It’s the Result of Genetics and Inflammation

The Essential Info
When an acne lesion is healing, the body must replace damaged tissue to heal the skin. Replacing this tissue is a highly intricate process that involves balancing collagen production. If the body produces too little collagen, an indented scar results. And if the body produces too much collagen, a raised scar results.
Why Do Some People Scar More Easily? Research suggests that the skin of people who scar tends to respond to an acne lesion with an inflammatory response that is too weak and too extended. Genetics also plays a part, meaning if your mom and/or dad have acne scars, you are more likely to develop them too.

The Science
- Types of Acne Scars
- Steps from Pimple to Scar
- Why Some People Scar More than Others
- Might It Be Possible to Prevent Scars from Forming?
Patients suffering from acne, particularly more severe acne, very often develop some amount of scarring. In fact, researchers investigating the prevalence of scarring in 185 acne patients treated at an acne clinic found that 95% had scarring somewhere on their face or body.1
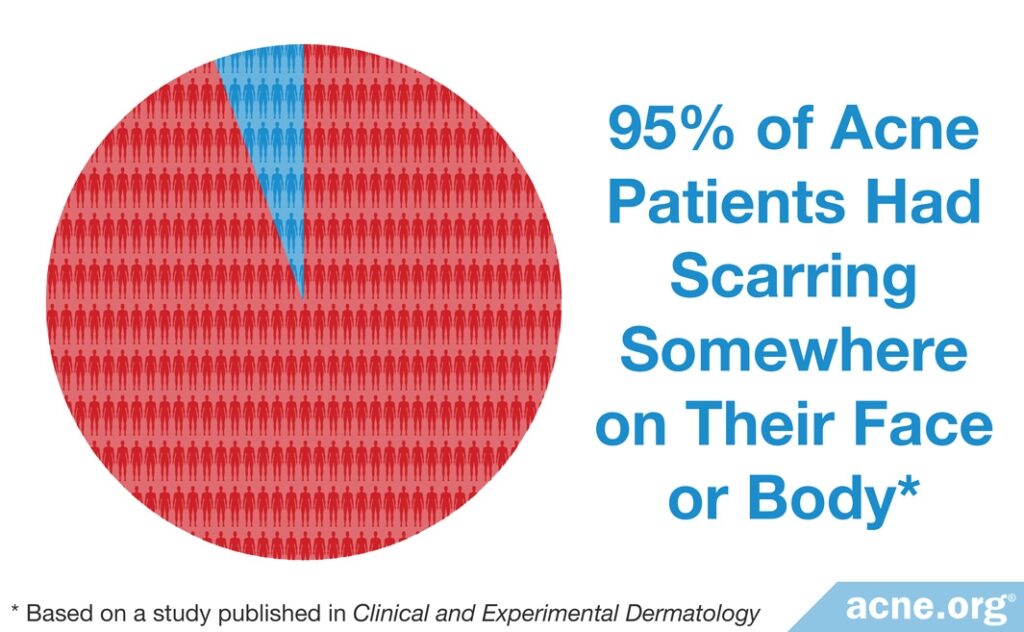
Scarring on the face is equally common in males and females, whereas scarring on the body occurs more frequently in males.
Not everyone is equally prone to acne scarring. Individual differences in the immune system and genetics help explain why certain individuals are more susceptible to scarring.
