Because They Provide Limited Effectiveness and Come with Many Side Effects, They Should Be Met with Caution

The Essential Info
Antibiotics can sometimes be somewhat effective in treating acne. However, there are several problems with using antibiotics to treat acne:
- They may not work: Oftentimes, antibiotics fail to work at all. When they do work, they are not known to produce impressive results. Other, safer medications are often more effective.
- Temporary benefit: Even when they work to some degree, the benefits are temporary since antibiotics should not be prescribed for longer than 3 months.
- Side effects: Antibiotics can cause a wide variety of side effects that range from uncomfortable to life-threatening.
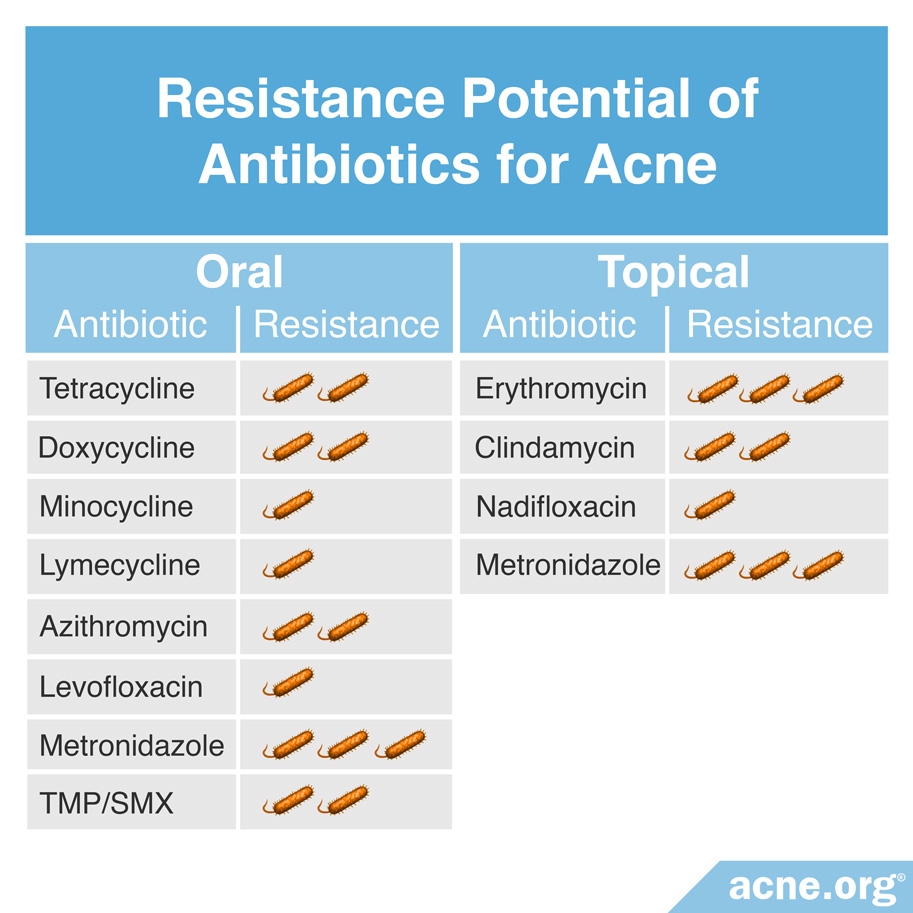
- Antibiotic resistance: Treatment with antibiotics, especially over long periods of time, leads to antibiotic resistance, which is becoming a worldwide problem that threatens to undermine our ability to treat bacterial infections in the future.
- Over-prescribed: Even though scientists strongly recommend limiting antibiotic use to severe acne and only for short courses of treatment, many doctors prescribe antibiotics for less severe acne and for long periods of time.
Antibiotics are powerful medicines that can save lives when used appropriately for bacterial infections. They may have a legitimate role in acne treatment in the short term in some cases, but they should be drugs of last resort, not the first options used. And when they are used, they should be prescribed sparingly and only for short periods of time–no longer than 3 months.
Be Your Own Advocate: If your doctor prescribes an antibiotic to treat your acne, do not simply accept it without question. Ask your doctor about side effects and about other options instead of antibiotics. If you do decide to use antibiotics, never use them for more than 3 months and always take them on time and complete the entire prescribed course, because skipping doses or stopping too soon increases the chances of developing resistant bacteria. Before considering antibiotics, always try other topical medications such as benzoyl peroxide first, and only use antibiotics if these other medications do not work.

