Isotretinoin (Accutane®) Works Best for Severe Cystic Acne, but Comes with Serious Side Effects

The Essential Info
Cystic acne, also called nodulocystic acne, is acne that comes with large (over 5 mm in diameter), red, painful lesions called nodules and cysts that arise deep within the skin. These lesions can last for weeks, months, or even longer, and often scar the skin.
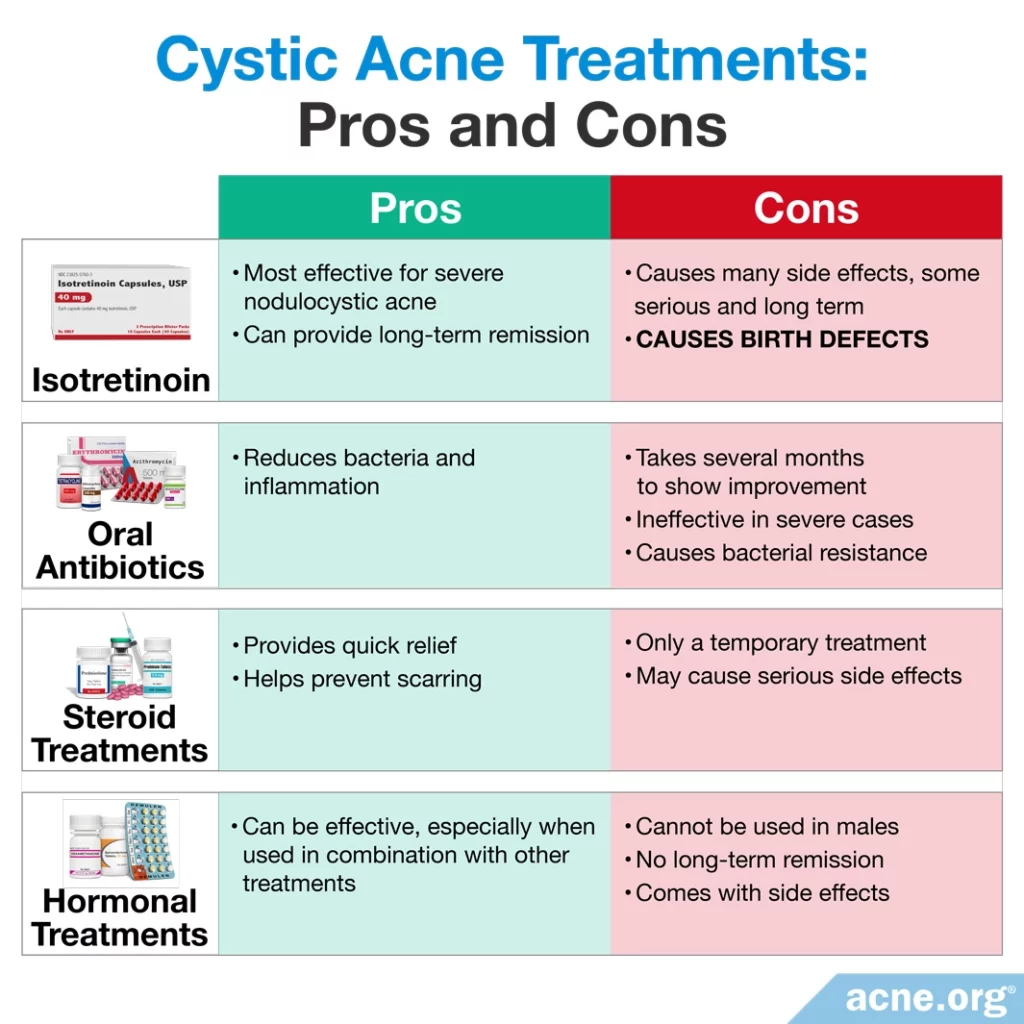
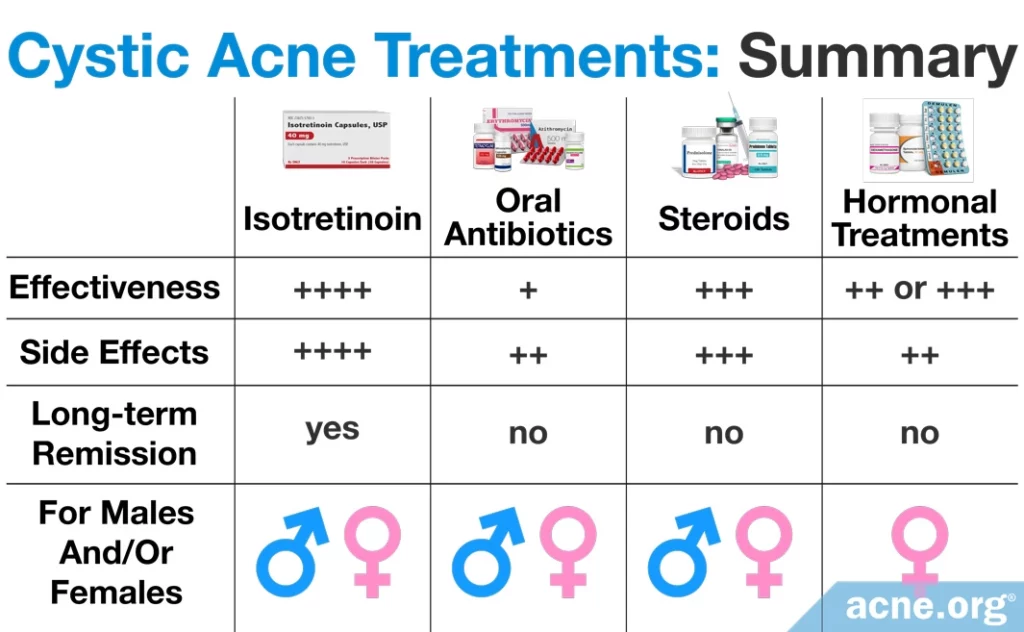
A proper topical regimen can sometimes keep nodulocystic acne in check, but when even this does not do the trick, there are four main therapies for cystic acne, and each has its pros and cons.
- Isotretinoin (Accutane®): Most effective but comes with major and potentially lifelong side effects
- Oral Antibiotics: Somewhat effective in some people in the short term, but with side effects
- Corticosteroids: Effective in the short term, but with side effects
