Skin on the Body Contains Larger Skin Oil Glands and Can More Easily Develop Severe Acne Lesions

The Essential Info
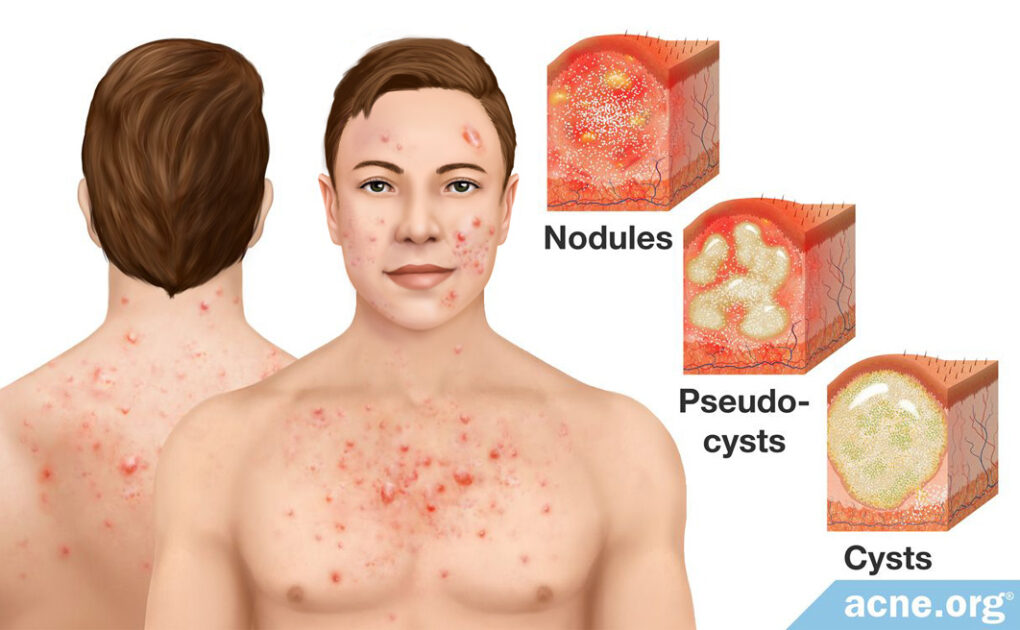
Cystic acne is a severe type of acne that can affect the body and face. The reason it is called “cystic” acne is because it comes with large (over 5 mm in diameter) lesions, such as:
- Nodules (much more common): Firm, fibrous lesions with no pus inside
- Cysts (far less common): Fluid filled lesions that feel “movable” when touched
Cystic acne often appears on the body because the body has larger skin pores and skin oil glands, but can also affect the face. When I say “body” that also includes the back of the neck, a common location for cystic lesions.
Who Gets It: Cystic body acne afflicts teenagers and young adults most frequently. It is more common in males, but females also can battle with it, particularly during the premenstrual window (7-10 days before the onset of menstruation).
Treatment: Recommended treatment for mild-to-moderate cystic body acne normally consists of a properly applied benzoyl peroxide + glycolic acid regimen. For especially severe and widespread cases, isotretinoin (Accutane®) is an option you and your doctor can discuss, but it can come with lifelong side effects. For one or two occasional nodules or cysts that show up on the body, making an appointment with your doctor for a quick cortisone injection can quickly reduce inflammation and speed healing.

The Science
- Who Is Likely to Experience Nodulocystic Acne on the Body?