The Science
- How Effective Are Antibiotics and How Do They Compare with Other Medications?
- Side Effects of Antibiotics
- Antibiotic Resistance: A Big Concern
- Conclusion
Doctors sometimes prescribe both topical and oral antibiotics to treat acne, especially severe acne. This practice is controversial. While prescribing antibiotics for acne remains common, as many physicians become increasingly wary of antibiotics’ limited effectiveness and drawbacks, they are prescribing them less frequently.
Antibiotic medications are sometimes helpful in treating acne, but they also have many side effects that range from mild skin irritation and stomach upset to severe neurological problems and life-threatening diarrhea. Other concerning long-term side effects include the possibility of permanent tooth and skin discoloration.
While antibiotics can be useful in acne treatment, there is no evidence that they are any more effective than other acne treatments, such as benzoyl peroxide (males and females) or oral contraceptives (females only). There is also evidence that antibiotics sometimes fail to work at all. To make matters worse, it is unsafe to use antibiotics for more than 3 months, so results are temporary.
For all of these reasons, it is important that acne patients try other options first. If antibiotics are chosen as a treatment, they should be prescribed for a maximum of 3 months, and should always be prescribed alongside other medications and never on their own.1
How Effective Are Antibiotics and How Do They Compare with Other Medications?
While antibiotics can work to some degree in some people, results are unimpressive, particularly when compared with other, safer treatment options that work just as well or better. Let’s have a look.
The antibiotics used to treat acne fall into two broad categories:
- Oral antibiotics: Taken by mouth. Oral antibiotics are systemic medications, meaning that they have effects throughout the body.
- Topical antibiotics: Applied to the skin. Topical antibiotics work locally, meaning that they affect the area of skin to which they are applied.
Oral Antibiotics

Doctors sometimes prescribe oral antibiotics to treat moderate-to-severe acne. The most commonly prescribed oral antibiotics for acne are:
- Minocycline
- Doxycycline
- Tetracycline
- Erythromycin
Oral antibiotics can be at least somewhat helpful in treating acne, with minocycline considered the most effective oral antibiotic for acne, and doxycycline the next most effective.2
Several studies show that oral antibiotics can be somewhat effective in treating acne3-5, and may reduce symptoms by approximately 50%3, but are not more effective than other medications.
Concerningly, two studies have reported that a significant number of patients fail to see improvement from oral antibiotics. One recent scientific article notes that in many cases, oral antibiotics fail to help patients with severe acne.6 Another recent study found that about ¼ of patients are dissatisfied with oral antibiotics due to lack of improvement in their acne.7
Expand to read details of research

According to a 2007 article in the Journal of the American Academy of Dermatology, “Antibiotics have been widely used for many years in the management of acne. There is evidence to support the use of tetracycline, doxycycline, minocycline, erythromycin, trimethoprim-sulfamethoxazole, trimethoprim, and azithromycin…[and] Systemic antibiotics are a standard of care in the management of moderate and severe acne and treatment-resistant forms of inflammatory acne.”2

The same article in the Journal of the American Academy of Dermatology noted, “Doxycycline and minocycline are more effective than tetracycline, and there is evidence that minocycline is superior to doxycycline in reducing C. acnes [bacteria associated with acne].”2

A 2011 review in The Journal of Family Practice found that doxycycline reduced acne lesions by about 50%. The authors reported, “A 2003 randomized, double-blind, controlled trial of 51 patients demonstrated that a subantimicrobial dose of doxycycline (20 mg orally twice a day) reduced comedonal lesions by 53.2%…and inflammatory lesions by 50.1%”3

A 12-week 2012 study in the Iranian Journal of Dermatology compared the efficacy of doxycycline and azithromycin (a less frequently prescribed antibiotic for acne) administered along with the topical retinoid medication tretinoin. This study found doxycycline and azithromycin to be equally effective, with between 40% and 67% of patients showing a greater than 80% reduction in acne lesions. However, since the patients in the study were also treated with tretinoin at the same time as the antibiotics, it is impossible to determine which medication improved their acne.4

