factors play a role:
- Genetics: Researchers suspect there is a gene responsible for predisposition to acne fulminans, which means that if a person’s parents suffered from acne fulminans, that person’s chances of getting it are much higher. Medical literature describes four cases in which identical twins developed acne fulminans with very similar symptoms.1
- Increased sensitivity to bacteria: Cutibacterium acnes (C. acnes), the bacteria associated with acne, lives in everyone’s skin. Some researchers hypothesize that the immune system in people with acne fulminans reacts to the presence of the bacteria even more so than in regular acne.1 The immune system in these people may be overactive in general, and may therefore respond to acne bacteria with extreme inflammation.3
- Elevated hormones: Medical professionals suspect that androgens (male hormones present in both males and females) contribute to acne fulminans, particularly because androgens peak in puberty and young adolescent males get affected most often. Elevated dehydroepiandrosterone sulfate (DHEAS) and testosterone (both male hormones) are a frequent finding in patients with nodulocystic acne, but no major studies have been performed to determine if that is also true for acne fulminans.
Some case reports have described bodybuilders who developed acne fulminans after using anabolic steroids.3 Anabolic steroids are natural or artificially made androgens that can help a person increase muscle mass and include testosterone. The fact that taking anabolic steroids can trigger acne fulminans lends support to the idea that elevated androgen levels may have something to do with this disorder.
Some case studies have reported on patients who started taking the oral acne medication isotretinoin for severe acne and then developed what looked like acne fulminans. These patients’ acne worsened to very severe acne with bloody lesions after isotretinoin treatment began. However, they did not develop systemic symptoms like fever and muscle pain. Therefore, some doctors call this condition pseudo-acne fulminans, which means “false acne fulminans,” and are still determining whether its treatment should be similar to “regular” acne fulminans.3,4
Symptoms
Acne fulminans usually occurs in individuals who have had mild-to-moderate acne for some time. The disease typically debuts in the early or middle teen years and almost never after the early twenties.
Abrupt onset: The onset of the disease is very abrupt. Typically, a person has just average, regular acne for some time, usually for a year or two, and then suddenly numerous nodules and cysts begin to emerge on large areas of the skin on the upper chest, back, neck, and face.5,6 Less severe acne lesions like whiteheads, blackheads, papules, and pustules might be present as well, but they are never a dominant feature.
Nodules and cysts: Nodules and/or cysts in acne fulminans are plentiful, and the neighboring lesions tend to merge with each other, forming extra-large lesions. Both nodules and cysts are over 5 mm in diameter and are tender and painful. The difference is that nodules are fibrous lesions that do not contain pus, whereas cysts contain “foul-smelling” pus-like material. Unlike in other forms of severe, nodulocystic acne, nodules and cysts in acne fulminans fill with blood and rapidly turn into painful ulcers (open wounds).1,5 Healing of ulcers can be extremely slow, often resulting in massive, disfiguring scars.
Systemic symptoms: Acne fulminans is a systemic disease, which means that not only is the skin affected but the rest of the body as well. The most frequent systemic symptoms include:
- Fever
- Fatigue
- Muscle pain
- Tenderness, swelling, and pain in the joints
- Softening of the bones and increased risk of fractures
- Pain in the bones (occurs approximately in four out of ten patients)
- Enlargement of the liver and spleen
- Anemia (reduced red blood cell count)
- Leukocytosis (increased white blood cell count)1-6
Scars: Scars in acne fulminans are often severe and widespread and can be atrophic (indented) or hypertrophic (raised above the skin).
