Preliminary Studies Say Yes, but Using These Drugs Is Risky, so They Are Reserved for Very Severe Cases of Acne

The Essential Info
Drugs that treat auto-immune diseases (i.e. rheumatoid arthritis or psoriasis) work by reducing inflammation in the body. Since acne is at its core an inflammatory disease, they may also help reduce acne, and initial studies have shown they are effective.
However, since these drugs work by repressing the immune system, that means the likelihood of getting a severe infection increases when taking them. For this reason, doctors do not regularly prescribe them for acne, and when they are prescribed, it is normally only for very severe cases.
___
Examples of so-called small molecule auto-immune drugs, which are taken orally:
(research shows they may reduce acne to a modest degree)
- Otezla® (apremilast)
- Zyflo CR® (zileuton)
Examples of so-called biosimilar auto-immune drugs, which are injected:
(research shows they may completely eradicate acne)
- Humira® (adalimumab)
- Enbrel® (etanercept)
- Remicade® (infliximab)

The Science
- How Do Auto-immune Drugs Counteract Acne?
- What Is the Evidence for the Effectiveness of Auto-immune Drugs for Acne?
- Side Effects and Risks: Why Auto-Immune Drugs Are Not Often Used in the Treatment of Acne
- Conclusion
Auto-immune diseases, such as rheumatoid arthritis and psoriasis, occur when the body’s immune system confuses certain body cells for “foreign invaders” and attacks itself. Drugs that treat auto-immune disorders work by inhibiting the immune system so it is less able to attack.
So why would this be of interest to us when it comes to acne? Because when the immune system gets confused and attacks the body, one hallmark of this immune response is inflammation. Inflammation is the redness, pain, swelling, and heat that often accompany disease or injury.1-3 Since acne is at its core an inflammatory disease, it stands to reason that drugs that decrease the immune response and inflammation could also treat acne.
As we will see, it appears these drugs do in fact work to help clear acne, and in some cases completely eradicate acne, but their side effects relegate them to only the most severe cases.
How Do Auto-immune Drugs Counteract Acne?
Drugs intended for use against auto-immune diseases function by blocking key enzymes in the immune system and preventing the immune response. By achieving this, these drugs also prevent inflammation.
There are two major types of drugs for auto-immune diseases:
- Small molecule drugs such as: Otezla® (apremilast), Zyflo CR® (zileuton)
- Biosimilar drugs such as: Humira® (adalimumab), Enbrel® (etanercept), Remicade® (infliximab)
Expand to Learn How These Drugs Work in the Body
Small molecule drugs
These typically function by binding to an enzyme involved in the immune response, thus preventing the enzyme from binding to its normal receptor on immune cells. One example is the drug Otezla® (apremilast). This drug blocks the enzyme phosphodiesterase-4 (PDE4), which is necessary for formation of proteins called cytokines that trigger inflammation. Because of this process, the inflammatory response becomes repressed when PDE4 is blocked.4
Another example of a small molecule drug is Zyflo CR® (zileuton). This drug inhibits the enzyme 5-lipoxigenase, which is necessary for the synthesis of a pro-inflammatory signaling molecule called leukotriene B4. As with apremilast, zileuton reduces inflammation by disrupting the chemical pathway which creates the proteins that trigger inflammation.
Recent studies show that zileuton is also effective in treating acne because it reduces inflammation. As the authors of a review of studies on zileuton as an acne treatment stated, “The use of anti-inflammatory drugs for the treatment of acne is further supported by recent results indicating a key role for leukotriene B4 (LTB4) in the development of tissue inflammation.”5
The studies mentioned above were conducted on volunteers who suffered from acne. They reported side effects such as heartburn, nausea, and stomach pain. Though these side effects may seem mild, small molecule drugs suppress the entire immune system and therefore leave patients more susceptible to infections.
Biosimilar drugs
The other kind of auto-immune drug is known as biosimilar drugs or artificial antibodies because they mimic the natural antibodies of the immune system. These drugs normally are injected intravenously rather than taken by mouth, as stomach acid would unravel their structure. Three of these biosimilar drugs are being investigated for use in severe acne: Humira® (adalimumab), Enbrel® (etanercept), and Remicade® (infliximab).6
All of the mentioned biosimilar drugs function by binding to tumor necrosis factor α (TNF-α), a protein which can trigger the inflammatory response. This binding blocks a receptor spot on TNF-α. Normally, this receptor spot is used when TNF-α joins to an immune cell and triggers inflammation. However, since the biosimilar drug now has taken this spot, TNF-α no longer has a place to bind to immune cells. Thus, TNF-α cannot activate the inflammatory response in the presence of biosimilar drugs.