- Treatment of Nodulocystic Acne on the Body
- Nodulocystic Acne Scarring on the Body
- Rare Forms of Nodulocystic Acne That Affect the Body
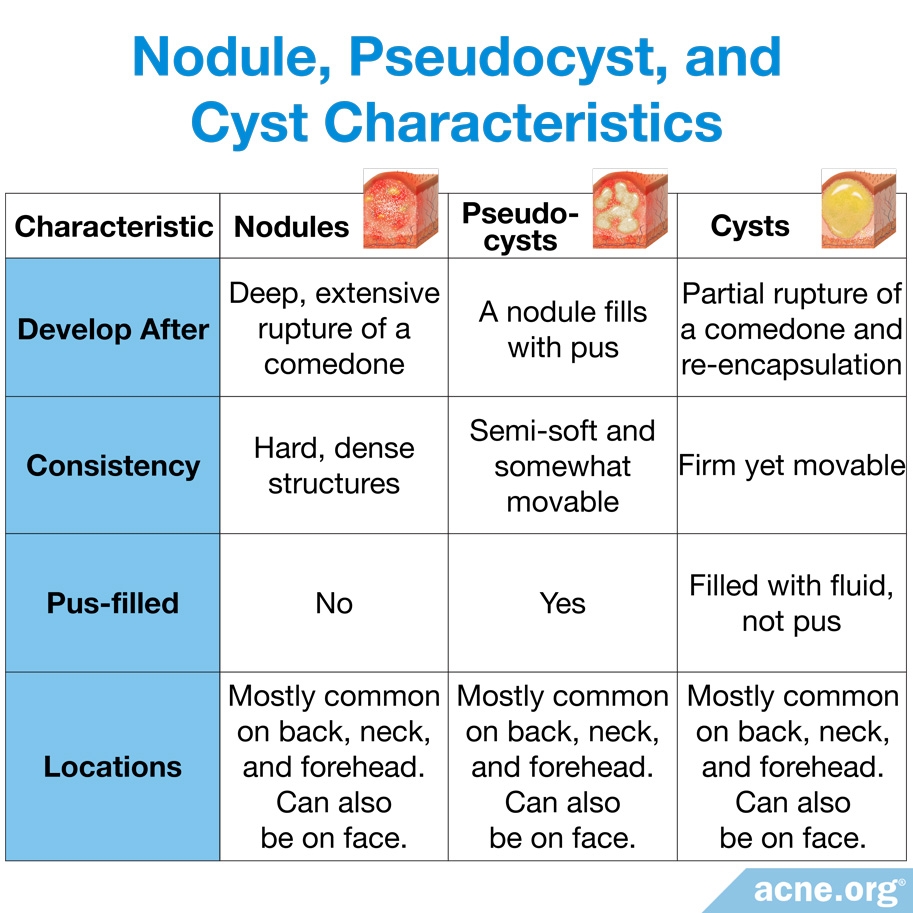
Cystic acne, also known as nodulocystic acne, is a severe form of acne that presents with two types of lesions:
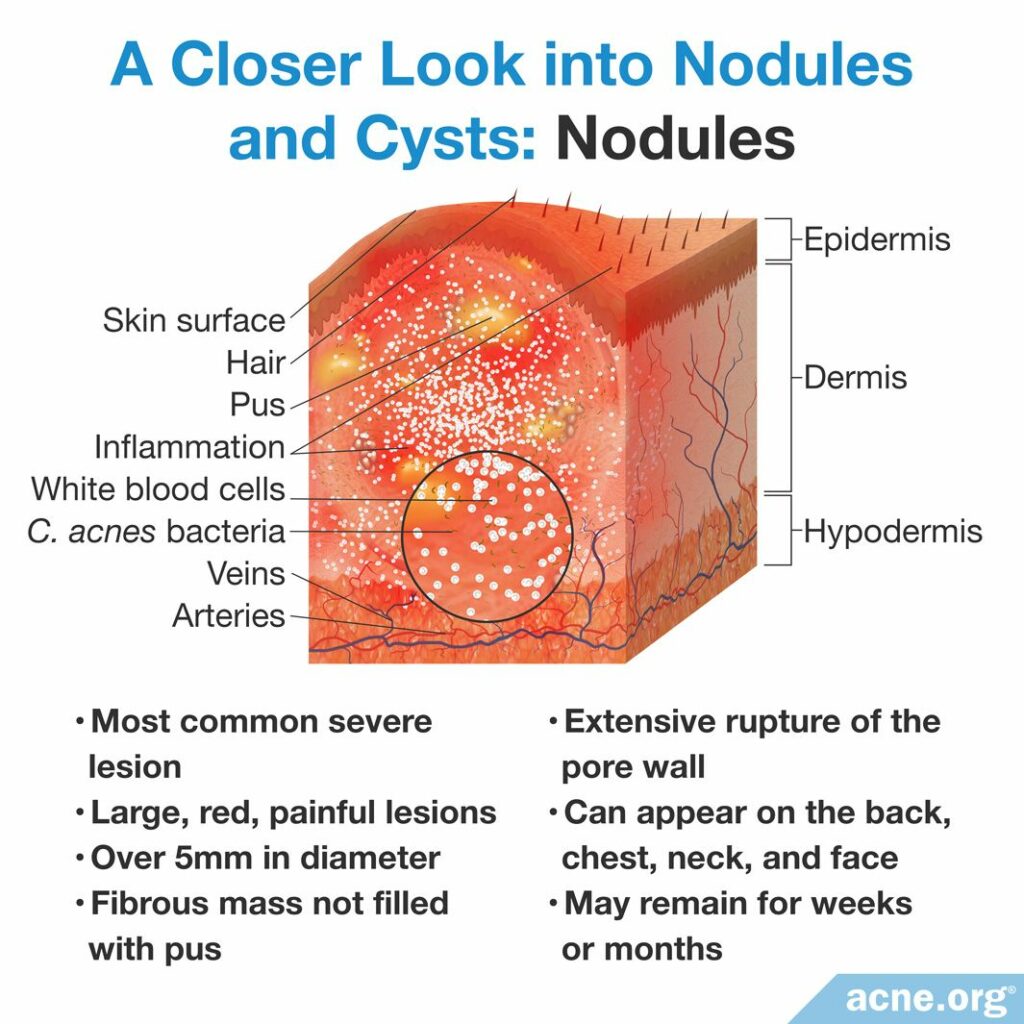
- Nodules: Nodules are by far the most common type of nodulocystic acne lesions. They are large (over 5 millimeters in diameter), red, painful, fibrous bumps that extend deep into the skin and do not contain pus.1 Nodules are stubborn lesions that usually remain on the body for weeks, months, or even longer, and often leave scars behind.