Types of Acne Scars
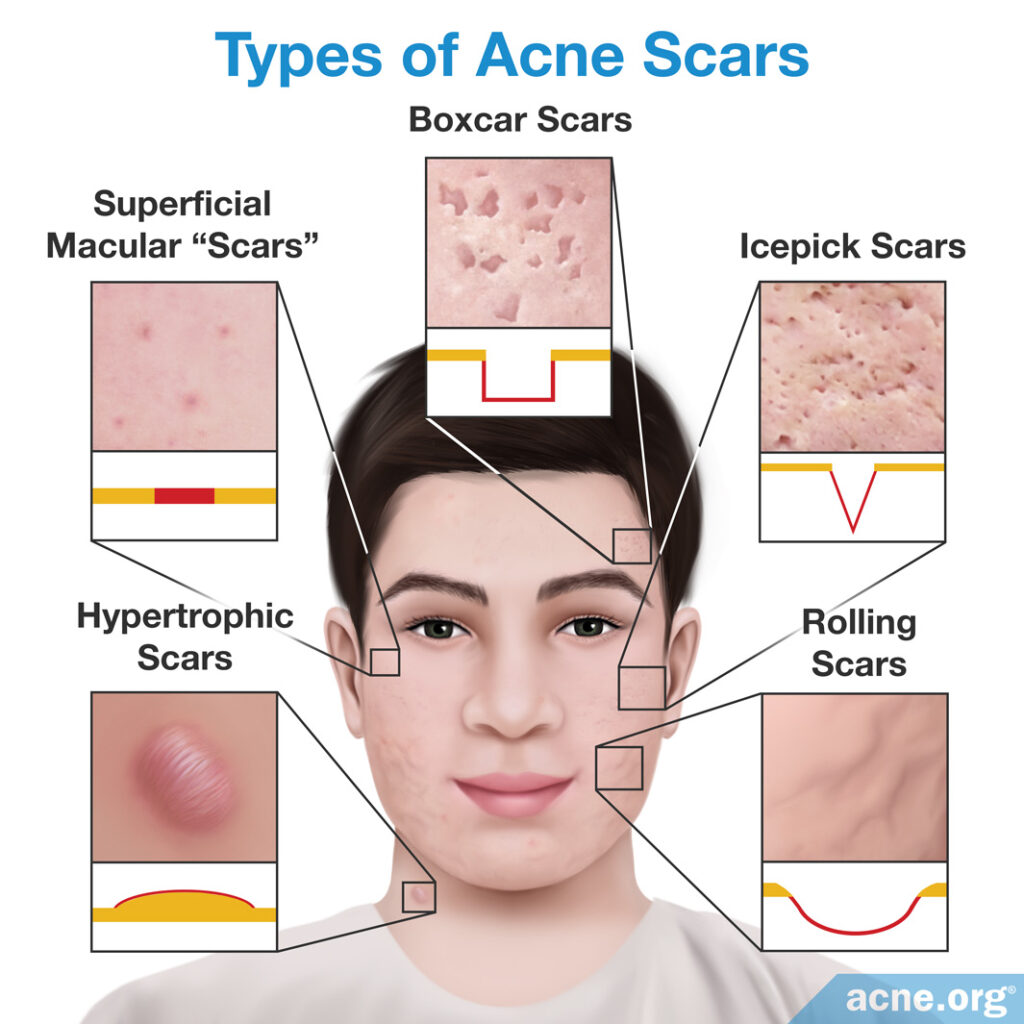
The pimple healing process can produce three types of acne scars:
- Atrophic (indented) scars are sunken due to loss of an important skin protein called collagen. Often, these scars are given specific names, like “ice-pick” scars, “rolling” scars, or “boxcar” scars, based on the appearance and depth of the skin damage. These are much more common than hypertrophic scars.
- Hypertrophic (raised) scars are raised due to a gain of collagen.