Compared to healthy skin, skin afflicted with acne shows higher TNF-α levels. This is not surprising since acne is inflammatory, and TNF-α triggers the inflammatory response. Therefore, researchers consider biosimilar drugs as a potential treatment for acne.
However, using biosimilar drugs that inhibit TNF-α carries potentially serious side effects. One of these side effects is a weakened immune system. Because TNF-α helps the immune system fight off infections, drugs that inhibit it also inhibit the immune system and leave the patient prone to infections. Furthermore, TNF-α plays a role in preventing tumors, and certain tumors have occurred in patients taking drugs that inhibit this protein.
What Is the Evidence for the Effectiveness of Auto-immune Drugs for Acne?
Good evidence for the effectiveness of auto-immune drugs in acne treatment would consist of published studies or clinical trials with hundreds or thousands of acne patients as participants. Unfortunately, there have been no such large studies done. However, several small studies provide some information concerning the effectiveness of auto-immune drugs for acne.
Small molecule drugs: A study of 10 participants was published in 2009 and tested zileuton, a small molecule drug used for auto-immune disorders, on people with acne. After three months of treatment, the severity of the patients’ acne decreased by 41%.7 This suggests that zileuton is at least partially effective against acne.
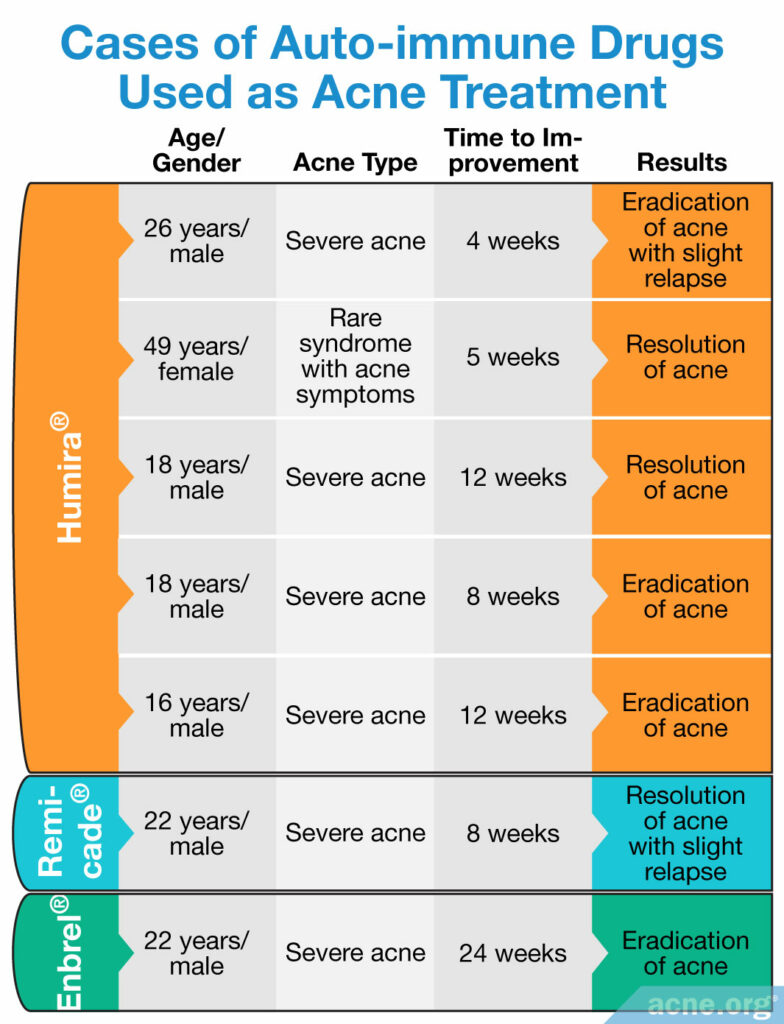
Biosimilar drugs: Because biosimilar drugs come with such serious risks, for safety reasons, no studies that include more than one person at a time have been conducted on biosimilar drugs for acne. However, doctors have administered biosimilar drugs to a few individual patients for the treatment of serious types of acne or rare syndromes often associated with acne, like acne inversa and SAPHO syndrome,8 and reported the results in medical journals. In these cases, the researchers determined that the benefits to these patients outweighed the risks of an inhibited immune system. Below we can see that, at least in these particular individuals with severe acne, biosimilar drugs provided dramatic clearing of the skin.
