A Draining Sinus Is a Large, Red, Painful Lesion That Develops from the Merging of Multiple Acne Cysts

The Essential Info
Draining sinuses are huge, tender bumps that form when multiple cysts combine under the skin. They are the largest type of a lesion found in “nodulocystic” acne, often referred to simply as “cystic acne,” and are very likely to leave behind scars.
Draining sinuses get the name “draining” because they contain pus that can spontaneously leak onto the skin. However, they should never be popped.
Treatments (Talk to Your Doctor)
- Cortisone Shots
- Incision and Drainage
- Aspiration
- Surgical Removal
- Cryotherapy
Prevention
- Isotretinoin (Accutane®): Powerful, but with many side effects.
- Benzoyl Peroxide: Works well to prevent acne, but sometimes not enough for the most severe cases of cystic acne.
- Oral Antibiotics: Can be a short-term aid, but limited effectiveness and many side effects.
- Cortisone Shots into Existing Cysts: Can prevent existing cysts from merging into a draining sinus.
- Cryotherapy: Non-invasive and can sometimes help heal existing cysts before they merge.
- Photodynamic Therapy: A new therapy that is painful and may have long-term repercussions, but may be an option.
- Hormonal Treatment (females only): Aims to get to the “root” of the issue.

The Science
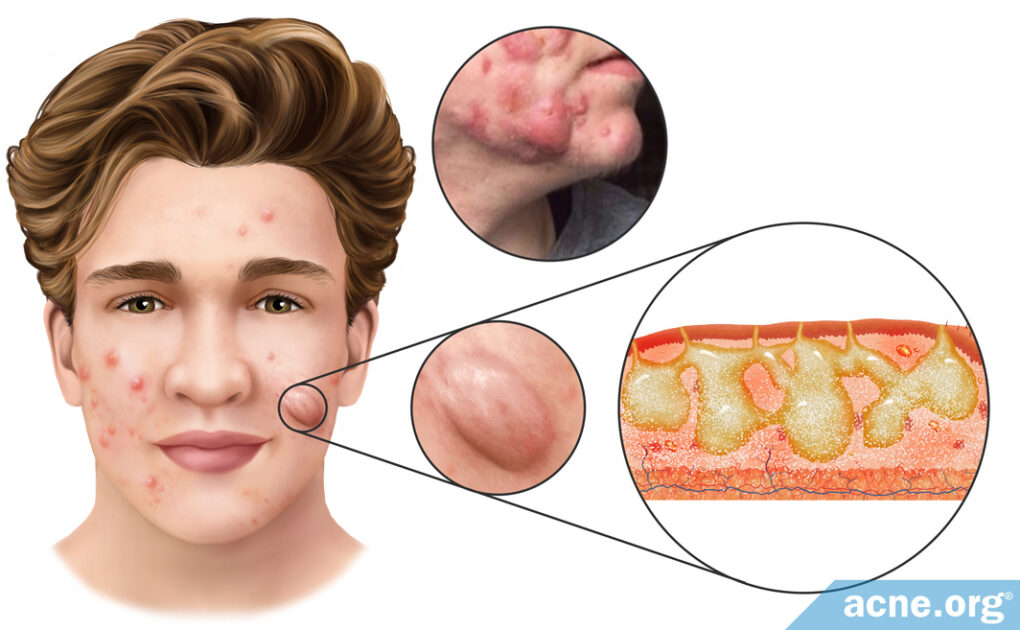
Draining sinuses develop when multiple acne cysts merge to form one huge lesion. They appear as raised, red, soft bumps around 2-5 centimeters long that occasionally leak pus. They tend to be elongated in shape, whereas single acne cysts are usually more circular.
Draining sinuses most commonly arise on the face, near the nasolabial fold–the area running from the sides of the nose down to the sides of the mouth–often called “smile lines” or “laugh lines.”