- Superficial macular scars are temporary “scars” that involve a darkening of the skin after the acne lesion heals. This is also called hyperpigmentation. There is some controversy over whether these are really scars since they fade with time–generally within 3 – 18 months.2
Steps from Pimple to Scar
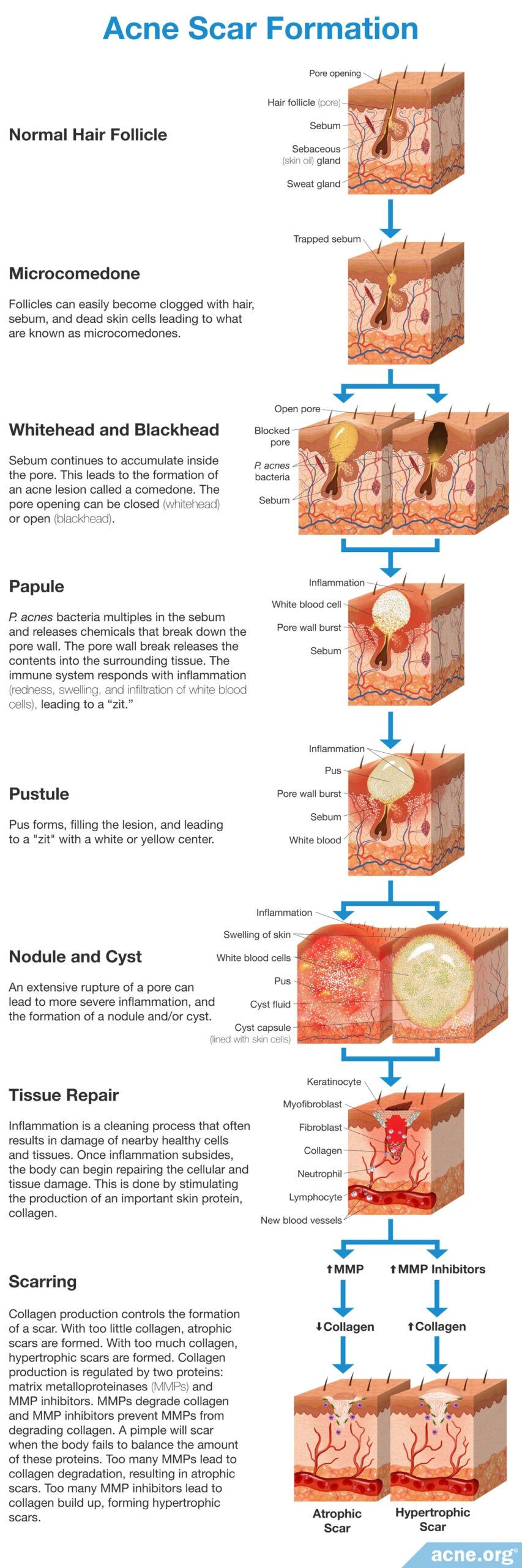
Acne scar formation occurs in 4 steps:
1. Initial clogged pore
The surface of the body is covered with microscopic hair follicles that produce tiny hairs along with skin oil. These follicles, often called pores, can become clogged.2
2. Formation of an acne lesion
Once a pore becomes clogged, skin oil, which normally drains to the surface, is trapped inside and accumulates. Acne bacteria thrives on this skin oil and multiplies inside the skin. The pore expands, and the wall of the pore breaks within the skin. The immune system responds with inflammation, which consists of redness, swelling, and an infiltration of white blood cells. This forms a run-of-the-mill “pimple” or “zit.”2,3 If the clogged pore ruptures into deeper layers of the skin, it can develop into a larger (over 5 mm in diameter), severe inflamed acne lesion like a nodule or cyst. Any type of inflamed acne lesion can scar, but nodules and cysts are more prone to scarring.
3. Tissue repair
The body uses inflammation to repair skin tissue. This cleaning process often results in damage of nearby healthy cells and tissues. After the inflammation subsides, the body begins repairing the cellular and tissue damage, which it does by stimulating the production of an important skin protein, collagen.4
4. Skin tissue remodeling
The amount of collagen the body produces controls the formation of a scar. If the body produces too little collagen, atrophic (indented) scars will form. If the body produces too much collagen, hypertrophic (raised) scars will form.