Expand to read details of studies
Humira®: The first of these cases involved three patients with severe acne treated with the auto-immune medication, Humira® (adalimumab). The usual acne treatments, such as antibiotics and vitamin A derivatives, had failed to help these patients. In all three patients 80 mg of Humira®, followed by 40mg every other week, was injected just under the skin all over the face, rather than intravenously, as is typical with treatment of auto-immune diseases. The first patient, a 26-year-old male with a severe form of acne, experienced an eradication of the majority of his acne after four weeks of treatment. This resolution persisted after 12 weeks of follow-up.9 The next patient, a 49-year-old woman with a rare, serious syndrome that includes acne as a symptom, had improvement in her acne after two weeks. Her acne lesions resolved after five weeks of continuing treatment.10 An 18-year-old male was the third patient. He had suffered from severe acne but showed improvement after four weeks, with resolution of his acne after 12 weeks of treatment.6
Another case involved an 18-year-old male with acne fulminans, a rare form of severe acne. After trying multiple treatments, including topical antibiotics, oral antibiotics, oral Accutane® (isotretinoin), steroid medications, and even antidepressants, the doctor began a new treatment regimen. This consisted of Humira® (adalimumab) in combination with daily oral corticosteroids and antibiotics. As in the three patients above, this patient received injections of Humira® just under the facial skin, starting with 80 mg the first week, followed by 40 mg per week. The inflammatory lesions cleared dramatically, and no new flare-ups occurred for at least six months, which is how long the doctor continued following up. The patient was instructed to stop taking corticosteroids after 2 months, but he continued to receive injections of Humira® every three weeks.11
Finally, another recent case involved a 16-year-old male with severe nodulocystic acne and joint pain. After trying oral Accutane® (isotretinoin) for two weeks, the patient’s symptoms worsened, showing multiple new lesions, new acne scars, and yellow discharge from acne lesions. The patient was instructed to stop taking isotretinoin and prescribed Humira® (adalimumab) together with topical acne medication. Three months later, after 8 doses of Humira®, the patient’s skin was clear with no active acne lesions, acne scars, post-inflammatory hyperpigmentation, or post-acne redness.12
Remicade®: Another case was a 22-year-old man treated with a separate biosimilar drug, Remicade® (infliximab). This patient had severe acne that improved after his first dose. His acne then resolved after the third dose. The young man did experience a minor relapse of his acne clearance four months after his Remicade® treatment, but it was mild and was treated with conventional therapy, without the need for more biosimilar drugs.13
Enbrel®: Finally, the last case was a 22-year-old man who received treatment with another biosimilar drug, Enbrel® (etanercept). He had suffered from severe inflammatory acne and was treated with Enbrel® injected under his skin. After 24 weeks of treatment, his acne was eradicated.14
From these individual cases, it appears that biosimilar drugs are effective in the treatment of acne. However, it bears stating again that these drugs can cause serious side effects and should be reserved for severe cases of acne that do not respond to conventional treatment.
Side Effects and Risks: Why Auto-Immune Drugs Are Not Often Used in the Treatment of Acne
From these impressive study results, it might seem like auto-immune drugs, particularly biosimilar drugs, might be a great resource that people could use to clear up acne. But because immune-suppressing drugs are so good at repressing the immune system, that means anyone taking them is more susceptible to serious infections, and if an infection happens, that infection will be more difficult to treat. Because this is such a concern, doctors do not regularly prescribe auto-immune drugs for acne.
Conclusion
Based on the one small study and several individual cases, both of the two major types of drug for auto-immune disorders, small molecule drugs and biosimilar drugs, show promise in treating acne, with small molecule drugs helping perhaps only partially and biosimilar drugs perhaps producing dramatic clearing of acne. However, more studies of both of these drug types are needed to prove the effectiveness and reliability of auto-immune drugs as an acne therapy.