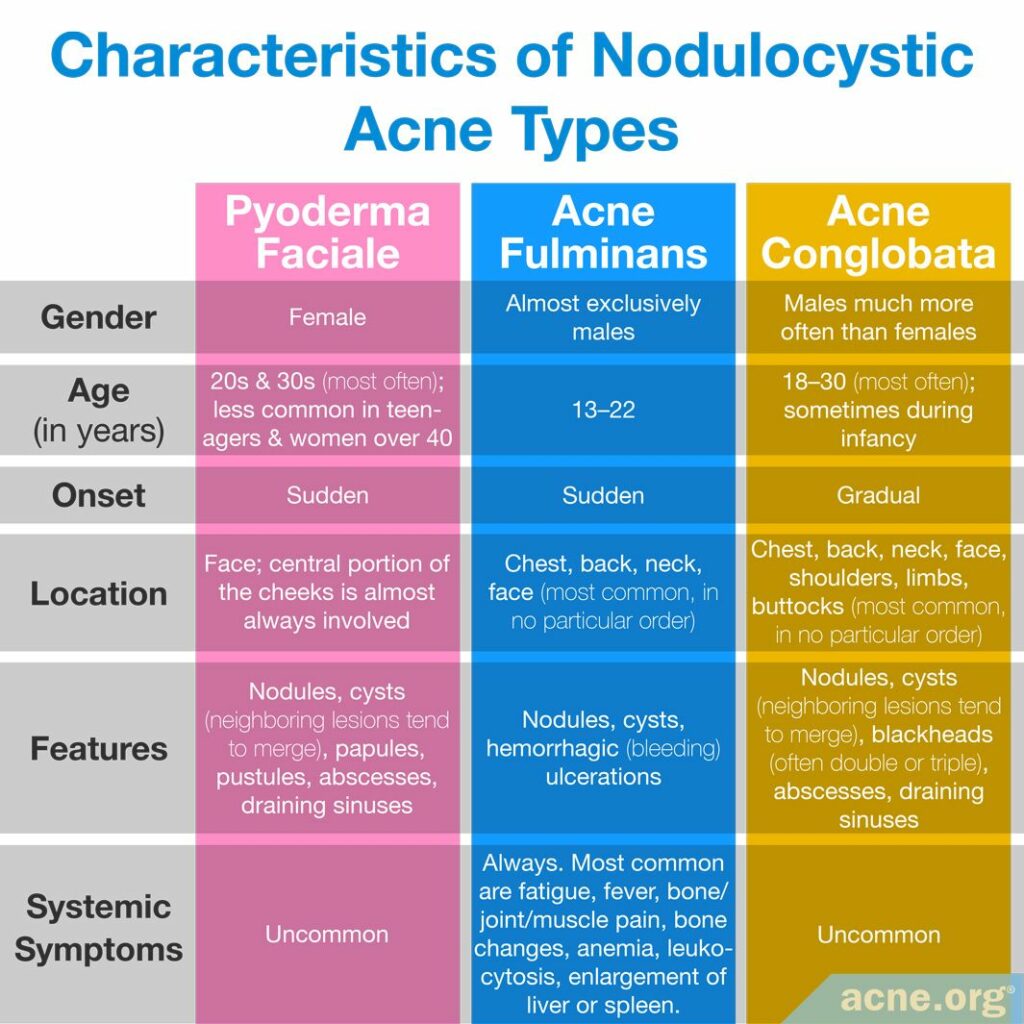
Acne Fulminans vs. Other Severe Forms of Acne
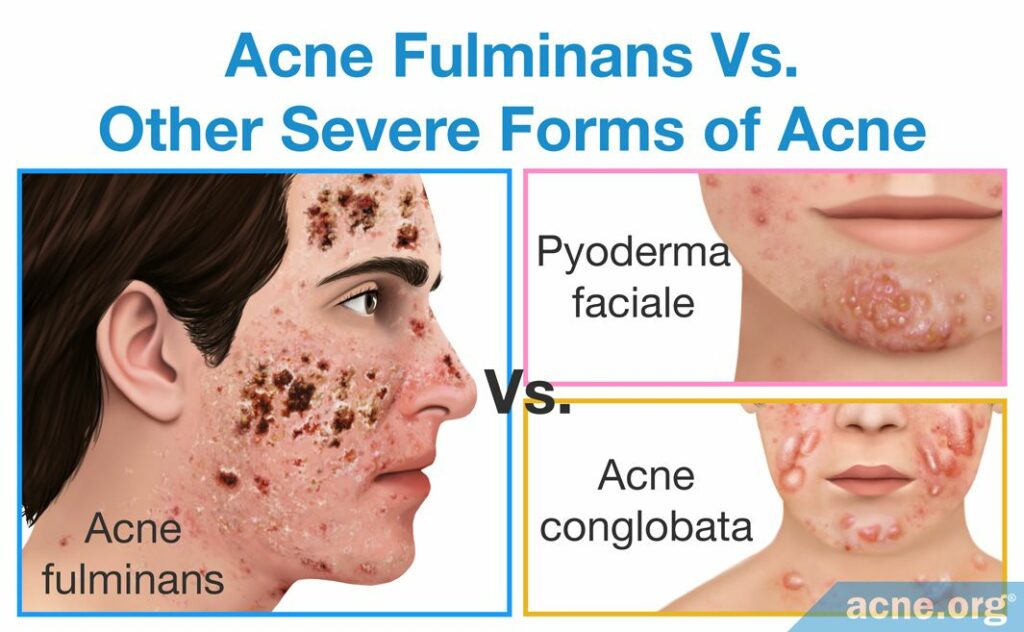
Acne conglobata
In acne conglobata, lesions tend to appear on the same areas of the face and body as in acne fulminans. Also, like in acne fulminans, neighboring nodules/cysts in acne conglobata often merge together and form extra-large, inflammatory lesions. What helps to distinguish between the two conditions is that nodules and cysts in acne fulminans fill with blood and rapidly turn into open wounds, while in acne conglobata they normally do not fill with blood and persist as raised lesions covered by the skin. In addition, acne fulminans patients