Here comes the deep science: The body controls collagen production through two proteins: matrix metalloproteinases (MMPs) and MMP inhibitors. MMPs are proteins that degrade collagen, and MMP inhibitors are proteins that prevent MMPs from degrading collagen. If the body produces too many MMPs, then an abundance of collagen is degraded, which results in atrophic scars. But if the body produces too many MMP inhibitors, then collagen can build up and form hypertrophic scars. In summary, a pimple will scar when the body fails to balance the amount of MMPs and MMP inhibitors, resulting in the production of too little or too much collagen.4
Skin is essentially composed of cells (mainly fibroblasts, endothelial cells, and keratinocytes) and ECM. The latter is a dynamic, organized interlocking mesh of many different secreted macromolecules and proteolytic enzymes. The ECM has many functions, including: providing structure, organization, and orientation to cells and tissues; controlling morphogenesis and cellular metabolism by acting as a template for cell migration, proliferation, apoptosis, differentiation, and adhesion; regulate cell activity and function via directly binding to integrins and other cell surface receptors; act as a reservoir for growth factors and regulate their bioavailability.5
Why Some People Scar More than Others
The natural pimple healing process can vary greatly between individuals. Research thus far has focused on examining:
- The immune system
- Genetics
Immune system
The immune system controls inflammation in our bodies. Research has found that the immune system can control the response to repairing the skin after a pimple.
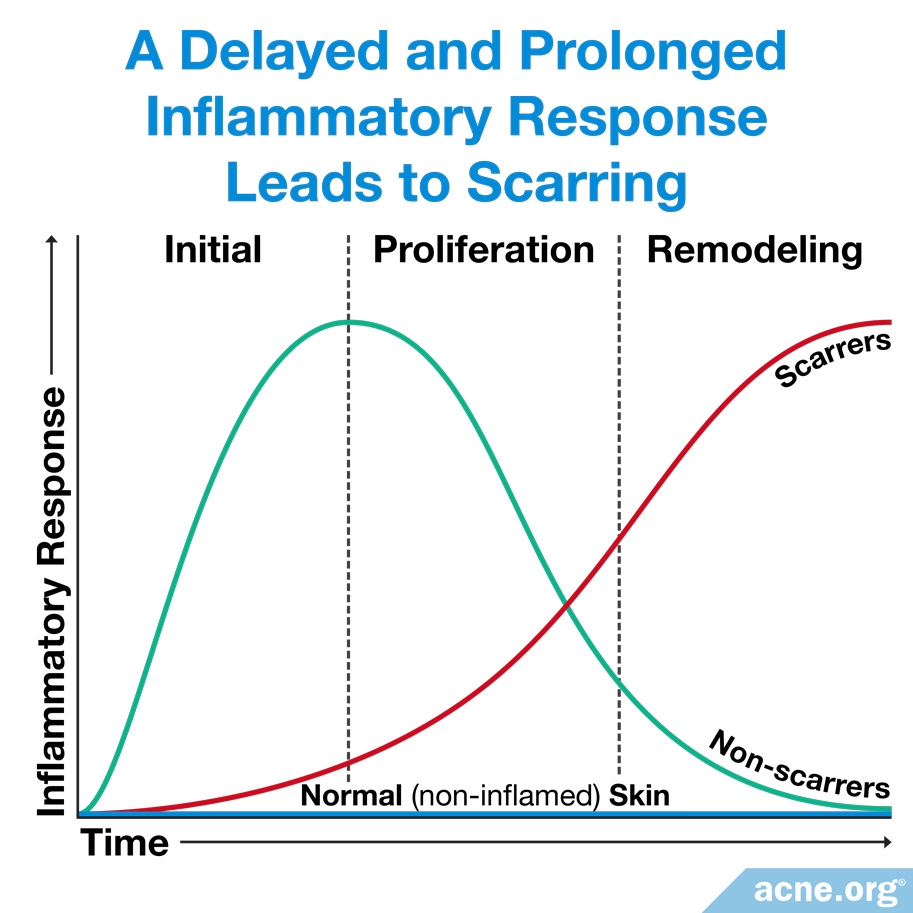
People who are not prone to acne scarring show a strong initial inflammatory response that is effective at quickly repairing tissue. After the tissue is repaired, this inflammatory response returns to normal levels.