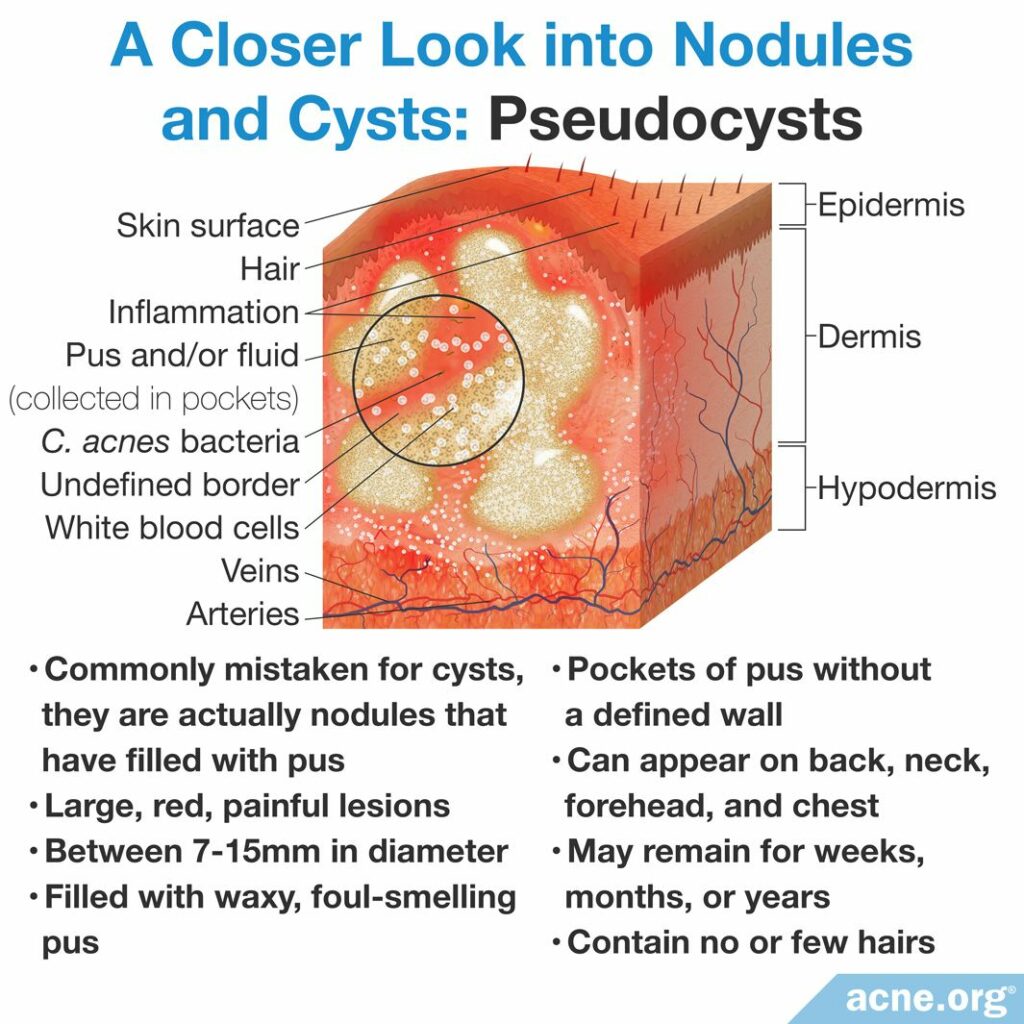
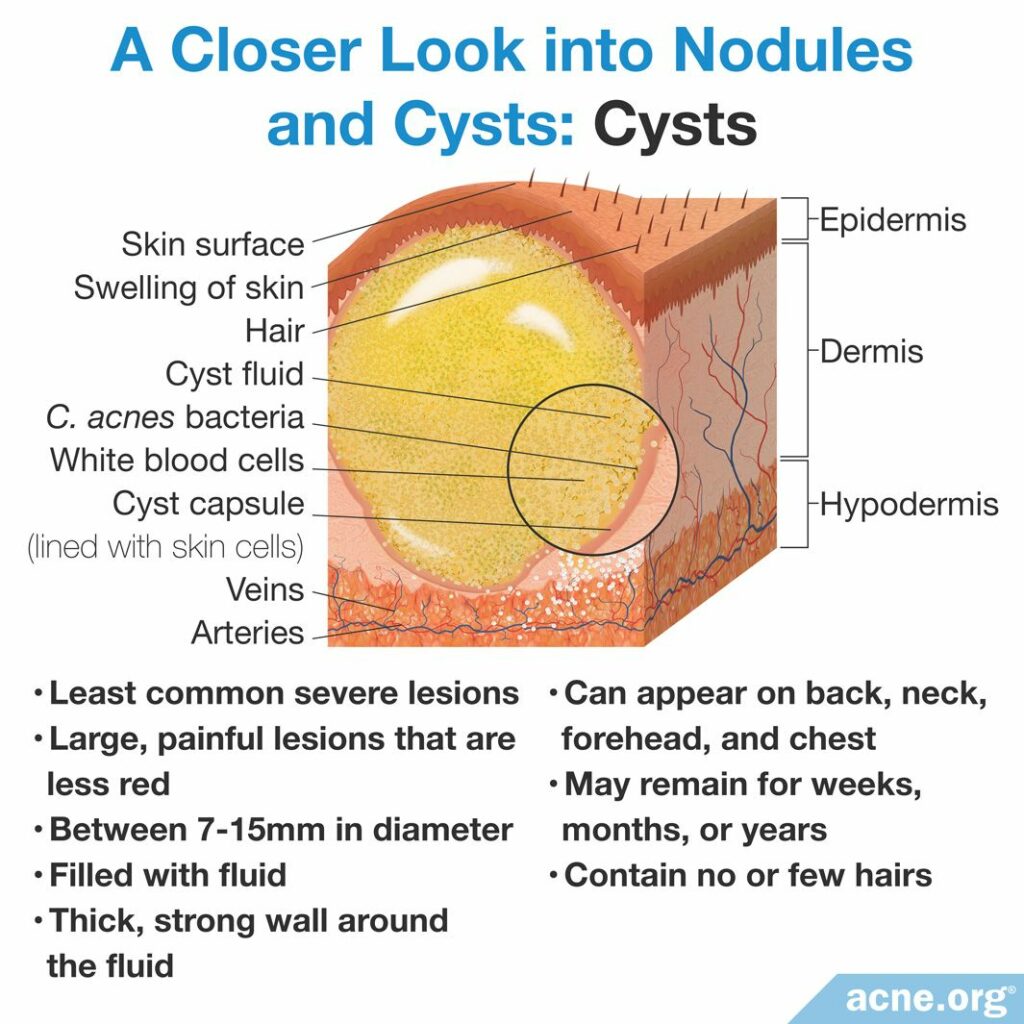
- Cysts: Cysts are large (greater than 5 millimeters but usually between 7 – 15 millimeters), red, painful lumps that extend deep into the skin and, unlike nodules, do contain pus. Cysts are soft lesions and, when touched, the soft liquid/pus inside can be felt moving around. Cysts can sometimes leak to the surface, and contain a cheesy, waxy material with an offending, rotting smell.1,2 They can remain on the skin for months or even years, and often leave scars behind. Note: Most cysts are actually lesions referred to as “pseudocysts,” which are simply nodules that have filled with pus. True cysts are extremely uncommon.
Nodules and cysts appear most often on the back, chest, and/or back of the neck, most likely because the skin-oil-producing glands are bigger on the body compared to the face. However, both types of lesions can also be found on the face, especially on the forehead.
Mild nodulocystic acne comes with just a few nodules and/or cysts. Severe nodulocystic acne comes with many nodules and cysts spread across a large area of skin.3,4
