Cystic Acne Comes with Large Lesions Called Nodules and/or Cysts

The Essential Info
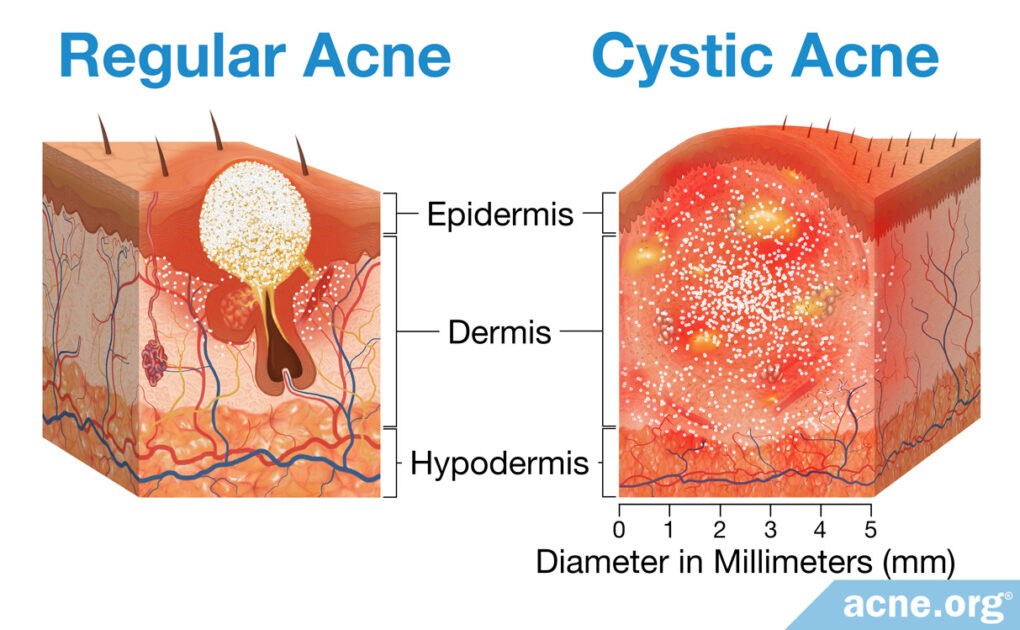
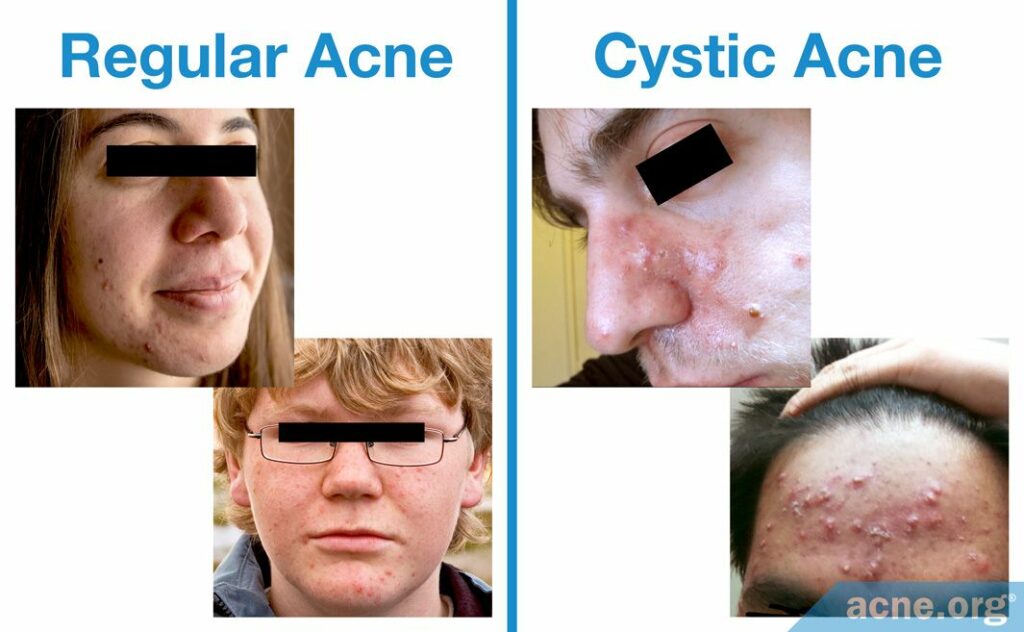
Regular Acne: Regular acne consists of run-of-the-mill pimples that are relatively small, often red, and that sometimes develop a white or yellow center.
Cystic Acne: Cystic acne is a more severe form of acne that comes with large (over 5 mm in diameter), often painful lesions called nodules and/or cysts.