A 2014 study in the Journal of the American Academy of Dermatology compared the efficacy of oral contraceptives and oral antibiotics for treating acne in females. This study found that antibiotics were more effective at reducing acne lesions in the first three months of treatment, but by six months of treatment, oral contraceptives were equally effective. The authors noted, “Although antibiotics may be superior at 3 months, [oral contraceptives] are equivalent to antibiotics at 6 months in reducing acne lesions and, thus, may be a better first-line alternative to systemic antibiotics for long-term acne management in women.”5

According to a 2015 study in the Journal of the American Academy of Dermatology, in a significant number of patients with severe acne who are initially prescribed oral antibiotics, the antibiotics fail to work. Many patients with severe acne are prescribed oral antibiotics and eventually have to change to isotretinoin due to lack of efficacy.6

A 2019 study in the Journal of Dermatological Treatment analyzed 5,527 Instagram posts shared by people with acne over an 8-year period. They found that 25.6% of acne patients taking oral antibiotics and 9.8% of acne patients using topical antibiotics were dissatisfied due to lack of improvement.7
Topical Antibiotics

Doctors also sometimes prescribe topical antibiotics to treat acne. The most commonly prescribed topical antibiotics for treating acne are:
- Clindamycin
- Erythromycin
Articles published in the Journal of the American Academy of Dermatology and the Journal of the European Academy of Dermatology remark about how topical antibiotics work to some degree in some people, but that other acne medications, such as topical benzoyl peroxide, work better.2,8
Expand to read details of articles

A 2007 article in the Journal of the American Academy of Dermatology noted, “The value of topical antibiotics in the treatment of acne has been investigated in many clinical trials. Both erythromycin and clindamycin have been demonstrated to be effective and are well tolerated.“2

Both clindamycin and erythromycin are at least moderately effective in treating acne. Both medications can reduce the number of inflammatory lesions by about 40 – 60%. According to a 2015 article in the Journal of the European Academy of Dermatology, “Clinical data show that erythromycin reduced the inflammatory lesion count by between 40 – 60%. Clindamycin applied for 12 weeks provided similar results.”8

The same 2015 article in the Journal of the European Academy of Dermatology noted that topical benzoyl peroxide was just as effective as antibiotics for inflammatory lesions and even more effective for non-inflammatory lesions. The authors stated, “After 3 months of treatment, [benzoyl peroxide] was similar to clindamycin in reducing the number of inflammatory lesions and reduced the non-inflammatory lesion count by 30% compared to 9% with clindamycin. Similar results were obtained when compared to erythromycin.”8
Doctors almost always prescribe topical antibiotics with benzoyl peroxide or one of the available topical retinoids such as tretinoin in order to reduce the antibiotic resistance that occurs with antibiotic use. This is especially true of erythromycin and clindamycin since they cannot be used as a single therapy due to their high potential of causing antibiotic resistance.2
It appears that combining other medications with topical antibiotics is superior than either used alone, as explained in a scientific article published in 2007.9
Expand to read quote from article

According to a 2007 article in the Journal of the American Academy of Dermatology, “A combination of topical retinoids and topical erythromycin or clindamycin is more effective than either agent used alone. Combining erythromycin or clindamycin with benzoyl peroxide eliminates or reduces bacterial resistance and enhances efficacy.”2 Similarly, a 2014 study in Drug Therapy Topics also found that combined treatment with clindamycin and benzoyl peroxide was more effective than either medication alone.9
And here is a study that shows us that safe over-the-counter medications are superior to topical antibiotics, even when topical antibiotics are combined with other medications:

A 2010 study in the Journal of the American Academy of Dermatology found that combination treatment with two popular over-the-counter medications, benzoyl peroxide and salicylic acid, was more effective than a topical antibiotic alone and a topical antibiotic in combination with benzoyl peroxide.10
Side Effects of Antibiotics
Even when they do show some results, both oral and topical antibiotics frequently cause side effects that range from mild to severe.
Click here for a full article outlining the side effects of antibiotics.
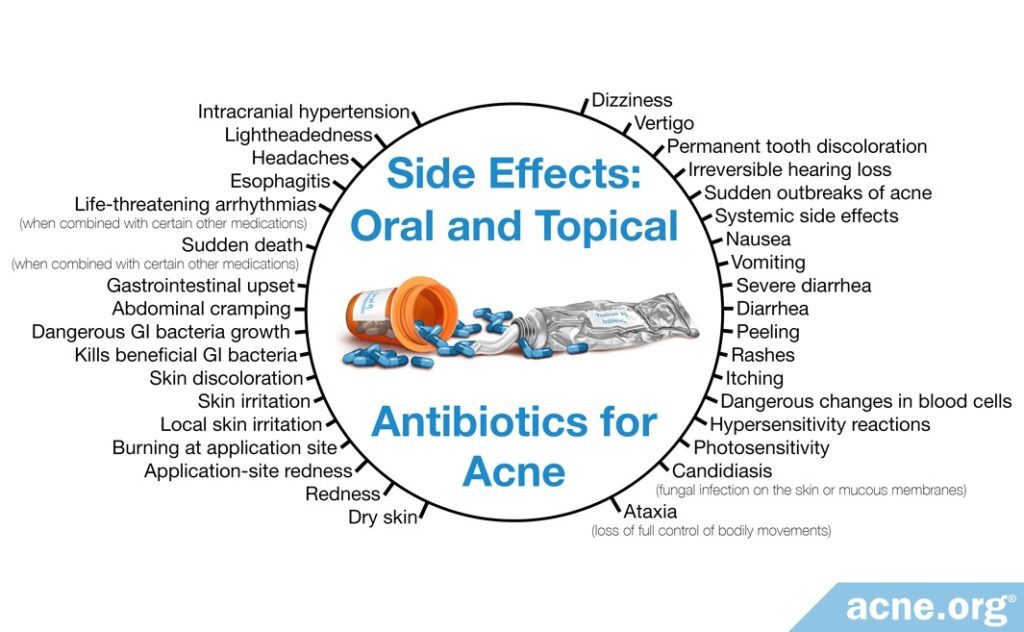
Oral Antibiotic Side Effects
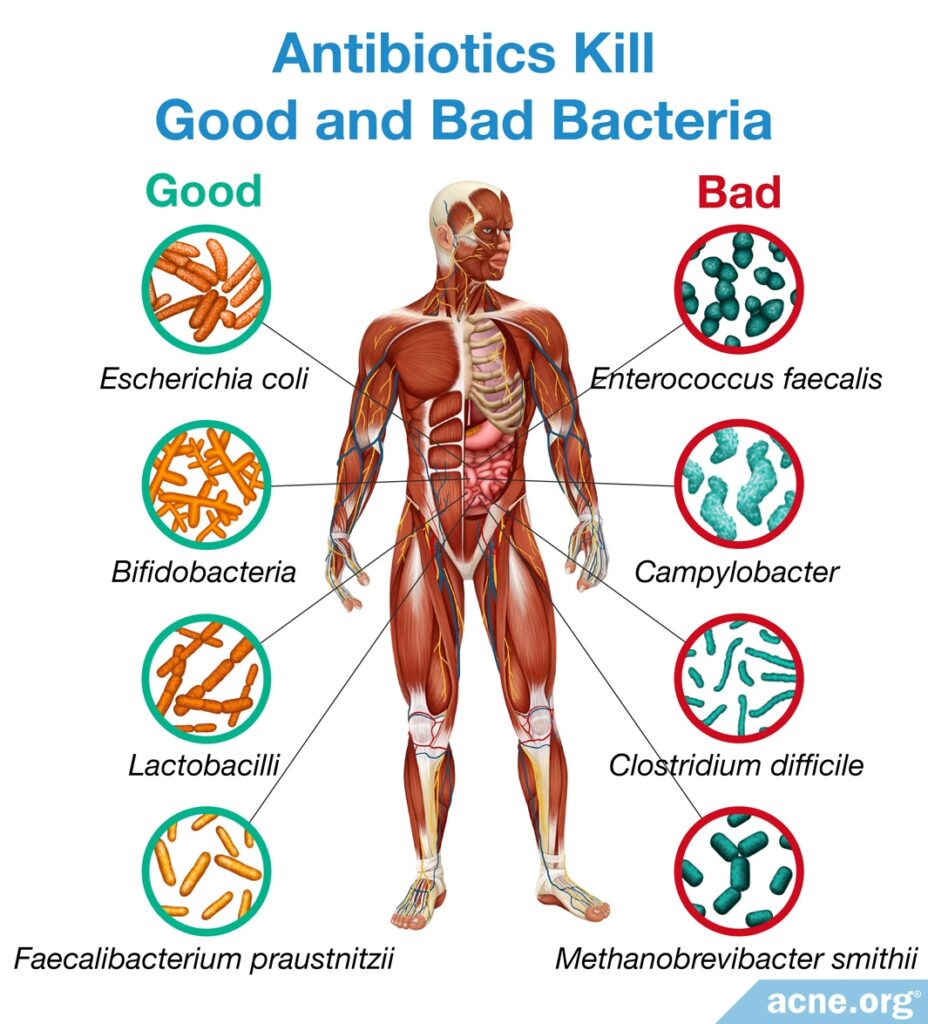
The majority of the side effects from oral antibiotics stem from the fact that antibiotics do not just kill the bacteria that they are targeting for a particular condition; they also kill beneficial bacteria along with the harmful ones. This leads to an imbalance in the bacterial composition of the intestines.
Oral antibiotics cause a wide variety of side effects, the most common of which is gastrointestinal upset, such as nausea and diarrhea, which occurs in up to 1/2 of patients taking oral antibiotics.11
Here are some other examples of side effects that various oral antibiotics can cause:
- Doxycycline causes sensitivity to sunlight. Other antibiotics in the tetracycline family, such as tetracycline and minocycline, also cause sensitivity to sunlight, but to a lesser degree than doxycycline.2