Once a draining sinus develops, it often persists on the skin for months or even years, will not resolve without treatment, and leaves large scars. Most often, draining sinuses occur only with especially severe forms of acne, including acne conglobata, acne fulminans, pyoderma faciale, and acne inversa.1-3
Inside of a draining sinus lies pus, acne bacteria, inflammatory cells, skin cells, hair remnants, and skin oil. Occasionally, a draining sinus will contain disease-causing bacteria in addition to the normal bacteria found in the skin, called C. acnes.
Formation of a Draining Sinus
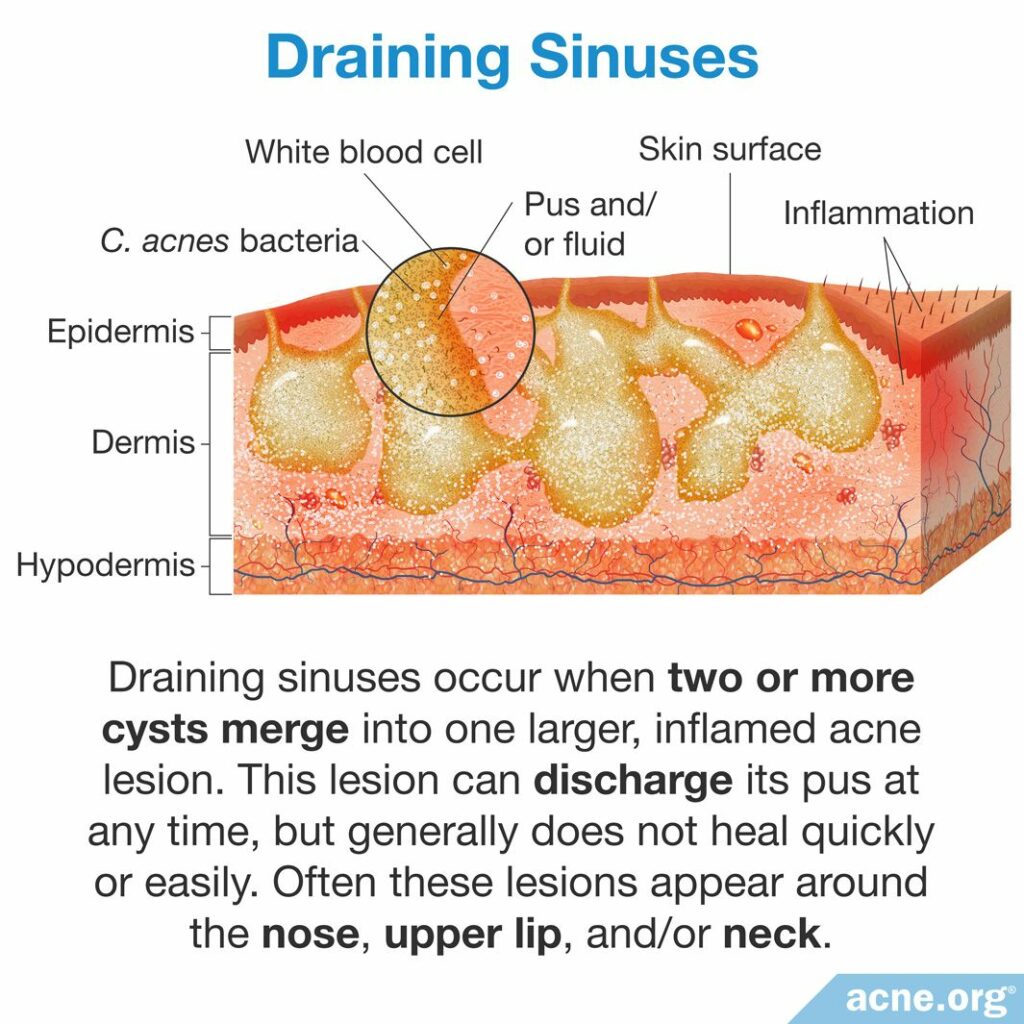
A draining sinus forms from the merging of multiple acne cysts.