People who are prone to acne scarring show a weaker and delayed/extended inflammation that is not as effective at repairing tissue. Chronic inflammation can be damaging to the skin tissue and cause acne scarring.6
Providing some evidence in support of this idea, one recent study found differences in the levels of two inflammation markers between acne patients who develop scars and those who don’t. Those with scars had:
- Lower levels of a protein called hepcidin in the blood: This protein is a sign of a strong initial inflammatory response.
- Higher levels of a protein called CRP in the blood: This protein can be a sign of ongoing low-level inflammation in the body.7
Genetics
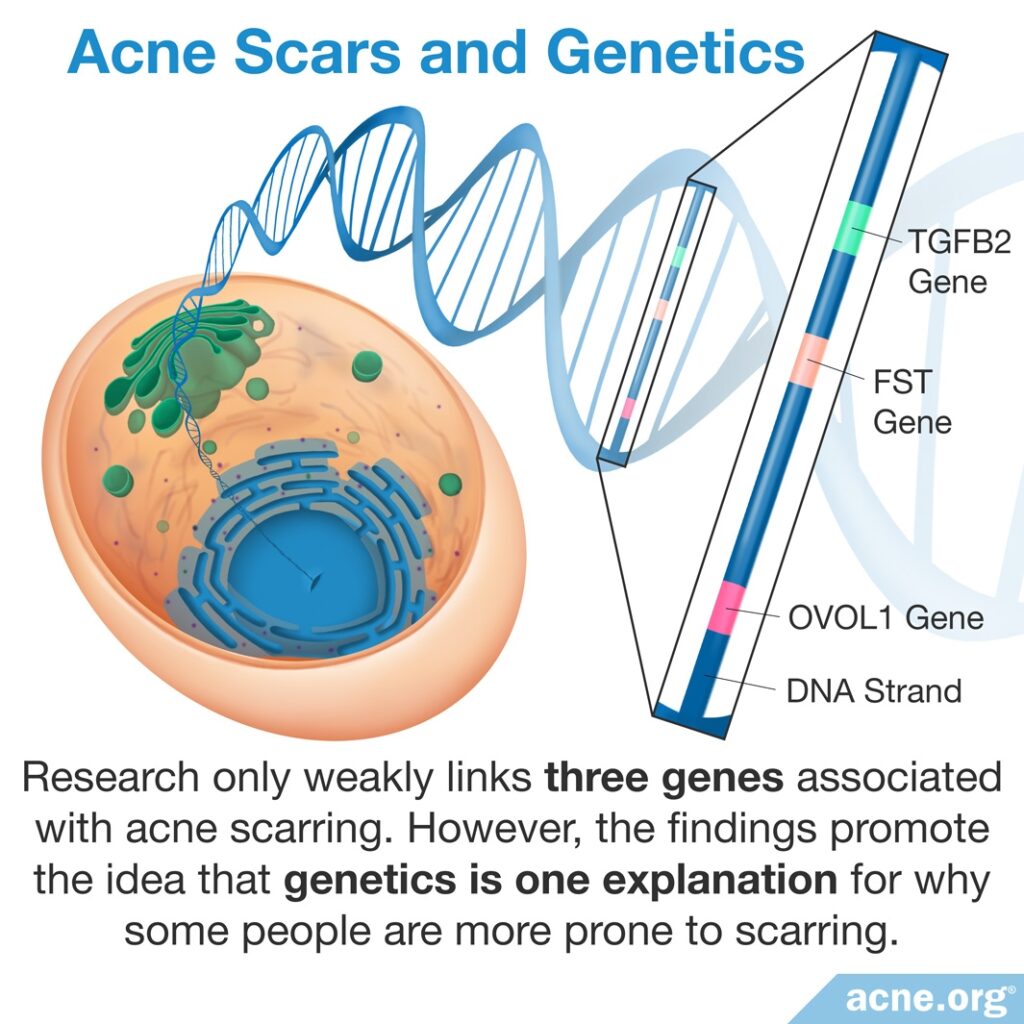
From the three studies we have so far, it appears that genetics may play a part in whether someone is more prone to scars.