commonly present with systemic symptoms, such as fever, joint pain, and weight loss, which are very uncommon in acne conglobata.
Pyoderma faciale
Pyoderma faciale is another form of nodulocystic acne, characterized by a sudden emergence of intense redness and large merging nodules and/or cysts on the face. The disease is relatively easy to differentiate from acne fulminans because pyoderma faciale occurs exclusively in females and affects the face only.
Treatment

Because acne fulminans includes skin symptoms as well as systemic symptoms, it needs to be treated by two types of doctors at the same time:
- A dermatologist: A dermatologist will monitor and treat the skin symptoms.
- An internist: An internist or internal medicine specialist will monitor and treat the systemic symptoms.3
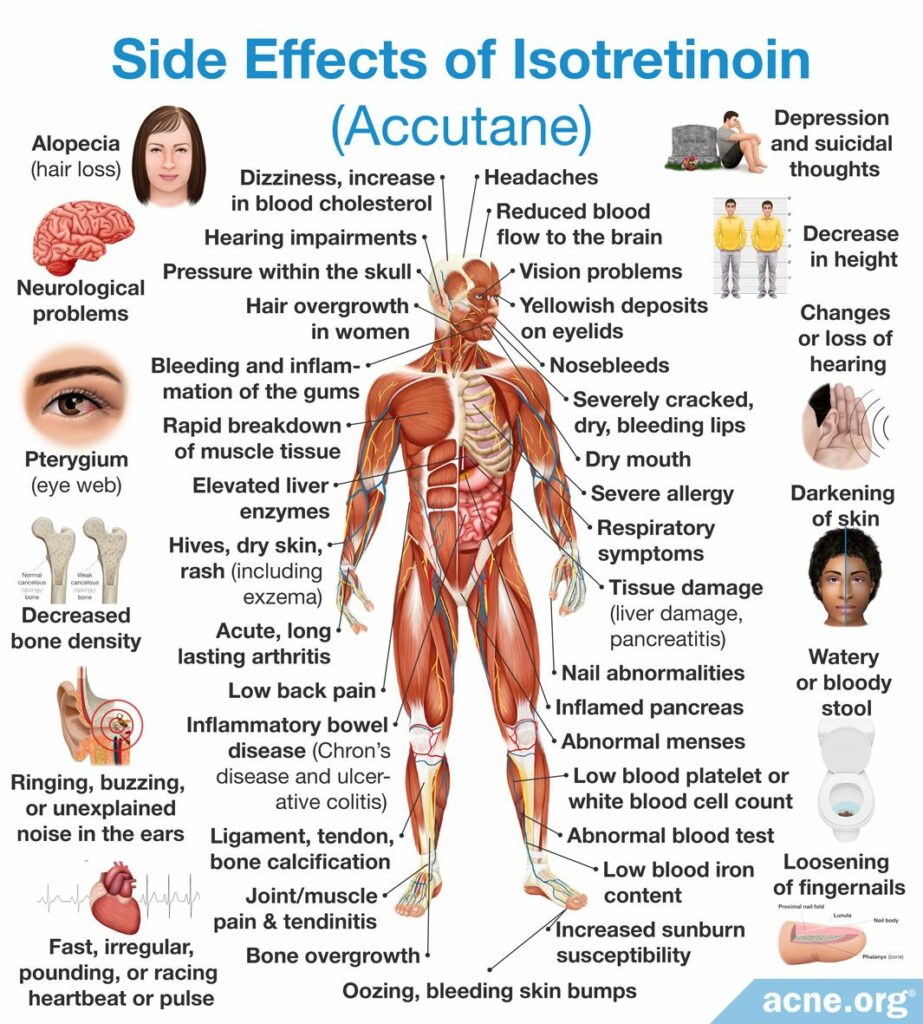
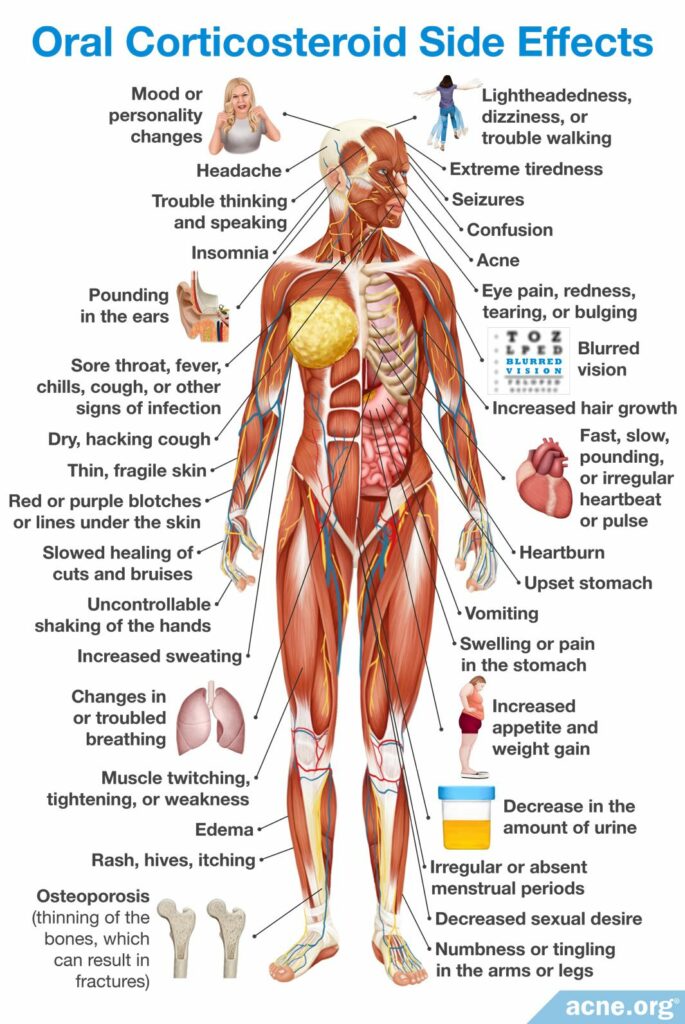
When it comes to the best course of treatment, because acne fulminans is so rare, very little clinical data is available for analysis. The only relatively large study suggested a combination of oral corticosteroids (e.g., prednisolone) and isotretinoin.2,7 Isotretinoin is a highly controversial drug that must be taken only in close supervision with a doctor and is associated with numerous hazardous health effects. Only the severity of the disease justifies the use of this treatment option.