Who Is Likely to Experience Nodulocystic Acne on the Body?
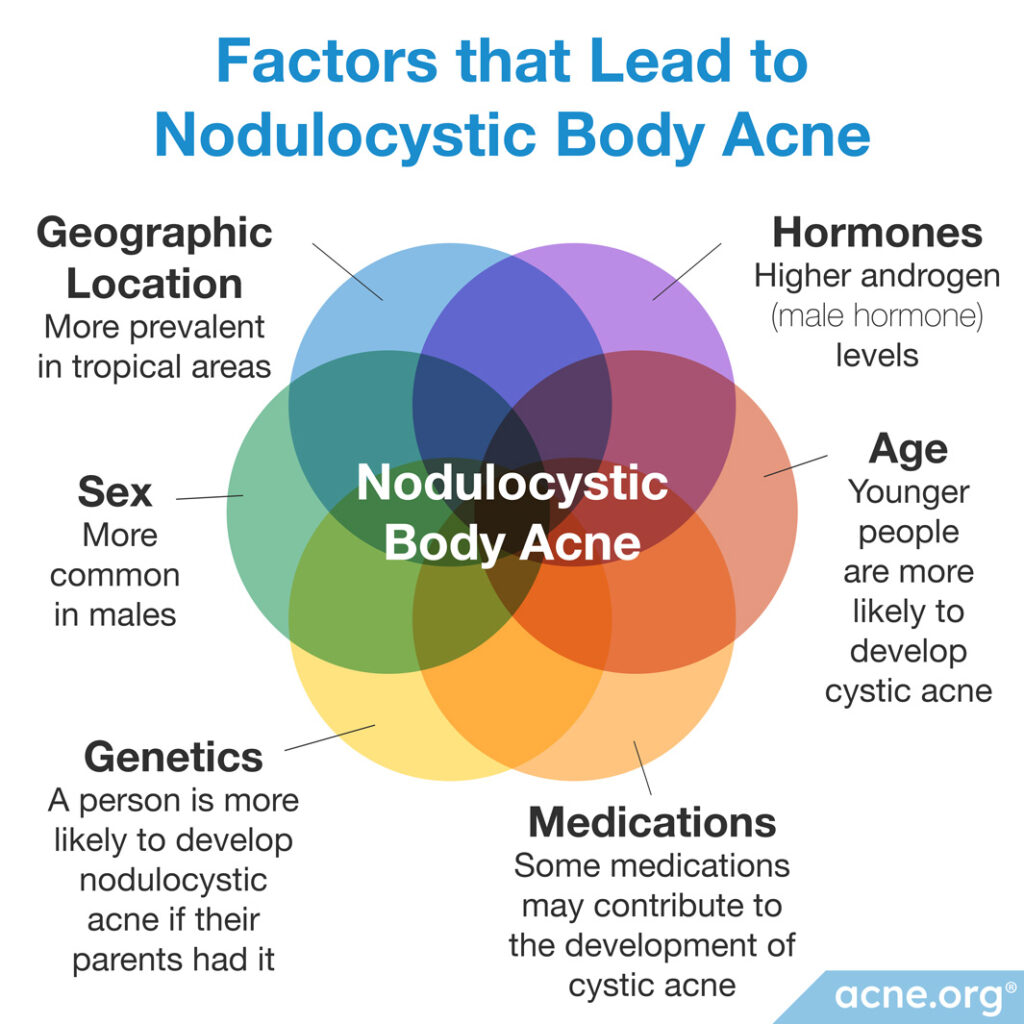
There are several factors that increase the likelihood that a person will develop nodulocystic acne on the body, or face for that matter:
- Hormones: Androgens are male hormones found in both males and females that increase the production of skin oil, called sebum, which is a substance necessary for the development of acne. Most nodulocystic acne patients have elevated androgen levels in their bodies, both in their blood and in their skin. There are several types of androgens, but those associated with acne include DHEA-S, testosterone, and DHT.
- Genetics: People are more likely to have nodulocystic acne if their parents or other close relatives had it.
- Geographic location: Nodulocystic acne is more prevalent in people who live in tropical regions of the world. The reason for this is unknown.
- Age: Nodulocystic acne is more common in teenagers and young adults, but can occur in younger or older people as well.
- Sex: Nodulocystic acne, particularly when it is on the body, is more common in males, but females can develop it too. Females are at a higher risk of developing it during the third trimester of pregnancy and during the premenstrual window (7 – 10 days before menstruation).5
- Medications: There are some reports describing the occurrence of cystic acne in patients treated with various medications.6,7
Treatment of Nodulocystic Acne on the Body
Treatment of nodulocystic acne on the body is the same as treatment on the face. Generally, people with only a few nodules or cysts can be treated with one or more of these therapies:
- Benzoyl peroxide: When combined in a regimen with glycolic acid, the combination can often clear the skin completely.
- Topical retinoids (tretinoin, adapalene, tazarotene, trifarotene): Topical retinoids normally provide some relief, but do not work well enough on their own to combat cystic acne. When combined with benzoyl peroxide, they work better.
- Oral antibiotics: In certain cases, physicians will prescribe oral antibiotics, but they must always be combined with other treatments, often do not provide relief, and come with worrying side effects. Never accept an oral antibiotic prescription without asking why it is necessary, and make sure you don’t stay on it for more than 3 months.
