It Can Help Females, but There Are Limitations Regarding Women Who Are Pregnant or Breastfeeding

The Essential Info
In both males and females, hormones play a significant role in acne, specifically hormones called androgens, which are male hormones found in both males and females.
There’s not much that boys and men can do about these hormones, because hormonal treatments can cause feminization of the male body, including breast growth, as well as other undesirable side effects.
However, doctors sometimes prescribe hormonal treatment to girls and women, as long as they are not pregnant or breastfeeding.
Hormonal treatments reduce the amount of androgens, which in turn decreases skin oil production, and ultimately reduces acne symptoms.
Treatments include:
- Combined oral contraceptives (COCs), otherwise known as birth control pills (most common – reliably reduces acne by about 60%)
- Cyproterone acetate (CPA)
- Spironolactone
- Flutamide
- GnRH agonists
Because hormonal treatments are oral treatments, they affect the entire body and can come with a wide array of side effects. It’s important to consult your physician about hormonal treatments and educate yourself as much as possible on the risks.

The Science
- Hormonal Treatments for Acne
- Combined Oral Contraceptives (COCs)
- Cyproterone Acetate
- Spironolactone
- Flutamide
- GnRH Agonists
Acne is a hormonal disease, and this is why we see it rear its head during puberty, when hormonal production goes into overdrive.
Each of these hormones plays a different role in acne:
- Androgens (male hormones present in both males and females): More androgens normally means more skin oil (sebum) production, and in turn, more acne. High levels of androgens are associated with acne in both males and females.
- Estrogens (female hormones present in both males and females): More estrogens normally means less sebum production, and in turn, less acne. Estrogens also may reduce inflammation.
- Progesterone (hormone present in both males and females): May play a role in fluctuating levels of sebum during the menstrual cycle. This is a matter of debate among researchers.1-4
Hormonal Treatments for Acne
Because acne is a hormonal disease, treatments that address hormone levels in the body can help alleviate symptoms. Available hormonal treatments include:
- Combined oral contraceptives (COCs), otherwise known as birth control pills
- Cyproterone acetate (CPA)
- Spironolactone
- Flutamide
- GnRH agonists
Let’s have a look at the effectiveness and side effects of each, starting with by far the most commonly prescribed hormonal treatment for acne, combined oral contraceptives (COCs).
Combined Oral Contraceptives (COCs)

Combined oral contraceptives (COCs) are birth control pills that contain both:
- Ethinyl estradiol (synthetic estrogen)
- Progestin (synthetic progesterone)
In addition to preventing pregnancy, the estrogen in COCs reduces sebum and may reduce the level of androgens, both of which reduce acne symptoms. The role of progestin in COCs is not understood as is that of estrogen and appears to vary somewhat according to the type of progestin.5
There are several types of progestin that can be present in COCs, including:
- Cyproterone acetate (CPA)
- Chlormadinone
- Drospirenone
- Derivatives of 19-nortestosterone, such as norethindrone, levonorgestrel, norgestrel, desogestrel, norgestimate, and gestodene5
There are many COCs on the market. In the United States, the Food and Drug Administration (FDA) has approved three COCs for acne treatment:
- Ortho Tri-Cyclen® – contains norgestimate
- Estrostep® – contains norethindrone
- YAZ® – contains drospirenone
However, just because these brands are approved for acne does not mean they are superior to other COCs. It’s notable that other countries have also approved other COCs for acne.5 In other words, research shows us that all COCs help reduce acne.
Effectiveness: Regardless of which ones are approved in any particular country, all COCs show evidence of effectively treating acne in women.

A 2012 systematic review (a rigorous literature review that pools the results of many studies) concluded that all COCs resulted in a significant reduction of acne lesions and acne severity. The review concluded also that COCs containing CPA appeared to be more effective than the other progestins studied, but the evidence for this was limited.5