- Hormonal Treatment [females only]: Moderately effective, but with side effects

The Science
Nodulocystic acne, normally known simply as “cystic acne,” when severe, can wreak havoc on the skin, causing permanent scarring. For this reason, it is vital that it be treated early and aggressively.
For many cases of cystic acne, proper application of benzoyl peroxide can calm the skin and keep the acne under control. But when the acne is extra severe, widespread, and/or scarring, sometimes other avenues can be explored. Let’s have a look at the most common treatments for cystic acne.
Isotretinoin
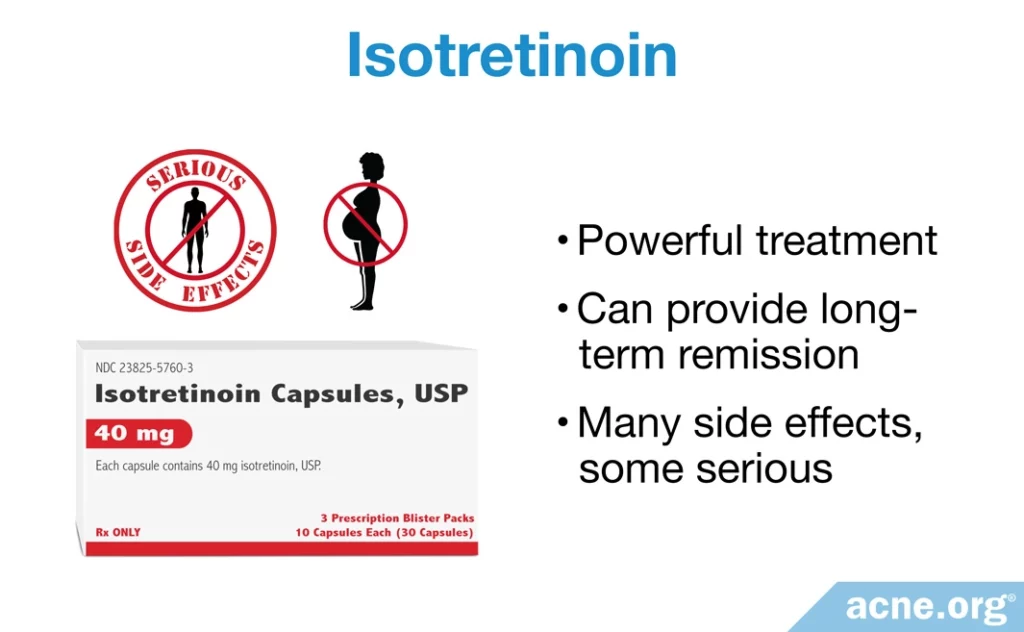
Isotretinoin, often known by its original brand name, Accutane®, is an oral medication that is proven to be the most effective treatment for nodulocystic acne. However, its power comes with serious side effects, some of which can be lifelong. It also causes serious birth defects and must never be used by women who are pregnant or plan to become pregnant.