- Cortisone shots: Making a quick appointment with your dermatologist for a cortisone shot directly into a cystic lesion is a great way to instantly begin reducing inflammation and rapidly speed healing.8
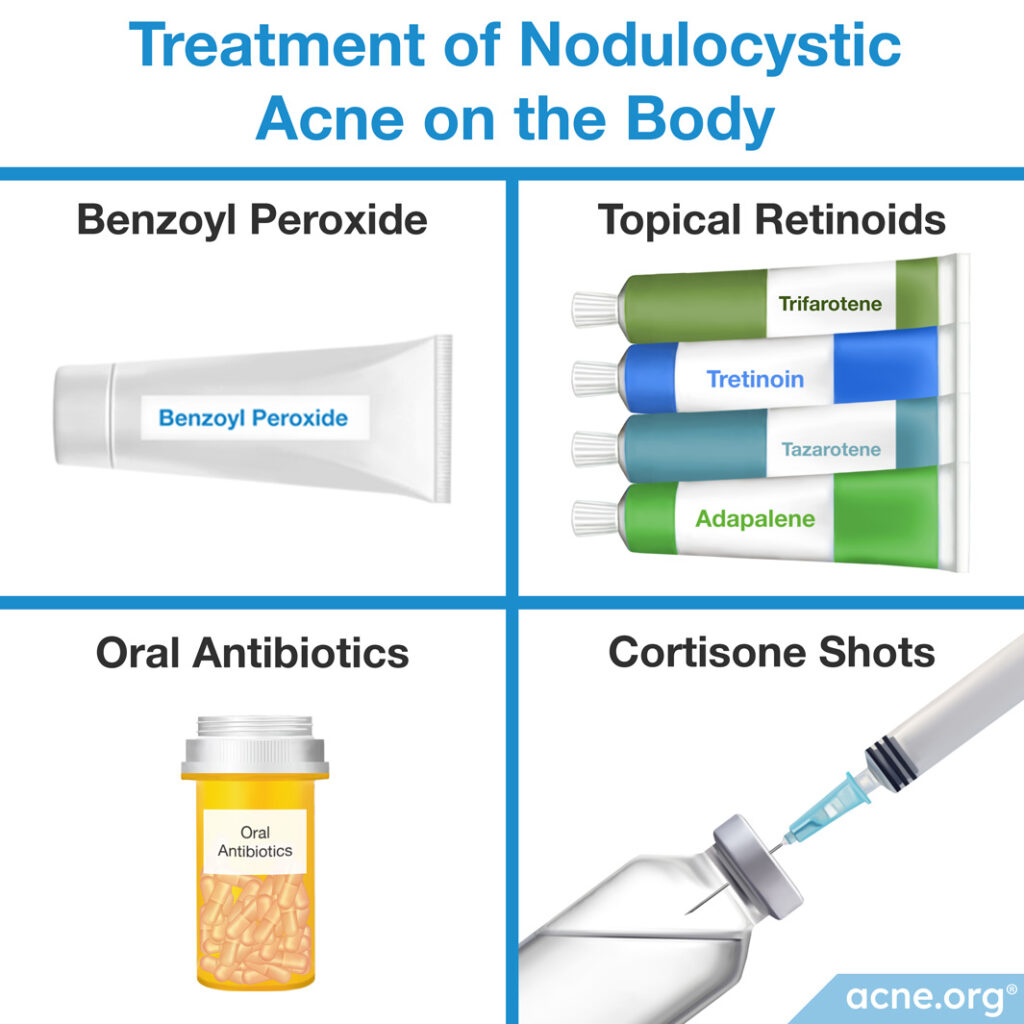
More severe nodulocystic acne sometimes requires treatment with isotretinoin (Accutane®), which is an oral medication normally prescribed for 15 – 20 weeks. Isotretinoin works by permanently reducing skin oil (sebum) levels. However, it comes with a plethora of side effects, some of which can be severe and lifelong, so it should never be entered into lightly. There is some question of whether isotretinoin may cause the skin to age more quickly in the long term as well.
Nodulocystic Acne Scarring on the Body
Untreated nodulocystic acne lesions often leave behind scarring. There are three types of scars that can develop from nodulocystic acne lesions on the body.
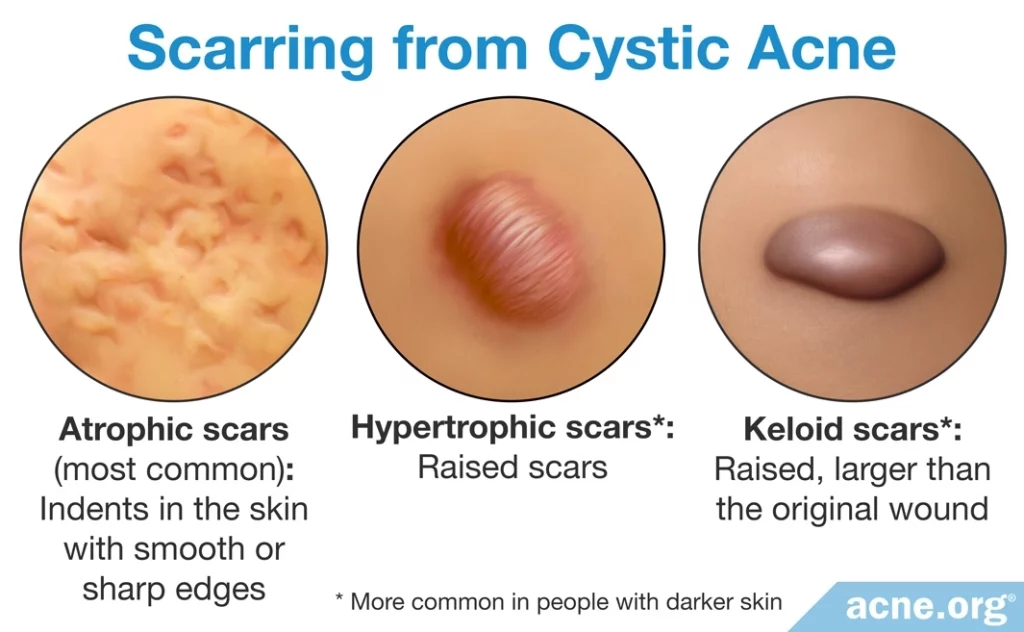
- Atrophic scars are indented beneath the skin surface, with either smooth or sharp edges. They are the most common scars that develop from nodulocystic acne lesions.