Formation of an acne cyst
All acne lesions start when a hair follicle (pore) becomes clogged. A clogged pore is the ideal environment for acne bacteria, which begins to divide rapidly inside the pore. In response to this, the body produces inflammation that damages the pore wall and causes it to rupture. If a small portion of the pore wall ruptures, then a run-of-the-mill pimple forms. However, if the entire pore explodes, a cyst can result.
Formation of a draining sinus
Draining sinuses form when multiple acne cysts combine to form one large, interconnected lesion. During this merging, a series of interconnected tunnels forms, which connects the multiple cysts in the deep layers of the skin. These tunnels consist of multiple openings that lead to the surface of the skin. Inside the cysts and tunnels there is a mix of pus, bacteria, inflammatory cells, skin cells, hair remnants, and skin oil. These contents can spontaneously leak onto the surface of the skin.1,2
What Causes Draining Sinuses?
Exactly what causes the formation of a draining sinus in individuals with acne cysts is unknown. Researchers have found that people with diseases of the sinus tract or who have family members with a sinus tract disease tend to be more likely to develop draining sinuses. However, the reason behind this connection is unknown.
Treatment Options for Draining Sinuses

Once a draining sinuses is formed, a dermatologist can treat it with a variety of treatments. Like acne cysts, draining sinuses should never be attempted to be popped, as this will only cause the contents to be expelled deeper into the skin, worsening the lesion, permanently damaging the skin, and leaving behind severe scarring.
Draining sinus treatments
Draining sinuses are difficult to treat, and dermatologists are not yet sure of the best method to treat them. However, there are several options to clear draining sinuses once they form in the skin, and a combination of methods is often employed. Caution: Never try any of these at home. It will result in a more severe lesion, potential infection, and worsen scarring.
- Intralesional shots (cortisone shots): Intralesional shots, often called cortisone shots, involve injecting an anti-inflammatory medication called a corticosteroid directly into the draining sinus. The introduction of corticosteroids into the draining sinus decreases swelling without increasing the risk of scarring.
- Incision and drainage: Due to the severity of a draining sinus, surgical intervention that cuts and drains the lesion is often required. This procedure involves cutting open the draining sinus with a blade in sterile conditions and draining its contents. However, this treatment option is only moderately effective, as draining sinuses will likely refill. Further, this procedure also increases the risk of scarring.