Oral corticosteroids and isotretinoin
Usually, treatment starts with a corticosteroid for the first six weeks. Corticosteroids work well on systemic symptoms and also reduce acne.
Isotretinoin, which is the workhorse that clears the severe acne, is usually incorporated 3 – 6 weeks after corticosteroid treatment has begun, so the treatments sometimes overlap.1,7,8 However, some doctors prefer to start both the corticosteroid and isotretinoin at the same time.9
In total, the treatment course usually lasts approximately six months.
Clinical trials on the effectiveness of oral corticosteroids plus isotretinoin in the treatment of acne fulminans

A study published in the British Journal of Dermatology in 1999 reported that starting treatment with oral prednisolone and adding isotretinoin later in the course was the most effective treatment regimen for acne fulminans. Giving prednisolone first and adding isotretinoin a few weeks later was better than the converse because corticosteroids worked on systemic symptoms quickly.7

A study published in the journal Dermatology in 2017 found that starting oral prednisolone and isotretinoin at the same time, and then tapering off the use of prednisolone after one month, produced good results in 26 patients with acne fulminans. After two weeks, all patients experienced a full recovery from systemic symptoms. After a full month of treatment, 65% or about two-thirds of the patients saw a reduction in the number of acne lesions by at least 50%. The remaining patients needed up to 6 months of isotretinoin treatment to see similar results.9
Despite being highly effective in treating severe acne, isotretinoin often comes with a long list of side effects and, sometimes severe, toxic reactions. This is why it is approved for use only for severe, nodulocystic acne. Some side effects may be lifelong.
The most frequent side effects include:
- Inflammation of lips (90%)
- Dryness of skin and mucous membranes (80%)
- Pink eye (40%)
- Itching (40%)
- Gastrointestinal symptoms, such as nausea, vomiting, and abdominal pain (20%)
- Muscle and/or joint pain (16%)
- Increased sensitivity to light (10%)
Toxic reactions: Possible toxic reactions associated with the administration of isotretinoin might include inflammatory bowel disease and increased intracranial (in the head) pressure that causes moderate-to-severe headaches and visual impairments, such as blurred and double vision, difficulty seeing to the side, and brief episodes of blindness.10 The incidence of these events is unknown, but they are rather uncommon.
AVOID PREGNANCY! Isotretinoin is contraindicated in pregnancy due to its severe, adverse effects on the fetus.10 In fact, it is the No.1 birth defect-causing medication on the market. Birth defects are often very severe, including death. Therefore, females are urged to obtain two (2) negative pregnancy tests prior to starting therapy. Additionally, women must use two (2) forms of contraception for 30 days both before and after treatment with isotretinoin.
In rare situations, isotretinoin might actually cause acne fulminans: Medical researchers have recently reported on three cases of teen males whose severe acne turned into acne fulminans after starting isotretinoin treatment.11-13 This is not a concern if you already have acne fulminans, and your doctor prescribes isotretinoin to treat the condition. However, if you are considering taking isotretinoin for other types of severe acne, this might be worth bringing up with your doctor.
Other treatments

Data on alternative treatment modalities for acne fulminans is limited and comes from scant case reports. On several occasions, prednisolone (a corticosteroid) was used in combination with one or another of the following drugs:1,7,14
- Cyclosporine (regulates immune response)
- Infliximab (regulates immune response)
- Dapsone (anti-inflammatory)
- Oral antibiotics (erythromycin, tetracycline, or minocycline)
Researchers have concluded that a combination of prednisolone and erythromycin may be a viable treatment option during the early stages of acne fulminans and cystic acne, but isotretinoin should be added to establish long-term remission.
