Yes, Isotretinoin Is Overprescribed. The Decision to Take It Should Be Made Only After Careful Consideration.

The Essential Info
The current medical research shows that isotretinoin (Accutane®), while extremely effective for severe acne, is overprescribed for the treatment of mild-to-moderate acne.
Isotretinoin is an oral medication that affects the entire body, changing not only the skin, but also potentially other parts of the body, forever.
Due to the severe side effects and high relapse rates of isotretinoin therapy, it becomes clear that doctors should be vigilant and careful when prescribing it.
Be Your Own Advocate: You only get one body. If you have severe, widespread, and scarring acne, isotretinoin may be an important option for you to consider. But if you suffer from less severe acne, make sure you exhaust other options before you take a medication that will change your body forever.
My Experience: I took isotretinoin in college when I had severe and widespread acne on my face and body. To his credit, my doctor followed accepted prescription guidelines. Even though I met the criteria for severe acne, he made sure to exhaust all other options first, and only prescribed isotretinoin to me after all other available options failed to help clear me up. Since taking isotretinoin, I have never completely gone back to “normal,” and still have to use lip balm multiple times a day. I also suspect, but cannot prove, that my joints may have suffered lifelong damage. If I could go back and do it over again, I would probably take it again because I had such severe acne, but I would caution anyone with less severe acne to be extremely cautious.