- Hypertrophic scars are elevated above the skin. When they first form, they are the same size as the acne lesion was on the skin, but over time hypertrophic scars may decrease in size. People with darker skin are more prone to develop this type of scarring.
- Keloid scars are similar to hypertrophic scars except that they are larger than the acne lesion was, and this size does not decrease over time. People with darker skin are also more prone to develop keloid scars.
There is a direct relationship between the severity of acne and the severity of resulting scarring. In other words, more severe scarring develops from larger and more abundant nodules and cysts. Also, the longer a person delays therapy for severe acne, the worse the scarring tends to be. This is why it is important to quickly and aggressively treat nodulocystic acne.9
There are a variety of treatment options available for reducing acne scars. According to a painstaking review published in the American Journal of Clinical Dermatology in 2018, laser therapy came out as the winner among effective scar treatments. However, the authors noted that multiple treatments are often combined for best results.10
Rare Forms of Nodulocystic Acne That Affect the Body
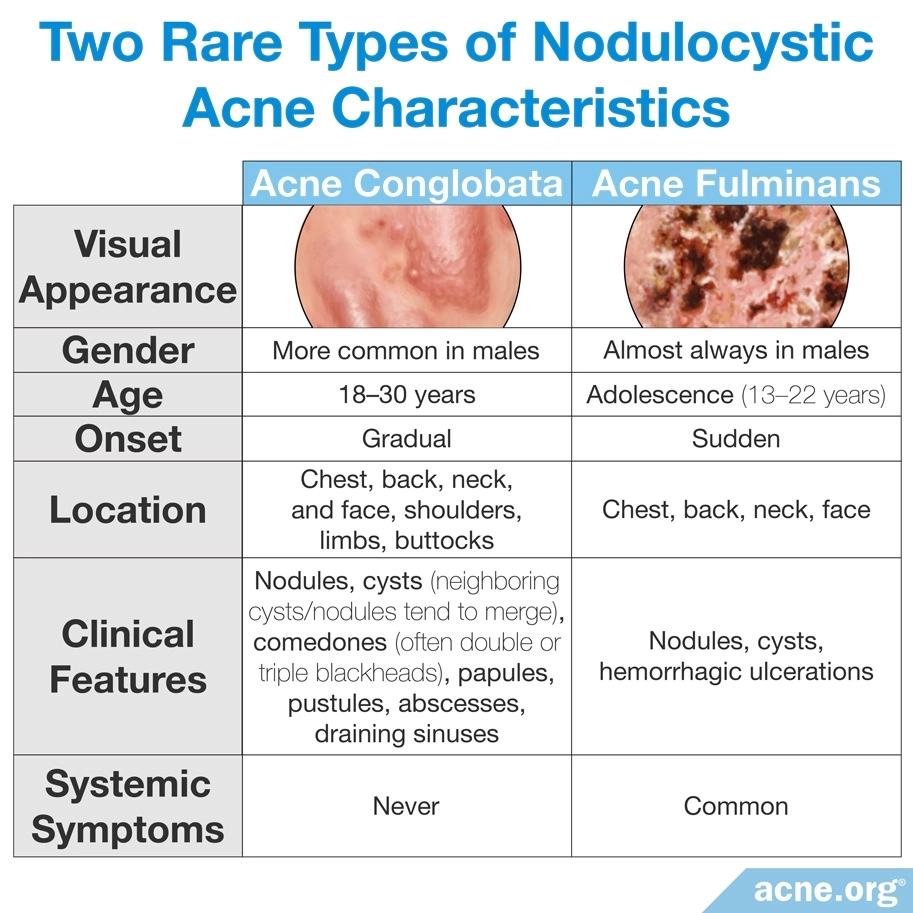
There are two uncommon forms of especially severe nodulocystic acne that can be found on the body:
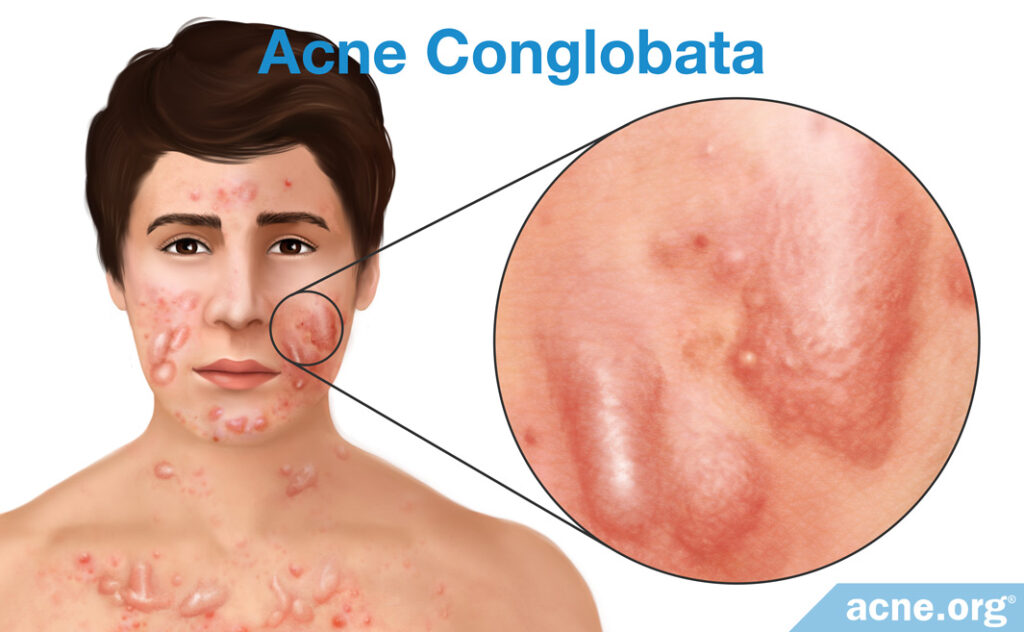
- Acne conglobata is an extensive, severe form of acne that usually involves the back, chest, upper arms, and to a lesser extent, the face. It presents a mixture of cystic lesions and less severe lesions. Acne conglobata may last for years and leave large scars. It is more prevalent in boys and young males, and in warmer climates. One complication associated with acne conglobata is a massive type of acne lesion called a draining sinus. Draining sinuses occur when two or more cysts merge into one sizable (2 – 5 centimeters) acne lesion. They can leak pus at any time and occur most often on the face around the nose and upper lip, but are not uncommon on the neck and chest. Draining sinuses can occur in general nodulocystic acne, but they are commonly associated with acne conglobata.3,11,12