- Aspiration: The term aspiration refers to inserting a thick needle into the lesion and removing the contents. This treatment is likely only temporary because the draining sinus will likely refill. However, aspiration is less likely to cause scarring.
- Surgical removal: In especially stubborn draining sinuses, when other treatment options do not work, the draining sinus will have to be removed surgically from the skin. Although this option is most likely to cure the draining sinus, it will leave large scars.
- Cryotherapy: Cryotherapy is a procedure performed by freezing an acne lesion with a liquid nitrogen spray for about 15 seconds. Freezing of the draining sinus prevents its growth and supports its healing. However, cryotherapy is not the preferred treatment option for draining sinuses, as it does not work well on every skin type, and it can leave severe scars if performed improperly.4,5
In addition, scientists are now looking into fluorescent light energy (FLE) as a potential option for treating draining sinuses. Fluorescent light therapy is a new procedure in which a doctor applies a fluorescent gel to the skin and then shines LED light on it. Preliminary research suggests that this treatment might help decrease inflammation and improve skin repair, thus reducing the chance of scarring. However, research on the efficacy of this procedure is still ongoing.6-8
Draining sinus prevention: acne cyst treatments
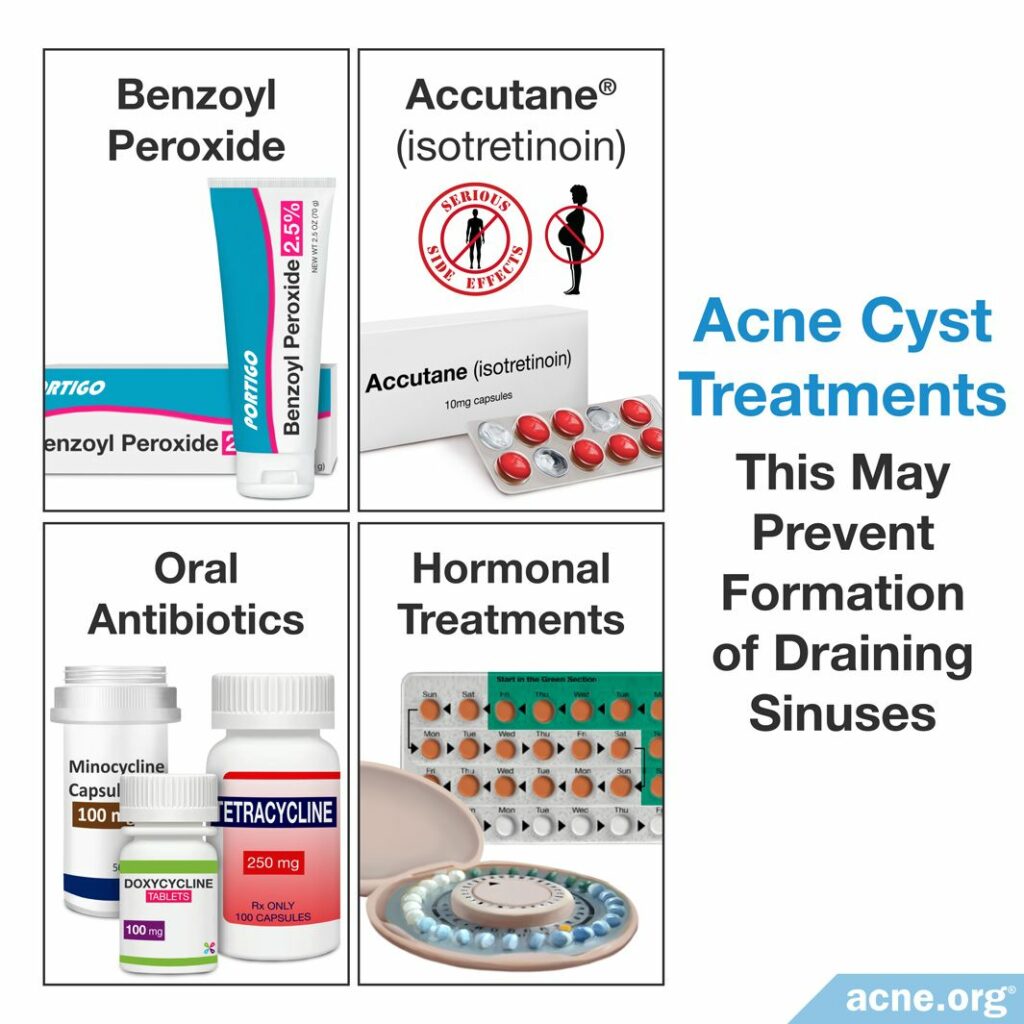
By treating individual acne cysts before they can combine into draining sinuses, the formation of a draining sinus can be prevented. There are several treatment options for acne cysts.
- A properly applied benzoyl peroxide regimen: To prevent future cysts, treating the skin gently and applying benzoyl peroxide in the right manner can stop the development of any type of acne lesion, including cysts.
- Isotretinoin + corticosteroids: Isotretinoin, often known by its brand name Accutane®, is an oral medication that permanently and irreversibly changes the skin and body, and therefore it is a treatment of last resort, only being approved for severe, widespread cystic acne. However, in the case of severe acne that comes with draining sinuses doctors often advise its use, sometimes in combination with oral corticosteroids, which help quickly reduce inflammation. Patients will often take corticosteroids for the first 2 – 4 weeks of treatment in order to decrease swelling, redness, and pain quickly. Then, after a few weeks of corticosteroid treatment, patients will begin taking an isotretinoin dosage of 0.5 – 1 milligram/kilogram/day, usually for 15 – 20 weeks. The combination of corticosteroids and isotretinoin is highly effective at clearing acne cysts, but it is a serious decision, since isotretinoin comes with severe side effects, some of which may be lifelong. These side effects include permanent changes to the body and dramatic birth defects or fetal death if taken by pregnant women.