The Science
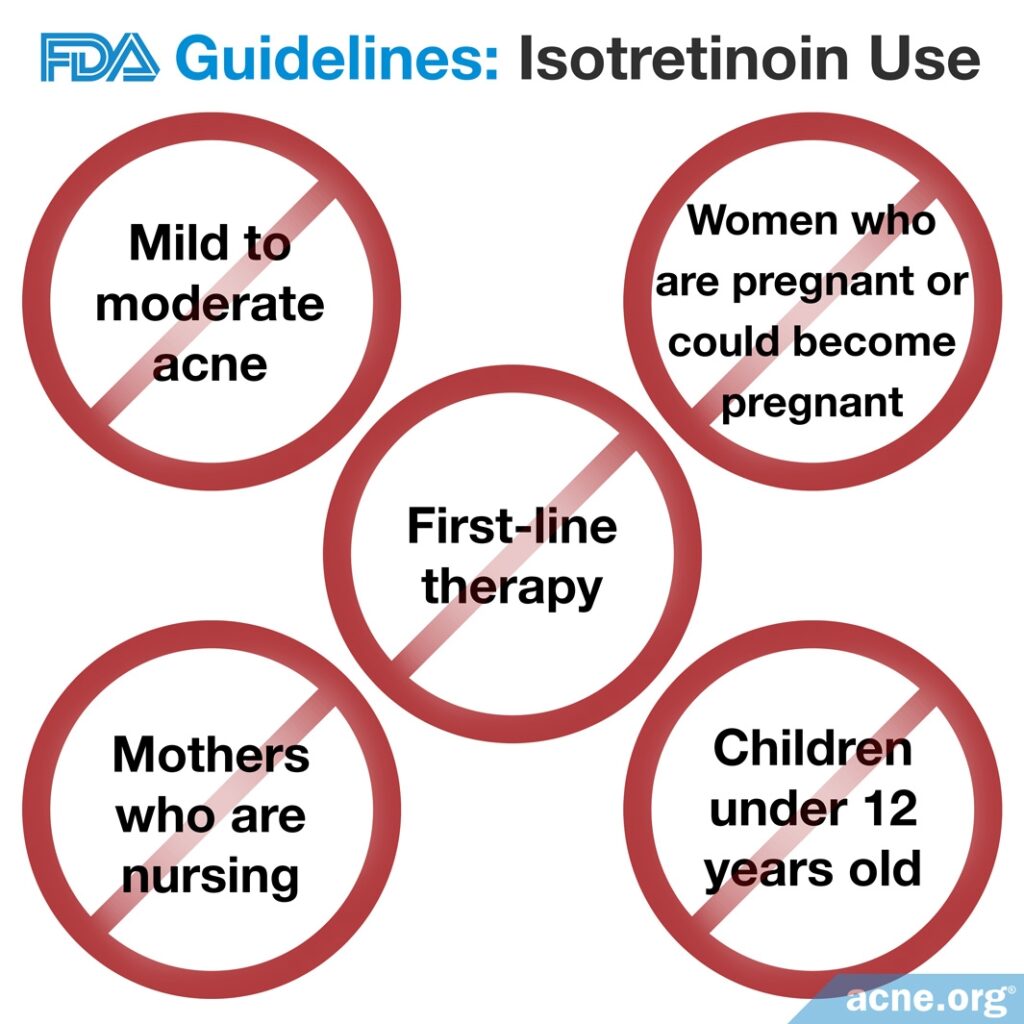
- The FDA Sets Strict Guidelines for the Prescription of Isotretinoin
- Against Recommendations, Doctors Sometimes Prescribe Isotretinoin for Mild-to-Moderate Acne
- High Relapse Rates
- The Bottom Line: Doctors Overprescribe Isotretinoin
Isotretinoin is an oral medication derived from Vitamin A that is normally used to treat severe nodular and cystic acne. Isotretinoin is taken orally once a day, normally for 15 – 20 weeks, with a meal that contains an adequate amount of dietary fat to aid in absorption.
Even though isotretinoin is effective1,2, it can come with severe and potentially long-lasting side effects. Because of these side effects, the FDA developed strict conditions under which doctors should prescribe the drug, and these conditions have become ever more rigorous over time as the severity of isotretinoin side effects come to light.
In spite of these guidelines, research regarding the prescription of isotretinoin shows that it is often prescribed to patients that do not meet these strict conditions.
The FDA Sets Strict Guidelines for the Prescription of Isotretinoin
Currently the FDA is responsible for establishing and implementing guidelines controlling isotretinoin prescription, but physicians can prescribe any drug as they see fit regardless of these official guidelines.
The current guidelines state that:
- Isotretinoin should only be used to treat severe acne that has not responded to at least one previous six to eight week treatment course of another acne therapy.3-5
- Isotretinoin should not be used to treat mild-to-moderate acne.4-5
- Isotretinoin should never be prescribed as a first line of therapy.4-5
- Isotretinoin should never be offered to children under the age of 12.2,5
- Chemical peeling treatments should be avoided during and six months following isotretinoin treatment.5
- The beginning dosage of isotretinoin should be 0.5 mg per kg of body weight (0.5 mg per 2.2 pounds).4-5
Against Recommendations, Doctors Sometimes Prescribe Isotretinoin for Mild-to-Moderate Acne
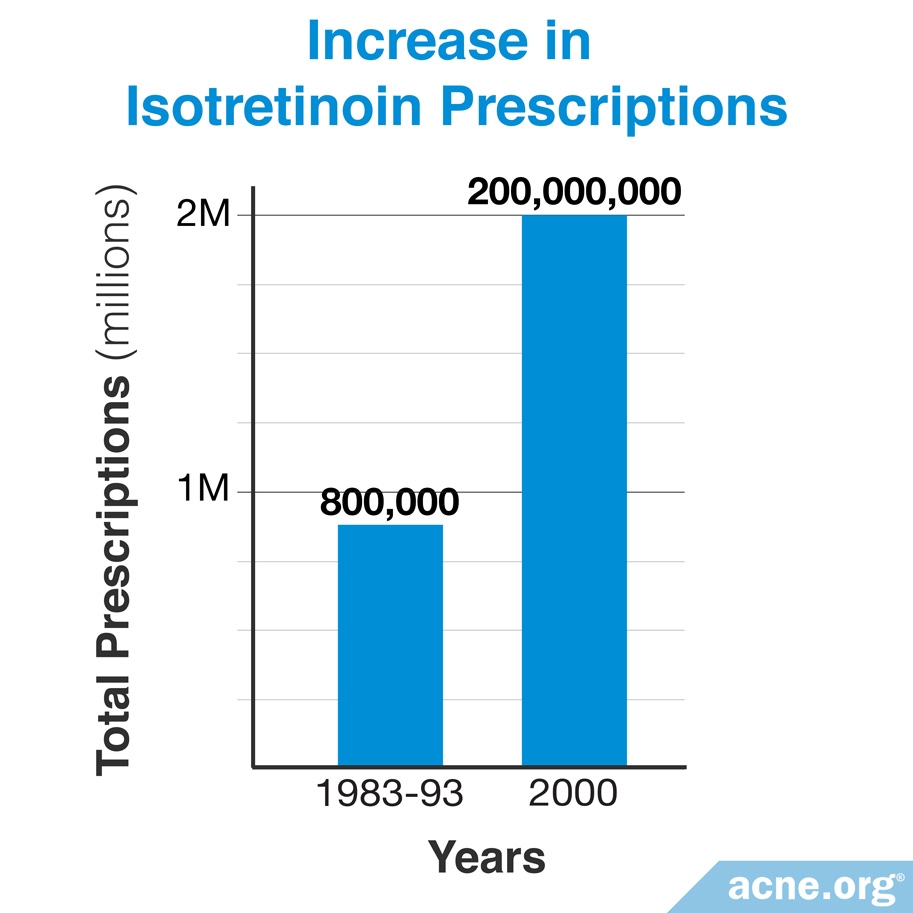
Istoretinoin hit the market in 1982. Despite increased FDA restrictions, prescriptions for isotretinoin have dramatically increased over the past 30+ years.
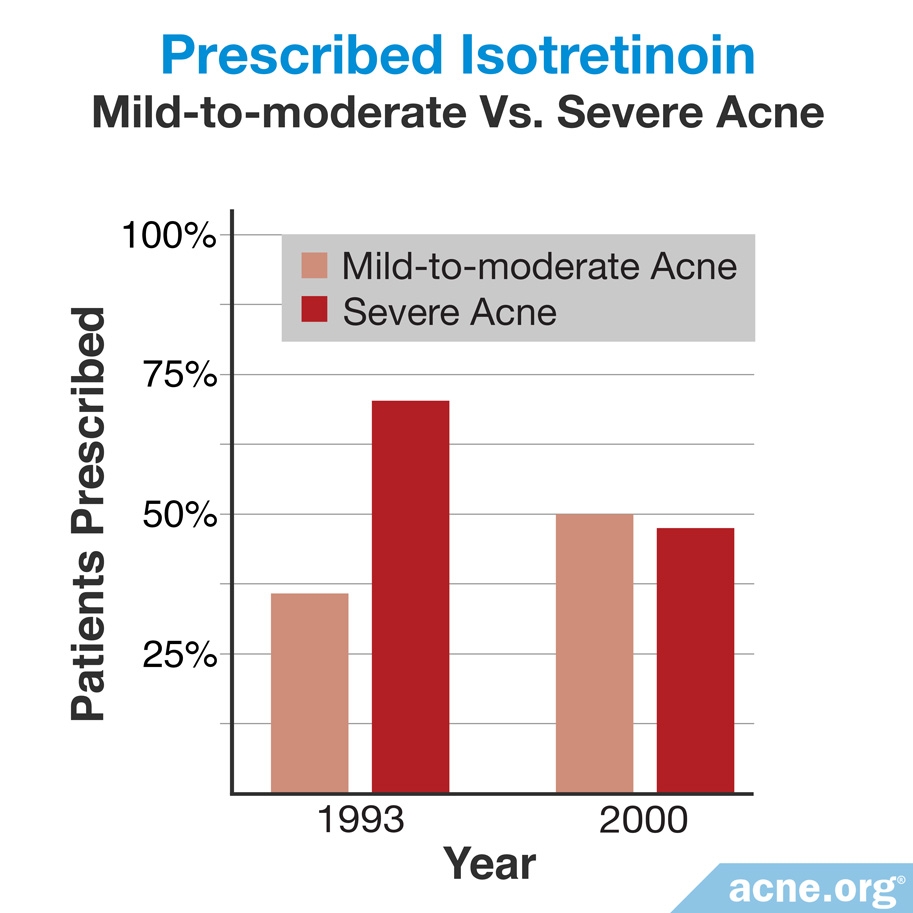
The last study examining the number of provided prescriptions in the U.S. looked at the years between 1982 and 2000, and found a dramatic uptick in the number of prescriptions written during this period. The researchers noted that this increase was due to more doctors prescribing isotretinoin for mild-to-moderate acne. Isotretinoin prescriptions for severe acne actually decreased during this period.6
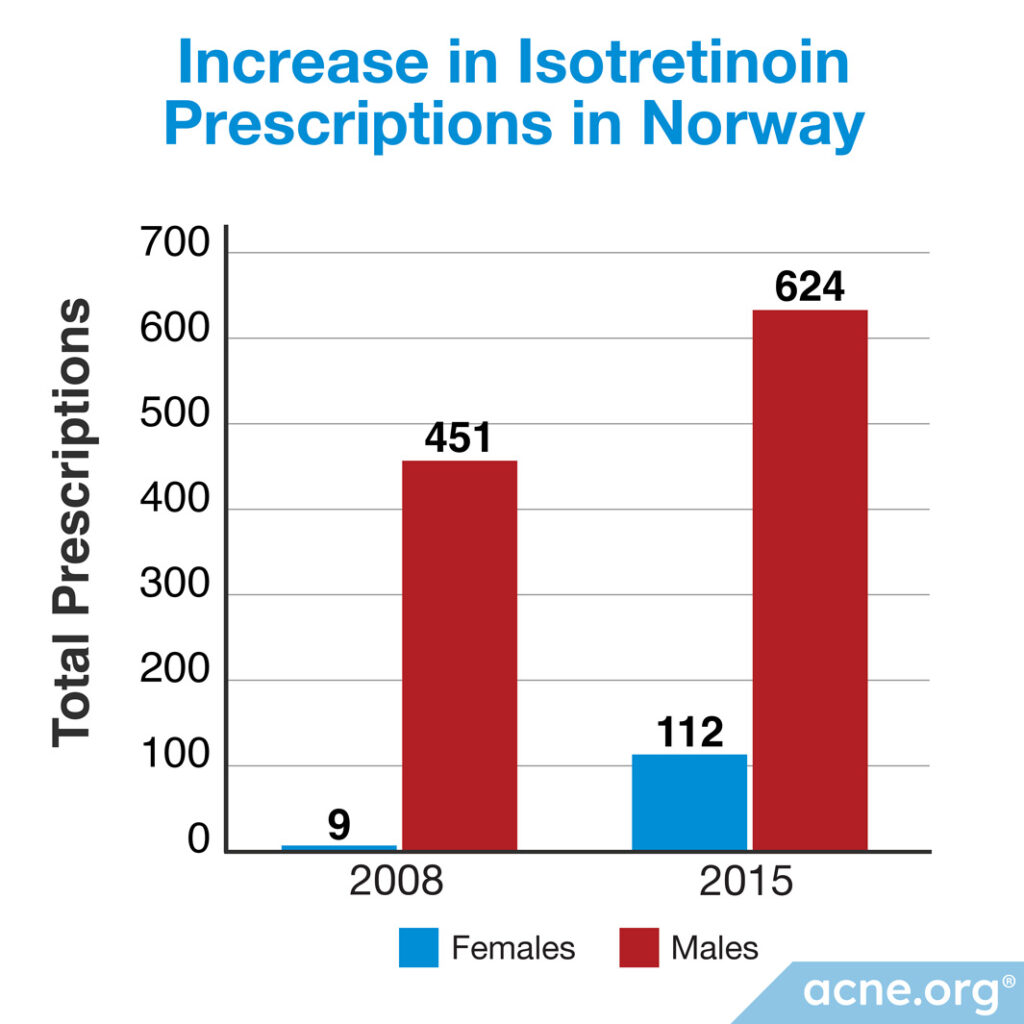
Another study conducted in Norway looked at the prescribing pattern of isotretinoin for the treatment of acne in young adult patients over a period of 11 years. The researchers found a startling increase in isotretinoin prescriptions from 2005 to 2015. Over that period, doctors in Norway started prescribing isotretinoin 10 times more to women and 3 times more to men.7