- Acne fulminans is a systemic disease that includes fever, fatigue, joint and bone pain, weight loss, and also severe acne. Most frequently the acne lesions associated with this form of acne are found on the chest, back, neck, and face. Researchers suspect that hypersensitivity to acne bacteria (C. acnes) is in part responsible for acne fulminans.2

References
- Acne. https://en.wikipedia.org/wiki/Acne
- Plewig, G. & Kligman, A. Acne and Rosacea. (Springer International Publishing, 2000).
- Habif, T. P. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 231 – 233 (2016). https://www.elsevier.com/books/clinical-dermatology/habif/978-0-323-26183-8
- Nodulocystic acne. https://www.dermnetnz.org/topics/nodulocystic-acne/
- Arndt, K. Manual of Dermatologic Therapeutics (7th Edition). 5 – 8 (LWW (PE), 2007). https://shop.lww.com/Manual-of-Dermatologic-Therapeutics/p/9781451176346
- Hwang, A., Iskandar, A., Del Rosario, M. & Dasanu, C. A. Cystic acne due to imatinib therapy for chronic myelocytic leukemia. J. Oncol. Pharm. Pract. 25, 972-974 (2019). https://pubmed.ncbi.nlm.nih.gov/29498323/
- Kashat, M., Caretti, K. & Kado, J. Etanercept-induced cystic acne. Cutis 94, 31-32 (2014). https://pubmed.ncbi.nlm.nih.gov/25101341/
- Park, S. J., Shin, S. H., Koh, Y. G., Kim, G. H., Rho, N. K. & Park, K. Y. Cold anesthesia for pain reduction during intralesional steroid injection for nodulocystic acne. J. Cosmet. Dermatol. 22, 3375-3378 (2023). https://pubmed.ncbi.nlm.nih.gov/37218601/
- Layton, A., Henderson, C. & Cunliffe, W. A clinical evaluation of acne scarring and its incidence. Clin. Exp. Dermatol. 19, 303 – 308 (1994). https://www.ncbi.nlm.nih.gov/pubmed/7955470
- Bhargava, S., Cunha, P. R., Lee, J., Kroumpouzos, G. Acne scarring management: Systematic review and evaluation of the evidence. Am. J. Clin. Dermatol. 19, 459-477 (2018). https://www.ncbi.nlm.nih.gov/pubmed/29744784
- Jansen, T., Lindner, A. & Plewig, G. Draining sinus in acne and rosacea. A clinical, histopathologic and experimental study. Hautarzt 46, 417 – 420 (1995). https://www.ncbi.nlm.nih.gov/pubmed/7642386
- Acne Conglobata. https://emedicine.medscape.com/article/1072716-overview
 Acne.org Products
Acne.org Products