- Oral antibiotics: Oral antibiotics, including minocycline, doxycycline, and tetracycline are alternatives to isotretinoin that can temporarily help clear acne cysts. Oral antibiotics should only be used for a maximum of three months, and although they may help reduce acne cysts during treatment, the acne will likely return once the treatment is stopped. Further, oral antibiotics cause side effects, including gastrointestinal issues, and can permanently stain the teeth or skin. Oral antibiotics should never be taken with isotretinoin because there is a risk of developing a disease called pseudotumor cerebri, which causes a buildup of pressure inside the skull. Oral antibiotics are also sometimes prescribed alongside draining sinuses treatments to prevent the development of infections inside the draining sinus.
- Hormonal treatments (females): Hormonal treatments, including oral contraceptives and spironolactone, are treatments female patients can use to treat acne cysts. These treatments can only be used by females since they can cause feminization symptoms in males, including breast growth, as well as sexual dysfunction. In females, however, hormonal treatments can be highly effective at clearing acne cysts.9-12
References
- Jansen, T., Lindner, A. & Plewig, G. Draining sinus in acne and rosacea. A clinical, histopathologic and experimental study. Hautarzt 46, 417 – 420 (1995) https://www.ncbi.nlm.nih.gov/pubmed/7642386
- Anderson, B., Netter, F. & Machado, C. THE NETTER COLLECTION of Medical Illustrations. (Elsevier Saunders, 2012) https://www.elsevier.com/books/the-netter-collection-of-medical-illustrations-integumentary-system/anderson/978-1-4377-5654-8
- Kurzen, H., Jung, E. G., Hartschuh, W., Moll, I., Franke, W. W. & Moll, R. Forms of epithelial differentiation of draining sinus in acne inversa (hidradenitis suppurativa). Br J Dermatol 141, 231-239 (1999). https://pubmed.ncbi.nlm.nih.gov/10468793/
- Jansen, T., Romiti, R., Plewig, G. & Altmeyer, P. Disfiguring draining sinus tracts in a female acne patient. Pediatr Dermatol 17, 123 – 125 (2000). https://www.ncbi.nlm.nih.gov/pubmed/10792801
- Hafsi, W. & Badri, T. Acne Conglobata. [Updated 2019 May 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459219/
- Koceva, I., Rümmelein, B., Gerber, P. A., Edge, D. & Nielsen, M. C. E. Fluorescent light energy: A new therapeutic approach to effectively treating acne conglobata and hidradenitis suppurativa. Clin Case Rep 7, 1769‐1772 (2019). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6745390/
- Edge, D., Mellergaard, M. & Dam-Hansen, C. et al. Fluorescent light energy: The future for treating inflammatory skin conditions? J Clin Aesthet Dermatol 12, E61‐E68 (2019). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6561711/
- Ferroni, L., Zago, M., Patergnani, S., et al. Fluorescent light energy (FLE) acts on mitochondrial physiology improving wound healing. J Clin Med 9, 559 (2020). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7073965/
- Schwartz, R. Acne Conglobata Treatment & Management: Medical Care, Surgical Care, Consultations. Emedicine.medscape.com (2016). http://emedicine.medscape.com/article/1072716-treatment
- Habif, T. P. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 231 – 233 (2016). https://www.elsevier.com/books/clinical-dermatology/habif/978-0-323-26183-8
- Arndt, K. Manual of Dermatologic Therapeutics (7th Edition). 5 – 8 (LWW (PE), 2007).
- Nikolakis, G., Kyrgidis, A. & Zouboulis, C. C. Is there a role for antiandrogen therapy for hidradenitis suppurativa? A systematic review of published data. Am J Clin Dermatol 20, 503-513 (2019). https://pubmed.ncbi.nlm.nih.gov/31073704/
 Acne.org Products
Acne.org Products