Treatment of Regular Acne: Topical medications like benzoyl peroxide and/or retinoids (tretinoin, adapalene, tazarotene) can help most people with regular acne get it under control. Hormonal treatments for females are also an option.
Treatment of Cystic Acne: Properly applied benzoyl peroxide can often get even cystic acne under control. However, when cystic acne is extremely severe and scarring, oral isotretinoin (Accutane) is a “nuclear option” that is effective but comes with potentially lifelong side effects. For females, hormonal treatments can also help get cystic acne under control in many cases.

The Science
Both regular and cystic acne (also called nodulocystic acne) develop mostly on the face, neck, upper chest, back and shoulders. Acne lesions occur when skin pores become clogged and skin oil, called sebum, gets trapped inside.
The difference between regular and cystic acne comes down to the types of lesions:
Regular acne: Regular acne consists of relatively small whiteheads, blackheads, papules, and pustules. While regular acne can sometimes scar and can cause deep emotional distress, all of the lesions in regular acne tend to come and go relatively quickly, within weeks.
Cystic acne: Cystic acne can also come with all of the lesions of regular acne, and usually does, at an even higher number than seen in regular acne. But what makes cystic acne unique is that it also comes with nodules and/or cysts, which are larger (over 5 mm), often painful lesions that can last for months or even longer, and frequently scar.
Expand to read about rare, severe cystic acne
Severe cystic acne (rare): In rare cases, a person may develop a particularly severe form of cystic acne such as acne conglobata or acne fulminans. Acne conglobata features abscesses (buildup of pus under the skin) and so-called draining sinuses, which are cysts that have merged together, in addition to the other types of lesions seen in cystic acne. In acne fulminans, nodules and cysts fill with blood and turn into ulcers.1,2
Regardless of the type or severity of acne, the same factors lead to all acne lesions:
- Excess skin oil (sebum) production, which is controlled by male hormones present in both males and females
- The release of inflammatory molecules in the skin
- An overgrowth of skin cells (keratinocytes) and an increase in keratin, a sticky protein that makes up these cells
- An overgrowth of acne bacteria (C. acnes) in the pore
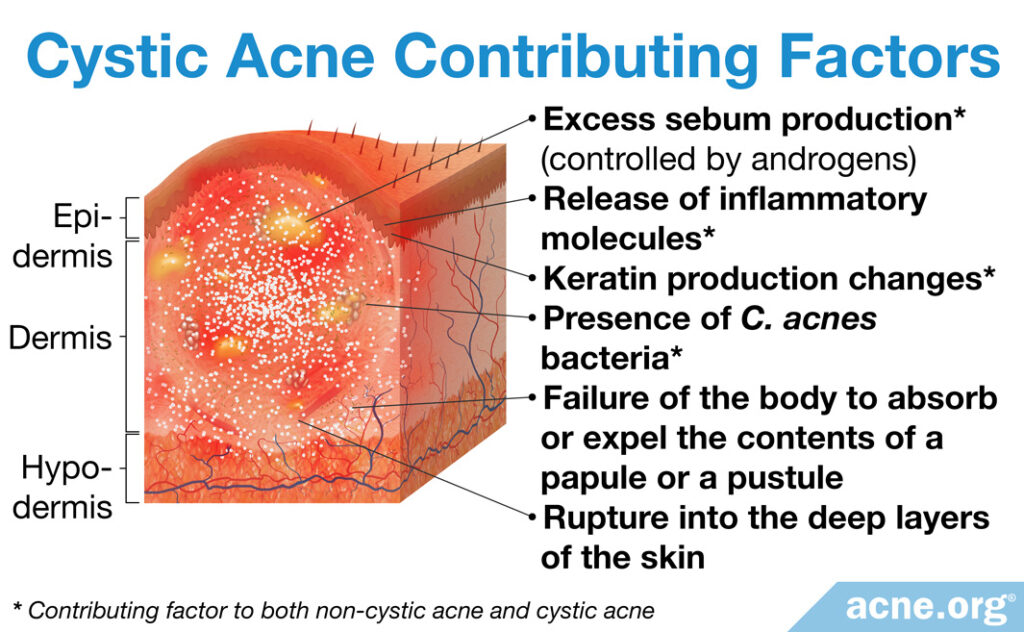
How some regular acne lesions become cystic acne lesions
All acne lesions start the same way, with a clogged pore.
Skin oil (sebum) inside the clogged pore starts to build up and either a whitehead, which looks like a very small white dot on the skin, or a blackhead, which looks like a black or brown dot on the skin, develops.