- Tetracycline antibiotics can cause skin irritation such as rashes.11
- Minocycline can cause permanent discoloration of the teeth and skin.2
- Minocycline can also cause rare but very severe side effects such as dizziness, vertigo, and autoimmune diseases.2,11
- Erythromycin can cause stomach cramps, nausea, and vomiting.11
- All systemic antibiotics may be associated with higher frequency of upper respiratory tract infections.8
Topical Antibiotic Side Effects
Topical antibiotics cause less severe side effects than oral antibiotics. The most common side effects of topical antibiotics are:
- Skin irritation
- Rashes
- Dryness2
However, when applied to large areas of skin, clindamycin can also be absorbed into the body and cause serious systemic side effects, including:
- Diarrhea
- Severe Colitis
- Dryness11,12
Antibiotic Resistance: A Big Concern
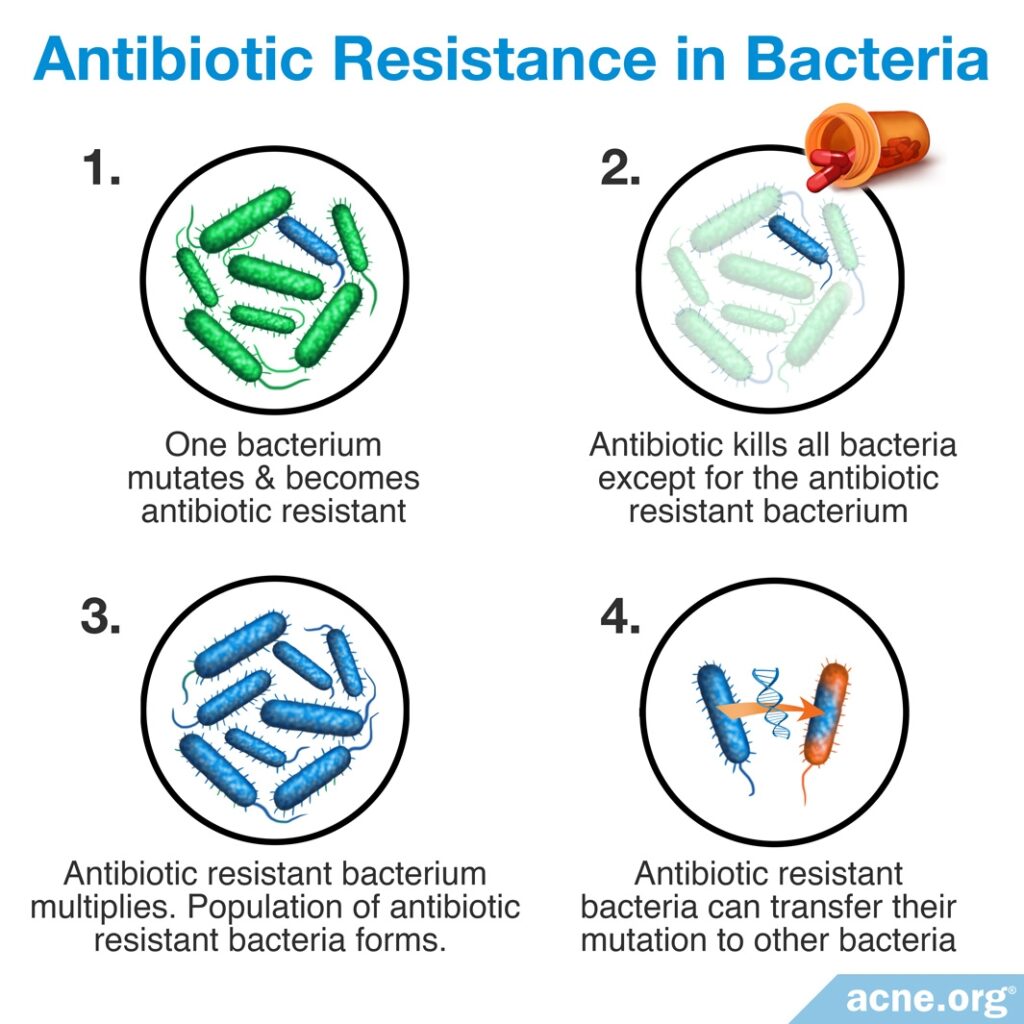
Treatment with oral or topical antibiotics, especially over longer periods of time, can also lead to a phenomenon called antibiotic resistance. Antibiotic resistance means that bacteria become immune to the effects of antibiotics over time, and eventually the antibiotics can no longer kill the bacteria. Antibiotic resistance is a serious global problem, because:
- When bacteria become resistant to an antibiotic, that antibiotic becomes less effective and less able to treat the condition for which it was prescribed as well as for other bacterial conditions. This applies to both the person taking the antibiotic as well as the population at large.
- Bacteria can share their genes with each other and transfer antibiotic resistance from one strain of bacteria to another.
- Ultimately, antibiotic resistance could result in many types of bacteria becoming resistant to all antibiotic medications. This means that doctors may eventually be unable to treat bacterial infections, and people may die from even common bacterial diseases such as strep throat, as people did before antibiotics were developed.
Because of the risk of antibiotic resistance, scientists and doctors have put together a set of guidelines for using antibiotics in acne treatment. These guidelines state that antibiotics should only be used to treat acne:
- For 3 months at most
- Together with other acne treatments rather than alone13,14
Unfortunately, many doctors still prescribe antibiotics to their acne patients for longer periods. For example, one study in England found that 79% of acne patients in that country used antibiotics for over 3 months. The researchers wrote, “Results indicate that oral antibiotic prescribing for acne in the community does not align with current guideline recommendations.”1
Expand to read details of study