Expand to read results of research
Prednisolone combined with erythromycin was given to 6 patients with cystic acne. The treatment responses were compared to those in 6 patients with cystic acne receiving isotretinoin and erythromycin and also to those in 3 patients with acne fulminans treated with prednisolone and erythromycin. During the first 4 weeks cystic acne showed a clear improvement in 5 out of 6 patients in both treatment groups. A similar improvement occurred in all 3 patients with acne fulminans. When corticosteroid was stopped, 2 out of 5 patients with cystic acne had a relapse and needed isotretinoin for complete control. In the isotretinoin-treated group, one patient with cystic acne needed prednisolone because the acne worsened to an ulcerative form. The results show that prednisolone combined with erythromycin is an effective treatment during the early stages of cystic and acne accompanied by the symptoms of a fever, but isotretinoin is needed for long-term control.14
References
- Zaba, R. Acne Fulminans. Emedicine.medscape.com (2016). http://emedicine.medscape.com/article/1072815-overview#showall
- Habif, T. Clinical Dermatology: A Color Guide to Diagnosis and Therapy (6th Edition). 231 – 233 (Saunders, 2015). https://www.elsevier.com/books/clinical-dermatology/habif/978-0-323-26183-8
- Zito, P. M. & Badri, T. Acne Fulminans. [Updated 2020 Apr 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459326/
- Grando, L. R., Leite, O. G. & Cestari, T. F. Pseudo-acne fulminans associated with oral isotretinoin. An Bras Dermatol 89, 657‐659 (2014). https://pubmed.ncbi.nlm.nih.gov/25054758/
- Jansen, T. & Plewig, G. Acne fulminans. Int J Dermatol 37, 254 – 257 (1998). https://link.springer.com/chapter/10.1007/978-3-642-59715-2_24
- Karvonen, S. Acne fulminans: Report of clinical findings and treatment of twenty-four patients. J Am Acad Dermatol 28, 572 – 579 (1993) https://pubmed.ncbi.nlm.nih.gov/7681856/
- Seukeran, D. C. & Cunliffe, W. J. The treatment of acne fulminans: a review of 25 cases. Br J Dermatol 141, 307 – 309 (1999) https://pubmed.ncbi.nlm.nih.gov/10468806/
- Zito, P. M & Badri, T. Acne Fulminans. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023. https://pubmed.ncbi.nlm.nih.gov/29083789/
- Massa, A. F., Burmeister, L., Bass, D. & Zouboulis, C. C. Acne fulminans: Treatment experience from 26 Patients. Dermatology 233, 136‐140 (2017). https://pubmed.ncbi.nlm.nih.gov/28768255/
- Hodgson, B. & Kizior, R. Saunders nursing drug handbook 2012. (W. B. Saunders Co., 2014)
- Sánchez-Velázquez, A., Falkenhain-López, D., Arroyo-Andrés, J., Montero-Menárguez, J., García-Donoso, C. & Postigo-Llorente, C. Apremilast: A novel adjuvant treatment for refractory isotretinoin-induced acne fulminans. Dermatol Ther 35, e15637 (2022). https://pubmed.ncbi.nlm.nih.gov/35703093/
- Li, A. W. & Antaya, R. J. Isotretinoin-induced acne fulminans without systemic symptoms with concurrent exuberant granulation tissue. Pediatr Dermatol 35, 257-258 (2018). https://pubmed.ncbi.nlm.nih.gov/29314240/
- Marasca, C., Fabbrocini, G., Abategiovanni, L., Camela, E., Nocerino, M., Di Guida, A. & De Fata Salvatores, G. Adalimumab in the management of isotretinoin-induced acne fulminans: Report of a case. Skin Appendage Disord 7, 115-119 (2021). https://pubmed.ncbi.nlm.nih.gov/33796557/
- Karvonen, S. Systemic corticosteroid and isotretinoin treatment in cystic acne. Acta Derm Venereol 73, 452 – 455 (1993). https://pubmed.ncbi.nlm.nih.gov/7906462/
 Acne.org Products
Acne.org Products