A whitehead or blackhead can heal on its own and go away. However, sometimes the buildup inside the pore becomes too much for the walls of the pore to handle and the pore walls break. This leads to the development of inflamed, red pimples, that can fill up with pus and get a white or yellow center3, what someone might refer to as a “zit” or “pimple.” Normally, pimples heal on their own when the body either absorbs their contents or the contents drain to the surface of the skin.4
However, sometimes a whitehead or blackhead completely explodes deep in the skin. This causes the body to overreact, producing a large, inflammatory reaction. When a whitehead or blackhead explodes severely like this, it usually produces the cystic acne lesion called a nodule, which are fibrous lesions that do not contain pus. The body will normally heal a nodule over time, however sometimes the area becomes encapsulated and fills with pus, creating a cyst.
Both nodules and cysts often cause scarring because the pore as well as surrounding pores and skin structure can be completely destroyed.4,5,6
Male hormones are to blame
Androgens, which are male hormones that are found in both males and females, are at the root of both regular and cystic acne. The higher the androgen level, normally, the more severe acne can become. People with cystic acne tend to have high levels of androgens compared to people with regular acne, and especially compared to people with no acne.
Incidence, Gender, Genetics, and Race
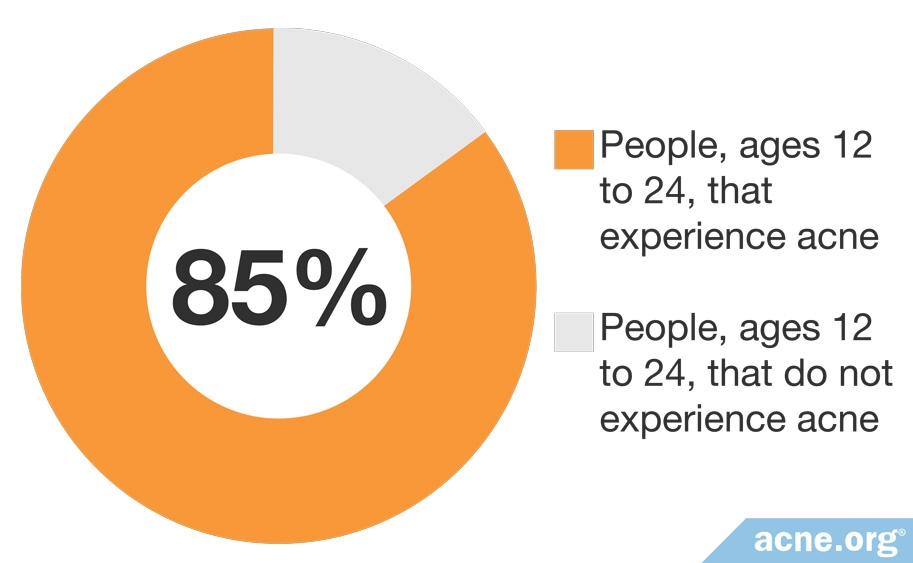
U.S. Census data showed that around 85% of people between 12 and 24 years old suffer from either regular or cystic acne at some point. The incidence decreases as people get older. Both males and females can develop both regular and cystic acne, but, as a whole, males tend to experience more cystic acne.7,8
As we can see in the following article published in 2013 in the British Journal of Dermatology, genetics also plays a part:

Research has also revealed a genetic link in the development and severity of acne. “Acne occurs earlier and is more severe in those with a positive family history. Several retrospective twin studies have found a possible genetic basis with familial clustering.” Based on the limited research we have thus far regarding ethnicity, the incidence of nodulocystic acne is also higher in Caucasians and Hispanics than in people of African descent.7
Treatment of Regular vs. Cystic Acne
Regular acne can be kept under control with proper topical treatment.
Cystic acne can also sometimes be kept under control through proper topical treatment. However, when nodules and cysts are widespread and actively scarring, it sometimes requires more aggressive treatment. Isotretinoin (Accutane) is the most reliable therapy for widespread and scarring cystic acne.9
Authors writing for the Journal of the German Society of Dermatology state:

“The multiple modes of action for isotretinoin…make this compound the single most effective in the treatment of severe recalcitrant nodulocystic acne, and in the prevention of acne scarring.”10
Isotretinoin acts on various levels, addressing all four factors which contribute to the development of acne. Specifically, isotretinoin can help with acne by:
- Reducing the size of skin oil glands and thus decreasing skin oil production
- Relieving acne-related inflammation
- Inhibiting the overgrowth of skin cells
- Reducing the overgrowth of acne bacteria in skin pores11,12
The following 2011 study published in the Clinical Evidence shows the power of isotretinoin:
After 20 weeks of treatment with isotretinoin, acne was eliminated in 85% of patients.3
Isotretinoin side effects
Because of its side effects, doctors usually only prescribe isotretinoin for severe cystic acne or acne which does not respond to other treatments. You should understand the side effects before taking isotretinoin so that you can make an informed decision. Most of the side effects are reversible, but some can be severe and long term. Isotretinoin is an oral medication that affects the entire body and can change it permanently in unexpected ways. Side effects include, but are not limited to, dry skin and mucous membranes, joint pain, changes in vision, raised levels of cholesterol and liver enzymes, and an extremely high potential for severe birth defects when taken by pregnant women.6
Treatment to reduce androgen levels
When blood tests confirm abnormally high levels of androgens, treatment that reduces androgen levels, such as oral contraceptives, or anti-androgen medications like spironolactone or cyproterone acetate, are sometimes an effective option for females with cystic acne. These treatments are not normally not prescribed to males because they can create feminizing symptoms, like enlarged breasts.