Expand to read details of U.S. study

The most recent study looking at prescription rates of isotretinoin in the United States was published in the Journal of the American Academy of Dermatology in 2002. While providers prescribed an average of 800,000 isotretinoin prescriptions per year between 1983 and 1993, by 2000 providers were writing nearly 2 million prescriptions per year, amounting to a 250% increase compared with 1983.6 The researchers attributed this increase with physicians using isotretinoin to treat mild-to-moderate acne, which rose from 31% in 1993 to 49% in 2000. While isotretinoin prescriptions for mild-to-moderate acne increased, the total prescriptions for severe acne decreased from 63% to 46%. Therefore, researchers attributed the 250% increase in total isotretinoin prescriptions to the treatment of mild-to-moderate acne and not for severe acne as the current regulatory guidelines advise.6
Expand to read details of Norwegian study
The study looking at prescription rates of isotretinoin in Norway was published in the Journal of Antimicrobial Chemotherapy in 2017. According to the Norwegian Prescription Database, isotretinoin was prescribed to only 9 females between the ages of 14 and 24 years old in 2008, compared to 112 females in that age group in 2015. Among male patients, 451 received prescriptions for isotretinoin in 2008, compared to 624 in 2015. The scientists concluded that the trend from 2008 to 2015 was toward prescribing more isotretinoin. Moreover, compared to a few years earlier in 2005, the prescription rate for isotretinoin in 2015 had increased 10-fold for females and 3-fold for males.7