After isotretinoin is swallowed, it enters the bloodstream and affects the entire body, including the skin. It works powerfully, and can permanently change the skin and body. This is why the Food and Drug Administration (FDA) approved it only for severe acne, and only after other options are exhausted.
Researchers believe that it clears acne primarily through decreasing the production of skin oil (sebum). Sebum is a major factor in the development of all acne, and by decreasing its production isotretinoin reduces the development of nodulocystic acne lesions.
The total duration of therapy is generally 15 – 20 weeks.1
Dosing depends on the weight of the patient, and studies are ongoing to determine an optimal dose, but all studies find that isotretinoin can reliably clear severe acne.
Expand to read details of studies

A 1979 study published in The New England Journal of Medicine examined the effectiveness of isotretinoin in 14 nodulocystic acne patients. Researchers performed this study by providing the patients 2 mg/kg of this medication every day for 4 months. The researchers found that it cleared the nodulocystic acne in 13 of the 14 patients studied. Nine of those 13 patients experienced clearing of acne by the end of the 4-month treatment; 3 of the 13 patients noticed clearing in 2 months post-treatment, and 1 of the 13 patients was clear in 10 months post-treatment. In the one patient whose acne persisted, isotretinoin decreased the number of lesions by 75%. Further, acne lesions on the face cleared faster than acne lesions on the chest and/or back. The researchers followed up with these 14 patients after 20 months post-treatment and found that 11 remained free of acne. They concluded that isotretinoin is exceptional at eliminating nodulocystic acne.2

A 1980 study published in the Journal of the American Academy of Dermatology examined whether the amount of isotretinoin prescribed affected its ability to clear nodulocystic acne. To perform this study, the researchers divided a group of 14 patients into 3 groups.
- Group 1 received 0.1 mg/kg of isotretinoin daily for 12 weeks. This group consisted of 5 patients.
- Group 2 received 0.5 mg/kg every day for 12 weeks. This group consisted of 5 patients.
- Group 3 received 1 mg/kg of isotretinoin daily for 12 weeks. This group consisted of 4 patients.
At the end of the 12-week study period, the researchers discovered that isotretinoin cleared nodulocystic acne at least somewhat in all 3 groups. The researchers observed clearing of acne lesions in 1 patient from group 1, in 3 patients from group 2, and in 2 patients from group 3. The lesions cleared fastest in group 3 patients, who received the highest dose. The researchers concluded that although every dose is effective at clearing acne, the highest dose clears the lesions the fastest. However, this may come with more severe side effects.3

A 1982 study published in the same journal examined the effectiveness of isotretinoin in 32 nodulocystic acne patients. The researchers performed this study by providing 32 patients a dosage of 0.5 mg/kg/day of isotretinoin for 4 months. In 6 patients who did not respond to this dose, the researchers increased it to a maximum of 1.2 mg/kg/day. At the end of the study, they found that 27 of the 32 nodulocystic acne patients receiving isotretinoin cleared all of their nodules and cysts. Eighteen of the 27 patients remained free of nodules and cysts for an average of 38 months post-treatment. Of the 5 patients whose acne did not resolve, they experienced 93% overall improvement in their acne, which increased to 97% improvement from 36 – 41 months post-isotretinoin treatment. This suggests that isotretinoin can continue clearing acne after the treatment period has ended. The researchers deduced that isotretinoin was remarkable at clearing nodulocystic acne and may be able to cure it.4

A 1984 study also published in the Journal of the American Academy of Dermatology examined the effectiveness of different isotretinoin doses to clear nodulocystic acne. To perform this study, the researchers divided 150 study participants into 3 groups.