In a study investigating oral contraceptive and anti-androgen treatment, severe acne cleared or showed a marked improvement in 97% of women…after six months.14
In severe cases of acne in females, treatment to reduce androgen levels may be added to isotretinoin treatment. As we see in the following study published in 2013 in the International Journal of Dermatology:
Researchers found that treatment with isotretinoin and anti-androgen therapy cleared acne completely in 91% of cases. In cases where this combined treatment only partly cleared the acne lesions, it was mostly in women with Polycystic Ovary Syndrome (PCOS), a condition that is characterized by excessive androgens.13
Anti-androgens are corticosteroid drugs, which have a range of side effects that should be considered even though the dosage needed to treat acne is relatively low.8 Oral corticosteroids are also on the World Anti-Doping Agency list of banned substances in competitive sport. You should discuss this with your doctor if you are a serious competitor because you must avoid oral corticosteroids for at least a week leading up to a competition.14
References
- Hafsi, W. & Badri, T. Acne Conglobata. In: StatPearls. Treasure Island (FL): StatPearls Publishing; July 17, 2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459219/
- Zito, P. M. & Badri, T. Acne Fulminans. [Updated 2020 Jul 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459326/
- Purdy, S. & DeBerker, D. Acne vulgaris. BMJ Clin. Evid. 2011. pii: 1714 (2011). https://www.ncbi.nlm.nih.gov/pubmed/21477388
- White, G. M. Recent findings in the epidemiologic evidence, classification, and subtypes of acne vulgaris. J. Am. Acad. Dermatol. 39, S34-S37 (1998). https://www.ncbi.nlm.nih.gov/pubmed/9703121
- Toyoda, M. & Morohashi, M. Pathogenesis of acne. Med. Electron Microsc. 34, 29-40 (2001). https://www.ncbi.nlm.nih.gov/pubmed/11479771
- Robertson, K. M. Acne vulgaris. Facial Plast. Surg. Clin. North Am. 12, 347-55 (2004). https://www.ncbi.nlm.nih.gov/pubmed/15261171
- Bhate, K. & Williams, H. C. Epidemiology of acne vulgaris. Br. J. Dermatol. 168, 474-485 (2013). https://www.ncbi.nlm.nih.gov/pubmed/23210645
- Marynick, S. P., Chakmakjian, Z. H., McCaffree, D. L. & Herndon, J. H. Jr. Androgen excess in cystic acne. N. Engl. J. Med. 308, 981-986 (1983). https://www.ncbi.nlm.nih.gov/pubmed/6220224
- Whitney, K. M. & Ditre, C. M. Management strategies for acne vulgaris. Clin. Cosmet. Investig. Dermatol. 4, 41-53 (2011). https://www.ncbi.nlm.nih.gov/pubmed/21691566
- Ganceviciene, R. & Zouboulis, C. C. Isotretinoin: state of the art treatment for acne vulgaris. J. Dtsch. Dermatol. Ges. 8, S47-S59 (2010). https://www.ncbi.nlm.nih.gov/pubmed/20482692
- Khalil, N. Y., Darwish, I. A. & Al-Qahtani, A. A. Isotretinoin. Profiles Drug Subst. Excip. Relat. Methodol. 45, 119-157 (2020). https://pubmed.ncbi.nlm.nih.gov/32164966/
- Abdelmaksoud, A., Lotti, T., Anadolu, R., Goldust, M., Ayhan, E., Dave, D. D., Vestita, M., Ebik, B. & Gupta, M. Low dose of isotretinoin: A comprehensive review. Dermatol. Ther. 33, e13251 (2020). https://pubmed.ncbi.nlm.nih.gov/32022958/
- Cakir, G. A., Erdogan, F. G. & Gurler, A. Isotretinoin treatment in nodulocystic acne with and without polycystic ovary syndrome: efficacy and determinants of relapse. Int. J. Dermatol. 52, 371-376 (2013). https://www.ncbi.nlm.nih.gov/pubmed/22998438
- Bruckner, P. & Nicol, A. Use of oral corticosteroids in sports medicine. Curr. Sports Med. Rep. 3,181-183 (2004). https://www.ncbi.nlm.nih.gov/pubmed/15231220
 Acne.org Products
Acne.org Products