This study was published in 2019 in the British Journal of Dermatology. The researchers combed through a database of patients treated for acne in England between January 2004 and April 2017. For their analysis, the researchers included any patients between 12 and 25 years old who were treated with antibiotics. Out of 928 patients who fit this description, it turned out that 79% had used antibiotics for over 3 months, and 28% had used antibiotics for longer than 1 year.1
Conclusion
Antibiotics are powerful medicines that can save lives when used appropriately for bacterial infections. They may have a legitimate role in acne treatment in some special cases in the short term, but they should be drugs of last resort, not the first options used. And when they are prescribed, they should be used sparingly and only for short periods of time–no longer than 3 months.
If your doctor recommends antibiotics for your acne treatment, make sure to ask questions. Why does he/she think antibiotics are the best course of action for you? How long does he/she think you should use them? What is the reasoning behind using antibiotics instead of other treatments? You and your doctor may decide that antibiotics are the way to go, but be your own advocate. It’s your body.
References
- Whitehouse, H., Solman, L., Eady, E. A., Layton, A. 3. Oral antibiotics in acne: a retrospective single-centre analysis of current prescribing in primary care and its alignment with the national antibiotic quality premium. Br. J. Dermatol. 181, 1341-1342 (2019). https://www.ncbi.nlm.nih.gov/pubmed/31301232
- Strauss, J. S. et al. Guidelines of care for acne vulgaris management. J. Am. Acad. Dermatol. 56, 651 – 663 (2007). https://www.ncbi.nlm.nih.gov/pubmed/17276540
- Gannon, M., Underhill, M. & Wellik, K. E. Clinical inquiries. Which oral antibiotics are best for acne? J. Fam. Pract. 60, 290 – 292 (2011). https://www.mdedge.com/familymedicine/article/64303/dermatology/which-oral-antibiotics-are-best-acne
- Moravvej, H., Halim, A. M., Yousefi, M. & Givrad, S. Efficacy of doxycycline versus azithromycin in the treatment of acne. Iran. J. Dermatol. 15, 7 – 10 (2012). https://pdfs.semanticscholar.org/9b58/82d3ce592969dd6e9522b64bea2c6210ab27.pdf
- Koo, E. B., Petersen, T. D. & Kimball, A. B. Meta-analysis comparing efficacy of antibiotics versus oral contraceptives in acne vulgaris. J. Am. Acad. Dermatol. 71, 450 – 459 (2014). https://www.ncbi.nlm.nih.gov/pubmed/24880665
- Nagler, A. R., Milam, E. C. & Orlow, S. J. The use of oral antibiotics before isotretinoin therapy in patients with acne. J. Am. Acad. Dermatol. 74, 273 – 279 (2016). https://www.ncbi.nlm.nih.gov/pubmed/26525749
- Reddy, P. S., DeBord, L. C., Gupta, R., Kapadia, P., Mohanty, A., Dao, H Jr. Antibiotics for acne vulgaris: using instagram to seek insight into the patient perspective. J. Dermatolog. Treat. 27, 1-5 (2019). https://www.ncbi.nlm.nih.gov/pubmed/31190574
- Leccia, M. T. et al. Topical acne treatments in Europe and the issue of antimicrobial resistance. J. Eur. Acad. Dermatol. Venereol. 29, 1485 – 1492 (2015). https://www.ncbi.nlm.nih.gov/pubmed/25677763
- Del Rosso, J. Q. Topical therapy for acne in women: is there a role for clindamycin phosphate-benzoyl peroxide gel? Cutis 94, 177 – 182 (2014). https://www.mdedge.com/dermatology/article/87886/acne/topical-therapy-acne-women-there-role-clindamycin-phosphate-benzoyl
- Seidler, E. M. & Kimball, A. B. Meta-analysis comparing efficacy of benzoyl peroxide, clindamycin, benzoyl peroxide with salicylic acid, and combination benzoyl peroxide/clindamycin in acne. J. Am. Acad. Dermatol. 63, 52 – 62 (2010). https://www.ncbi.nlm.nih.gov/pubmed/20488582
- Tripathi, S. V., Gustafson, C. J., Huang, K. E. & Feldman, S. R. Side effects of common acne treatments. Expert Opin. Drug Saf. 12, 39 – 51 (2013). https://www.ncbi.nlm.nih.gov/pubmed/23163336
- Oudenhoven, M. D., Kinney, M. A., McShane, D. B., Burkhart, C. N. & Morrell, D. S. Adverse effects of acne medications: recognition and management. Am. J. Clin. Dermatol. 16, 231 – 242 (2015). https://www.ncbi.nlm.nih.gov/pubmed/25896771
- Habeshian, K. A., & Cohen, B. A. Current issues in the treatment of acne vulgaris. Pediatrics 145, 225-230 (2020). https://pubmed.ncbi.nlm.nih.gov/32358215/
- Dessinioti, C. & Katsambas, A.. Antibiotics and antimicrobial resistance in acne: Epidemiological trends and clinical practice considerations. The Yale Journal of Biology and Medicine95, 429-443 (2022). https://pubmed.ncbi.nlm.nih.gov/36568833/
 Acne.org Products
Acne.org Products