- Group 1 received 0.1 mg/kg of isotretinoin daily for 20 weeks
- Group 2 received 0.5 mg/kg of isotretinoin daily for 20 weeks
- Group 3 received 1 mg/kg of isotretinoin daily for 20 weeks
At the end of the 20-week study period, the researchers found that isotretinoin cleared acne similarly in the patients of all 3 groups, suggesting that the lowest dose may be just as effective as the highest dose. However, the researchers did find differences in effectiveness after they examined the patients 12 – 18 months post-isotretinoin treatment. They found that only 10% of the group 3 patients, who received the highest dose of isotretinoin, relapsed and developed new nodulocystic acne lesions and needed a second treatment course, whereas 20% of group 2 patients and 42% of group 1 patients relapsed and needed a second treatment course of isotretinoin. Therefore, the researchers concluded that while 0.1 mg/kg/day treatment of isotretinoin may be enough to clear nodulocystic acne in a 5-month period, patients receiving a higher dose are more likely to stay free of acne.5

A 1988 study published in Clinical and Experimental Dermatology compared the effectiveness of isotretinoin to that of an antibiotic called dapsone normally used to treat leprosy. The researchers performed this study by dividing 40 nodulocystic acne patients into 2 groups.
- Group 1 received 40 mg of isotretinoin daily for 16 weeks
- Group 2 received 100 mg of oral dapsone daily for 16 weeks
The researchers found that the group receiving isotretinoin saw significant improvements in nodulocystic acne and a 55% reduction in sebum production. This reduction remained for 5 months post-treatment. However, the group receiving oral dapsone noticed only a slight improvement in nodulocystic acne and no change in sebum production. The researchers therefore concluded that isotretinoin was better at treating nodulocystic acne when compared to the oral antibiotic, dapsone.6

A 2019 study published in BioMed Research International examined the effectiveness of isotretinoin in treating severe nodulocystic acne that developed as a result of polycystic ovary syndrome (PCOS). Females with PCOS have a hormonal imbalance that typically results in acne as well as weight gain and excessive hair growth.
In this study, 40 women with PCOS and severe nodulocystic acne were treated with oral isotretinoin at a dose of 0.6 – 0.8 mg/kg/day for 6 months. This treatment significantly reduced the women’s acne, so that most had a final acne score of 0 – 0.75, indicating little to no acne. Surprisingly, isotretinoin also reduced excessive hair growth and improved hormone levels in the women with PCOS. The researchers wrote, “Solely isotretinoin administration may supply adequate healing in PCOS patients’ symptoms complicated with severe cystic acne.”7
Isotretinoin can not only clear existing nodules and cysts, but can prevent further breakouts. About 2/3 of people who take a course of isotretinoin experience long-term remission of acne.
A 4-month treatment plan using a generic form of isotretinoin can cost between $700 – $1400 for a patient weighing around 175 pounds (80 kilograms). Consequently, the cost can be prohibitive to some who cannot afford treatment.
In addition to the cost, isotretinoin comes with unwanted and severe side effects, some of which can be permanent. As an example of how worrisome its effects are on the body, the U.S. Air Force will not allow anyone who has ever taken isotretinoin to become a fighter pilot due to how it affects the eyes. Lifelong dry lips are also a common complaint, and joint pain may also stick around long term. These are only a few of the potential long-term side effects. Suffice it to say that taking isotretinoin is a very serious decision, and both the patient and doctor should carefully weigh the benefits against the short-term and life-term side effects.
Pregnant women should never take isotretinoin: Isotretinoin is the #1 birth-defect-causing medication on the market and causes catastrophic birth defects as well as miscarriage. Females taking isotretinoin must obtain at least two (2) negative pregnancy tests prior to starting treatment, and remain on at least two (2) forms of birth control for the duration of the treatment.8
Oral Antibiotics
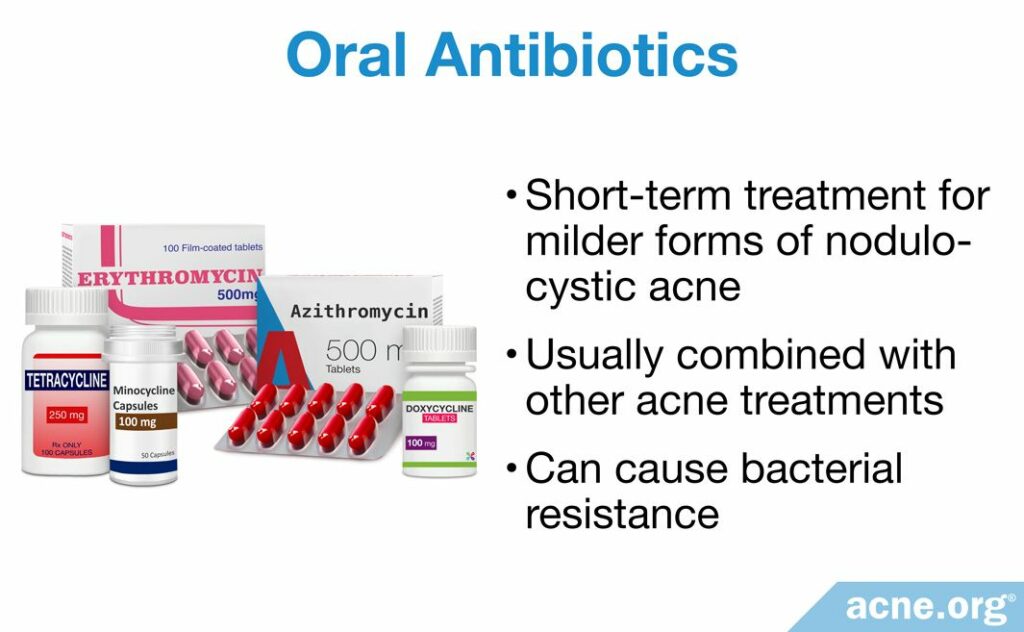
Oral antibiotics do not produce anywhere near the results of isotretinoin, only work in the short term, and only work for some people. However, they are a treatment option that can help reduce bacteria and inflammation. They should only be used for a maximum of 3 months, and are best used to treat people with only a few nodules or cysts.