The first study observed that a specific gene is found more often in patients prone to acne scarring and believe that it is connected with skin cell growth and clogged pores.8
The second study identified a gene that was also present more often in patients prone to acne scarring, but the gene’s function remains unknown.9
Finally, a third study found a location on a genetic structure called a chromosome containing many genes that they believe are involved in acne scar formation.10
These findings promote the idea that genetics is one explanation for why some people are more prone to acne scarring than others. Scientists need to perform more research to confirm these findings, as well as to identify other potentially associated genes.
Might It Be Possible to Prevent Scars from Forming?
In theory, it should be possible for acne lesions and other wounds to heal without forming scars. We know this because wounds in the mouth heal without scars or with only minimal scars. In addition, if a fetus in the early stages of pregnancy becomes injured, the wound can usually heal without a scar.11
However, in teens and adults, as we have seen, acne lesions often do leave scars. Researchers are continuously studying the scarring process to understand how it might be prevented. For now, the best line of defense we have against acne scars is to use proven acne treatments, reducing the chances of breakouts that might end up leaving scars.
An final important thing to note here is that picking at the skin can cause more scarring than a pimple itself. Therefore, it is absolutely imperative that you don’t pick at a healing acne lesion. If you want to pop a pimple, do that carefully and correctly, but never, ever pick at your skin.
References
- Layton, A. M., Henderson, C. A. & Cunliffe, W. J. A clinical evaluation of acne scarring and its incidence. Clin Exp Dermatol 19, 303 – 308 (1994). https://www.ncbi.nlm.nih.gov/pubmed/7955470
- Goodman, G. J. Post-acne scarring: a short review of its pathophysiology. Australas J Dermatol 42, 84 – 90 (2001). https://www.ncbi.nlm.nih.gov/pubmed/11309028
- Goodman, G. J. Postacne scarring: a review of its pathophysiology and treatment. Dermatol Surg 26, 857 – 871 (2000). https://www.ncbi.nlm.nih.gov/pubmed/10971560
- Fabbrocini, G. et al. Acne scars: pathogenesis, classification and treatment. Dermatol Res Pract 2010, 1 – 13 (2010). https://www.ncbi.nlm.nih.gov/pubmed/20981308
- Xue, M. & Jackson, C. J. Extracellular matrix reorganization during wound healing and its impact on abnormal scarring. Adv Wound Care (New Rochelle) 4, 119-136 (2015). https://pubmed.ncbi.nlm.nih.gov/25785236/
- Holland, D. B. et al. Inflammation in acne scarring: a comparison of the responses in lesions from patients prone and not prone to scar. Br J Dermatol 150, 72 – 81 (2004). https://www.ncbi.nlm.nih.gov/pubmed/14746619
- El-Taweel, A. A., Salem, R. M. & El-Shimi, O. S. Predictive value of serum markers for postacne scarring. J Cosmet Dermatol 17, 491-494 (2018). https://pubmed.ncbi.nlm.nih.gov/28857398/
- Navarini, A. A. et al. Genome-wide association study identifies three novel susceptibility loci for sever acne vulgaris. Nat Commun 5, 4020 (2014). https://www.ncbi.nlm.nih.gov/pubmed/24927181
- Zhang, M. et al. A genome-wide association study of severe teenage acne in European Americans. Hum Genet 133, 259 – 264 (2014). https://www.ncbi.nlm.nih.gov/pubmed/24114350
- He, L. et al. Two new susceptibility loci 1q24.2 and 11p11.2 confer risk to severe acne. Nat Commun 5, 2870 (2014). https://www.ncbi.nlm.nih.gov/pubmed/24399259
- Marshall, C. D., Hu, M. S., Leavitt, T., Barnes, L. A., Lorenz, H. P. & Longaker, M. T. Cutaneous scarring: Basic science, current treatments, and future directions. Adv Wound Care (New Rochelle) 7, 29-45 (2018). https://pubmed.ncbi.nlm.nih.gov/29392092/
 Acne.org Products
Acne.org Products