High Relapse Rates
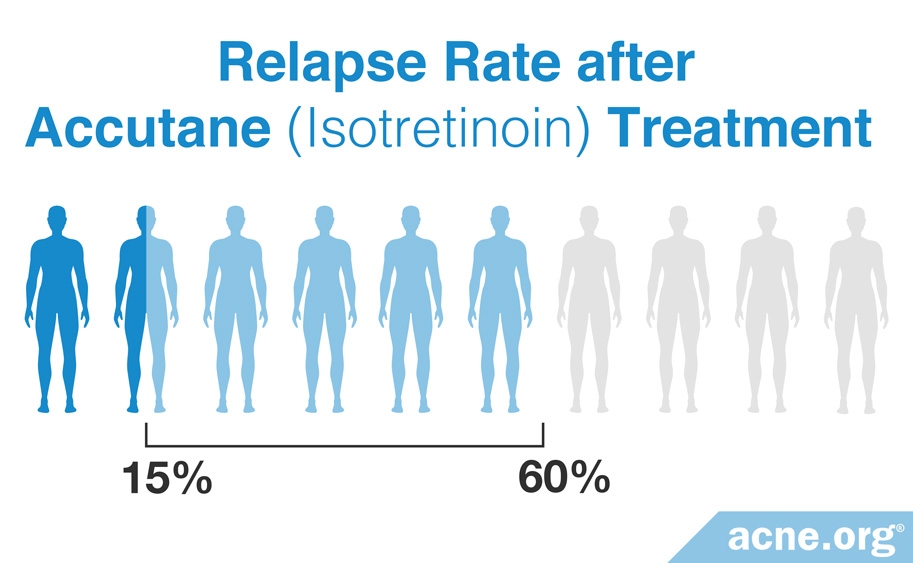
There is further controversy over the increased prescribing of isotretinoin due to its potential for limited long-term effectiveness, especially in people with more severe acne and in males.2 The idea of the isotretinoin achieving a cure can be misleading. The relapse rate after a course of isotretinoin therapy can be anywhere between 15 – 60% depending on the severity of acne, duration of treatment, and dosage provided.8 Acne relapses usually occur somewhere between 6 and 10 months after stopping isotretinoin treatment.9,10
Scientists believe that relapses are underreported and thus the true relapse rate is higher than patients and doctors may believe. For example, some people with severe acne may overlook a few small blemishes following isotretinoin treatment because these spots are considered insignificant and therefore patients do not report this renewed, yet lesser, outbreak as a relapse.2
The Bottom Line: Doctors Overprescribe Isotretinoin
The current research indicates that isotretinoin, while extremely effective, is overprescribed for the treatment of mild-to-moderate acne.11,12 Upon examining the severe side effects and potential for relapse, it becomes clear that doctors should take care in closely following the restrictive guidelines regarding prescription.