Antibiotics are not as effective as isotretinoin and not as quick in producing results. However, they are more effective when combined with other acne treatments like topical benzoyl peroxide.9 There are 2 main antibiotic classes used in the treatment of acne:
- Tetracyclines: Tetracycline, doxycycline, and minocycline
- Macrolides: Azithromycin and erythromycin
Researchers have performed one study investigating the ability of oral antibiotics to clear cystic acne and one study investigating the side effects of oral antibiotics. Although they will need to perform more studies to confirm their findings, these studies have found that oral antibiotics are effective at temporarily reducing nodulocystic acne, but they cause side effects and are only a short-term treatment.
Expand to read details of studies

A 1994 study published in The Journal of Dermatology compared the effectiveness of oral tetracycline to that of gugulipid, which is a natural oral antibiotic made from the extract of an Indian medicinal plant, in treating nodulocystic acne. To perform this study, researchers separated 20 nodulocystic acne patients into 2 groups.
- Group 1 received 500 mg of tetracycline twice daily for three months
- Group 2 received 25 mg of gugulipid twice daily for three months
The researchers found that group 1 had a 65.2% reduction in nodulocystic acne, while group 2 experienced a 68% reduction in nodulocystic acne. Because of this, the researchers stated that gugulipid may be slightly advantageous over tetracycline at treating nodulocystic acne. However, it was clear from the research that tetracycline was also highly effective in reducing nodulocystic acne.10
A 2014 book chapter published in the Saunders Nursing Drug Handbook listed several side effects of oral antibiotics used as nodulocystic acne treatment. These side effects include:
- Gastrointestinal problems, including diarrhea, nausea, and abdominal pain, are associated with any antibiotic, but are often seen with doxycycline and the macrolide classes of antibiotics
- Vaginal yeast infections and rashes are a potential side effect from any antibiotic, including those used to treat acne
- Photosensitivity, which is increased sensitivity to the sun’s ultraviolet (UV) rays, is a side effect of the tetracycline class of antibiotics. People taking doxycycline are particularly photosensitive.
- Dizziness is a potential side effect from minocycline use.