Caution: Since auto-immune drugs suppress the immune system, treatment with them leaves the patient open to potentially dire infections, particularly in the case of treatment with biosimilar drugs. Therefore, therapy for acne with auto-immune drugs should be considered only in particularly severe acne cases and under the recommendation and supervision of a physician.
References
- Farrar, M. D. & Ingham, E. Acne: inflammation. Clin Dermatol 22, 380 – 384 (2004). https://pubmed.ncbi.nlm.nih.gov/15556722
- Marta Guarna, M., Coulson, R. & Rubinchik, E. Anti-inflammatory activity of cationic peptides: application to the treatment of acne vulgaris. FEMS Microbiol Lett 257, 1 – 6 (2006). https://pubmed.ncbi.nlm.nih.gov/16553825/
- Vowels, B. R., Yang, S. & Leyden, J. J. Induction of pro-inflammatory cytokines by a soluble factor of Propionibacterium acnes: implications for chronic inflammatory acne. Infect Immun 63, 3158 – 3165 (1995). https://pubmed.ncbi.nlm.nih.gov/7542639/
- Gooderham, M. & Papp, K. Apremilast in the Treatment of Psoriasis and Psoriatic Arthritis. Skin Therapy Lett 20 (2015). https://pubmed.ncbi.nlm.nih.gov/26382906/
- Zouboulis, C. C. & Piquero-Martin, J. Update and future of systemic acne treatment. Dermatology 206, 37 – 53 (2003). https://pubmed.ncbi.nlm.nih.gov/12566804/
- Sand, F. L. & Thomsen, S. F. Adalimumab for the treatment of refractory acne conglobata. JAMA Dermatol 149, 1306 – 1307 (2013). https://pubmed.ncbi.nlm.nih.gov/24048280/
- Zouboulis, C. C. Zileuton, a new efficient and safe systemic anti-acne drug. Dermatoendocrinol 1, 188 – 192 (2009). https://pubmed.ncbi.nlm.nih.gov/20436887/
- Włodarek, K., Ponikowska, M., Matusiak, Ł., Szepietowski, J. C. Biologics for hidradenitis suppurativa: an update. Immunotherapy 11, 45-59 (2019). https://pubmed.ncbi.nlm.nih.gov/30702012/
- Yiu, Z. Z., Madan, V. & Griffiths, C. E. Acne conglobata and adalimumab: use of tumour necrosis factor-alpha antagonists in treatment-resistant acne conglobata, and review of the literature. Clin Exp Dermatol 40, 383 – 386 (2015). https://pubmed.ncbi.nlm.nih.gov/25545016/
- Arias-Santiago, S., Sanchez-Cano, D., Callejas-Rubio, J. L., Fernandez-Pugnaire, M. A. & Ortego-Centeno, N. Adalimumab treatment for SAPHO syndrome. Acta Derm Venereol 90, 301 – 302 (2010). https://pubmed.ncbi.nlm.nih.gov/20526553/
- Miguel, D., Tittelbach, J., Elsner, P. A dramatic case of acne fulminans responding to adalimumab. J Dtsch Dermatol Ges Aug;17, 837-838 (2019). https://pubmed.ncbi.nlm.nih.gov/31056852/
- Shahada, O. O. et al. Synovitis, acne, pustulosis, hyperostosis, and osteitis syndrome diagnosis in adolescent and isotretinoin as a possible serious exacerbating factor. Cureus 14, 1-12 (2022). https://pubmed.ncbi.nlm.nih.gov/35371846/
- Schuttelaar, M. L. & Leeman, F. W. Sustained remission of nodular inflammatory acne after treatment with infliximab. Clin Exp Dermatol 36, 670 – 671 (2011). https://pubmed.ncbi.nlm.nih.gov/21595742/
- Campione, E., Mazzotta, A. M., Bianchi, L. & Chimenti, S. Severe acne successfully treated with etanercept. Acta Derm Venereol 86, 256 – 257 (2006). https://pubmed.ncbi.nlm.nih.gov/16710590/
 Acne.org Products
Acne.org Products