In order to receive the best therapy course for your acne type, it is crucial to discuss all available treatment options with a medical professional. Finally, it is always important to speak openly with your doctor regarding the severity of your acne, risks, side effects, and alternatives when considering a course of isotretinoin therapy. Research suggests that doctors sometimes fail to discuss the serious side effects of isotretinoin with their patients because of time constraints during medical appointments.13 Be your own advocate and make sure to ask about any concerns you have.
References
- Katsambas, A. & Papakonstantinou, A. Acne: systemic treatment. Clin. Dermatol. 22, 412-418 (2004). https://www.ncbi.nlm.nih.gov/pubmed/15556728
- Layton, A. The use of isotretinoin in acne. Dermatoendocrinol. 1, 162-169 (2009). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2835909/
- Goldsmith, L. A. et al. American Academy of Dermatology Consensus Conference on the safe and optimal use of isotretinoin: summary and recommendations. J. Am. Acad. Dermatol. 50, 900-906 (2004). https://www.ncbi.nlm.nih.gov/pubmed/15153892
- Goh, C. L. et al. South-East Asia study alliance guidelines on the management of acne vulgaris in South-East Asian patients. J. Dermatol. 42, 945-953 (2015). https://www.ncbi.nlm.nih.gov/pubmed/26211507
- Layton, A. M., Dreno, B., Gollnick, H. P. & Zouboulis, C. C. A review of the European Directive for prescribing systemic isotretinoin for acne vulgaris. J. Eur. Acad. Dermatol. Venereol. 20, 773-776 (2006). https://www.ncbi.nlm.nih.gov/pubmed/16898895
- Wysowski, D. K., Swann, J. & Vega, A. Use of isotretinoin (Accutane) in the United States: rapid increase from 1992 through 2000. Journal of the Am. Acad. Dermatol. 46, 505-509 (2002). https://www.ncbi.nlm.nih.gov/pubmed/11907498
- Odsbu, I., Selmer, R., Stålsby Lundborg, C., Blix, H. S. Increased prescribing of systemic tetracyclines and isotretinoin for treatment of acne. J. Antimicrob. Chemother. 72, 1510-1515 (2017). https://pubmed.ncbi.nlm.nih.gov/28158436/
- Morales-Cardona, C. & Sánchez-Vanegas, G. Acne relapse rate and predictors of relapse following treatment with oral isotretinoin. Actas Dermosifiliogr. 104, 61-66 (2013). https://www.ncbi.nlm.nih.gov/pubmed/22795452
- Kassem, B., Ismail, M. & Hassan, F. Evaluation of the efficacy and relapse rates of treatment protocols for moderate acne using isotretinoin based on the global acne grading system: Randomized, controlled, comparative study. Dermatol. Ther. 35, e15974 (2022). https://pubmed.ncbi.nlm.nih.gov/36346039/
- Demirci Saadet, E. Investigation of relapse rate and factors affecting relapse after oral isotretinoin treatment in patients with acne vulgaris. Dermatol. Ther. 34, e15109 (2021). https://pubmed.ncbi.nlm.nih.gov/34431590/
- Evaristo, L. S. B. F. & Bagatin, E. Use of oral isotretinoin to treat acne in the public system: a hospital-based retrospective cohort. Sao Paulo Med J 137, 363-368 (2019). https://pubmed.ncbi.nlm.nih.gov/31691769/
- O’Donnell, J. Overview of existing research and information linking isotretinoin (accutane), depression, psychosis, and suicide. Am J Ther 10, 148-159 (2003). https://pubmed.ncbi.nlm.nih.gov/12629595/
- Kokandi AA. Trends and opinion of isotretinoin use for acne treatment by dermatologists in western area of Saudi Arabia: A cross-sectional survey. Int Arch BioMed Clin Res 3, 10-15 (2017). https://iabcr.org/index.php/iabcr/article/view/44
 Acne.org Products
Acne.org Products