- Tinnitus, which is a disorder that causes a constant ringing in the ears, is associated with minocycline use.8
- Pseudotumor cerebri, which is increased pressure in the skull, is a particularly dangerous side effect that can occur if oral tetracycline is used with isotretinoin. Therefore, oral tetracycline and isotretinoin should not be taken together.11
Another problem with antibiotic treatments for acne is that oral antibiotics can be used for only 3 to 6 months. Further, long-term use of oral antibiotics can cause bacteria to develop resistance to the drug, making it useless. Antibiotics can only temporarily reduce nodulocystic acne lesions, and other treatments are necessary to clear the acne for extended periods of time.8
Steroid Treatments
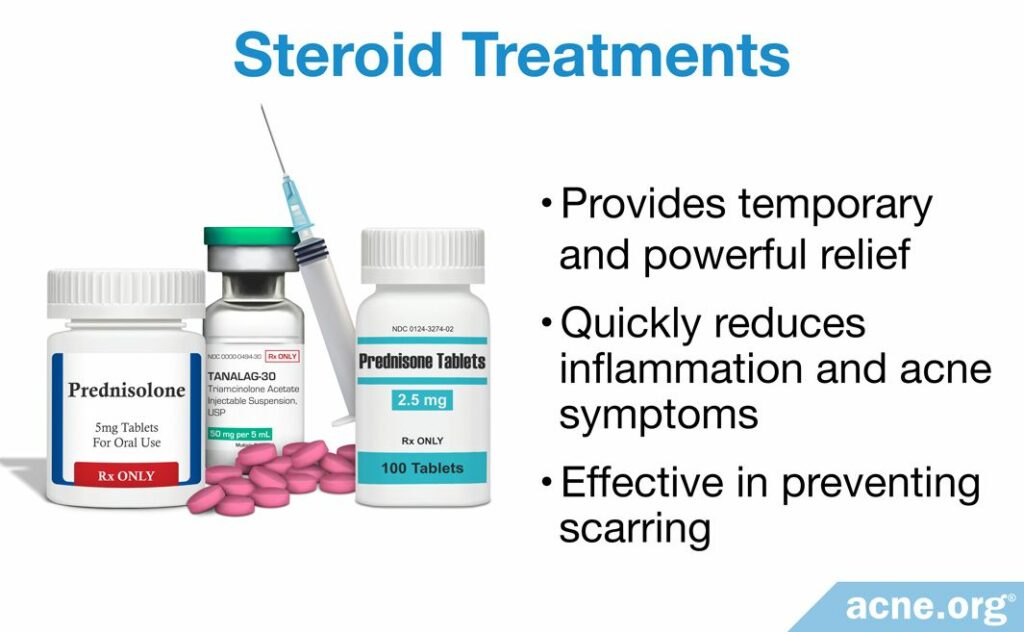
In the case of severe cystic acne, steroid treatments, such as oral prednisone, are a short-term treatment that can quickly reduce inflammation.
These steroids, called corticosteroids, are different from anabolic steroids, which bodybuilders use. Doctors will sometimes administer oral corticosteroids initially to a patient who presents with severe acne in order to reduce inflammation and quickly reduce acne symptoms. Then, isotretinoin can be given to clear up the acne in the long term.
There are 2 studies that confirm the effectiveness of oral corticosteroids, and 1 study that confirms the effectiveness of injected steroids, which I’ll mention next.
Injected corticosteroids (cortisone shots): Doctors commonly inject steroids, such as cortisone, directly into a nodule or cyst in order to reduce the inflammation and heal the nodule or cyst quickly. A reduction in swelling can be seen almost immediately and healing begins. If you only get a cystic acne lesion once in a while, don’t hesitate to make a quick appointment with your dermatologist for a cortisone shot.
Expand to read details of studies

A 1993 study published in Acta Dermato-Venereologica examined the effectiveness of a steroid treatment combined with an oral antibiotic to clear nodulocystic acne. The researchers divided the participants into 2 groups to perform this study.
- Group 1 received a combination of oral prednisolone (steroid hormone) and erythromycin (macrolide antibiotic). This group consisted of 6 nodulocystic acne patients in this group.
- Group 2 received a combination of isotretinoin and erythromycin. This group consisted of 6 nodulocystic acne patients.
The researchers found that after 4 weeks, the treatment plans of both groups cleared nodulocystic acne in 5 of 6 patients. However, when the patients in the first group stopped taking prednisone, 2 of the 5 patients relapsed in nodules and cysts. In the isotretinoin-treated group, 1 patient needed prednisolone because the acne worsened, and he/she even developed ulcers (ruptures of the skin that look like severe wounds). The researchers concluded that although not ideal for every person, the best combination of medications to treat early stages of cystic acne is prednisolone and erythromycin. However, in order to achieve long-term results, the researchers went on to say that isotretinoin should be taken.13

A 1984 study published in the British Journal of Dermatology compared 4 treatment regimens in patients with acne fulminans, which is an especially severe form of nodulocystic acne that also comes with symptoms including fever and joint pain. The 4 treatment groups were as follows.
- Group 1 received oral and topical antibiotics daily for several months, which resulted in clearance of cystic acne in addition to other acne fulminans symptoms. Although the oral antibiotics worked well to clear acne, they generally did not do so quickly and took on average 42 weeks to achieve 75% clearance of acne. It also took around 9 weeks to clear other acne fulminans symptoms.
- Group 2 received oral antibiotics in combination with oral prednisolone, a corticosteroid hormone, for several months. The prednisolone dose was reduced over a 6-week period. This combination took 45 weeks to clear 75% of acne lesions, but only 3 weeks to clear other acne fulminans symptoms.
- Group 3 received isotretinoin for 16 – 20 weeks combined with oral prednisolone from the 4th – 6th week for 6 weeks. This treatment regimen took 18 weeks to clear 75% of acne, and 8 weeks to clear other acne fulminans symptoms.
- Group 4 received oral prednisolone for 6 weeks combined with isotretinoin from the 3rd – 6th week for 16 – 20 weeks. This treatment regimen took 18 weeks to achieve 75% clearance of acne, but only 1 week to clear other symptoms of acne fulminans.
The researchers concluded that the preferred treatment protocol was group 4, which received oral prednisolone for 6 weeks in combination with isotretinoin for 16 – 20 weeks.14

A 1983 study published in the Archives of Dermatology investigated the effectiveness of injecting corticosteroid hormones directly into the nodules or cysts. This type of procedure is called an intralesional injection because the corticosteroid is injected directly into the lesion. The researchers found that an injection of the corticosteroid, triamcinolone acetate, was effective at resolving nodules and cysts. However, intralesional shots are effective only when clearing one or a few particularly stubborn nodules or cysts. Corticosteroid injections are not recommended when numerous nodules or cysts are present on the skin.8,15
Hormonal Treatments
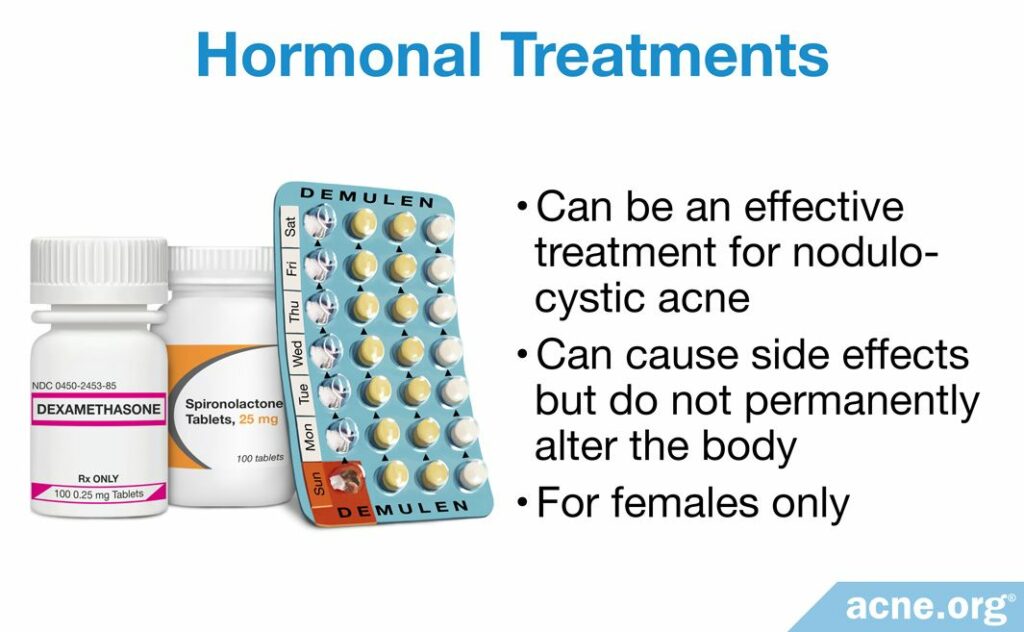
While not as effective as isotretinoin, hormonal treatments like oral contraceptives (birth control pills) and anti-androgens (such as spironolactone) do produce reliable effectiveness.
Hormonal treatments cause side effects, but do not permanently alter the body like isotretinoin does.
Only females can use them because hormonal treatments in males can cause breast growth and problems with sexual function.
Researchers have performed several studies to identify the effectiveness of hormonal treatments for nodulocystic acne and have found that they can help reduce nodulocystic acne.
Expand to read details of studies

A 1983 study published in the New England Journal of Medicine examined 2 hormonal treatments for their ability to clear nodulocystic acne. To perform this study, the researchers divided the patients into 2 groups.
- Group 1 received either dexamethasone, which is a corticosteroid hormone, or Demulen, which is an oral contraceptive, or both daily for 6 months. This group consisted of 59 females.
- Group 2 received dexamethasone daily for 6 months. This group consisted of 32 males.
After six months, the researchers found that 97% of females and 81% of males had clear skin. They concluded that dexamethasone and Demulen are effective at clearing nodulocystic acne.12

A 1984 study published in the British Journal of Dermatology examined the effectiveness of the hormonal treatment, spironolactone, on clearing acne. Spironolactone works by preventing androgens from working properly. Androgens are male hormones, found in both males and females. Researchers have found that higher levels of androgens normally correspond with more acne and more severe acne. Therefore, by blocking androgens, spironolactone may prevent acne. However, spironolactone can cause side effects, especially in males, including breast growth and decreased sex drive. To perform this study, the researchers provided 100 – 200 mg of spironolactone to 13 males and 13 females with acne. At least 3 of these patients had nodulocystic acne, but the researchers did not describe the type of acne in the other 23 patients. At the end of the study, the study conductors found that 67% of females and 83% of males receiving at least 100 mg of spironolactone daily had improvement of their acne. However, the most acne improvement occurred in 3 of the 4 patients receiving 200 mg daily. These 3 patients had nodulocystic acne that had not responded well to other treatments, including oral antibiotics. Due to the small number of study participants, the researchers were not able to draw conclusions regarding the effectiveness of spironolactone on nodulocystic acne. However, the results from this study warrant future research investigating its effectiveness on this form of acne.16,17
References
- Zaenglein, A. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol 1 – 29 (2016). https://www.ncbi.nlm.nih.gov/pubmed/26897386
- Peck, G. et al. Prolonged Remissions of Cystic and Conglobate Acne with 13-cis-Retinoic Acid. New Engl J Med 300, 329 – 333 (1979). https://www.ncbi.nlm.nih.gov/pubmed/153472
- Farrell, L., Strauss, J. & Stranieri, A. The treatment of severe cystic acne with 13-cis-retinoic acid. J Am Acad Dermatol 3, 602 – 611 (1980). https://www.ncbi.nlm.nih.gov/pubmed/6451637
- Peck, G. et al. Isotretinoin versus placebo in the treatment of cystic acne. J Am Acad Dermatol 6, 735 – 745 (1982). https://www.ncbi.nlm.nih.gov/pubmed/6461677
- Strauss, J. et al. Isotretinoin therapy for acne: Results of a multicenter dose-response study. J Am Acad Dermatol 10, 490 – 496 (1984). https://www.ncbi.nlm.nih.gov/pubmed/6233335
- Prendville, J. et al. A comparison of dapsone with 13-cis retinoic acid in the treatment of nodular cystic acne. Clin Exp Dermatol 13, 67 – 71 (1988). https://www.ncbi.nlm.nih.gov/pubmed/2975199
- Acmaz, G., Cınar, L., Acmaz, B. et al. The effects of oral isotretinoin in women with acne and polycystic ovary syndrome. Biomed Res Int 2019, 2513067 (2019). https://pubmed.ncbi.nlm.nih.gov/31080813/
- Hodgson, B. & Kizior, R. Saunders nursing drug handbook 2012. (W. B. Saunders Co., 2014).
- Habif, T. P. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 231 – 233 (2016). https://www.elsevier.com/books/clinical-dermatology/habif/978-0-323-26183-8
- Thappa, D. & Dogra, J. Nodulocystic Acne: Oral Gugulipid versus Tetracycline. J Dermatol 21, 729 – 731 (1994).
- Acne Conglobata Treatment & Management, https://emedicine.medscape.com/article/1072716-treatment
- Marynick, S. et al. Androgen Excess in Cystic Acne. New Engl J Med 308, 981 – 986 (1983). https://www.ncbi.nlm.nih.gov/pubmed/6220224
- Karvonen, S. Systemic corticosteroid and isotretinoin treatment in cystic acne. Acta Dermato-Venereol 73, 452 – 455 (1993). https://www.ncbi.nlm.nih.gov/pubmed/7906462
- Seukeran, D. C. & Cunliffe, W. J. The treatment of acne fulminans: a review of 25 cases. Br J Dermatol 141, 307 – 309 (1999). https://www.ncbi.nlm.nih.gov/pubmed/10468806
- Levine, R. Intralesional corticosteroids in the treatment of nodulocystic acne. Arch Dermatol 119, 480 – 481 (1983). https://www.ncbi.nlm.nih.gov/pubmed/6222700
- Tobechi, L. et al. Hormonal treatment of acne in women. J Clin Aesthet Dermatol 2, 16 – 22 (2009). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2923944/
- Goodfellow, A. et al. Oral spironolactone improves acne vulgaris and reduces sebum excretion. Br J Dermatol 111, 209 – 214 (1984). https://www.ncbi.nlm.nih.gov/pubmed/6235834
 Acne.org Products
Acne.org Products