A 2014 meta-analysis (another rigorous literature review that pools the results of many studies and combines them into a single analysis) compared the effectiveness of COCs with a placebo. This meta-analysis found that after three months of COC treatment, there was a 35% reduction in acne lesions, and after six months of treatment, there was a 55% – 60% reduction.6
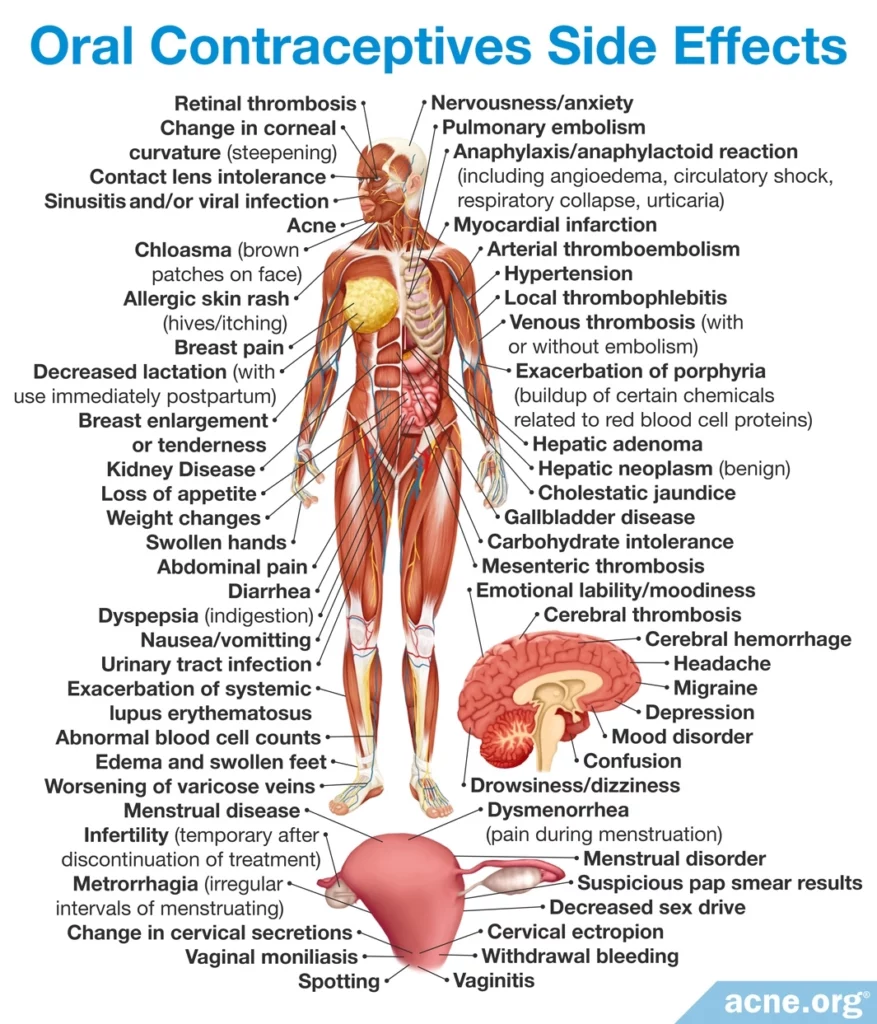
Side effects: The most serious side effects of COCs are thromboembolisms, which is a type of blood clot that can cause severe problems and even death. Therefore, COC-use is not advised in women with predisposing factors that raise their risk of a thromboembolism, such as genetic clotting disorders, previous thromboembolisms, heart disease, high blood pressure, obesity, smoking in women older than 35 years of age, diabetes, liver disease, migraine and headache, prolonged immobilization, such as long-term bed rest, history of breast, endometrial, or liver cancer, pregnancy and breastfeeding, or hypersensitivity to any ingredient in a COC.5
Other safety concerns are related to the estrogen in COCs and include breast tenderness, heart disease, headache, nausea, blood clotting problems, and risk of uterus and breast cancers. Newer COCs that contain a lower dose of estrogen carry a lower risk of these side effects.5
Finally, combining a COC with an antibiotic may reduce the effectiveness of the COC if it is used for birth control. There is some evidence that doxycycline and tetracycline, which are commonly used for acne, do not affect the effectiveness of COCs. However, if you are trying to prevent pregnancy, it is wise to employ a second method of birth control when taking any antibiotic with a COC.5
Cyproterone Acetate
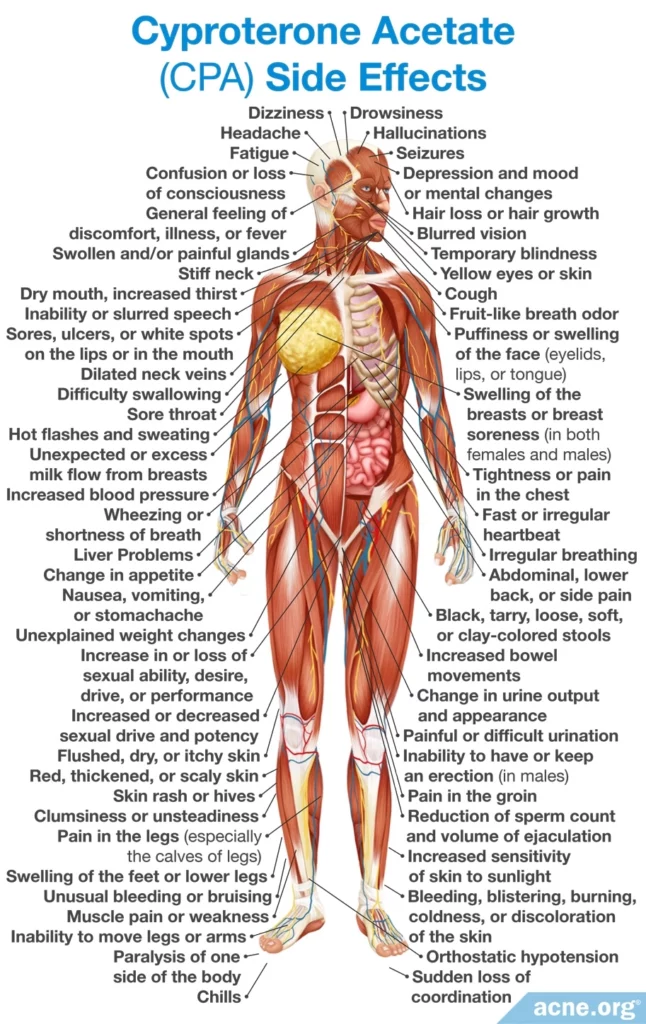
Cyproterone acetate (CPA) is a progestin that is often present in a COC, and is sometimes, albeit rarely, prescribed on its own. Cyproterone acetate works as an anti-androgen: it blocks androgen receptors and decreases the production of androgens. Because of these effects, cyproterone acetate may cause feminization and other issues in males. It also cannot be used in pregnant women.5,7
Effectiveness: I’ll just talk about studies based on CPA when it is prescribed on its own because when prescribed as part of a COC, it produces results on par with other COCs. Based on two studies performed in the 1990s, CPA used alone in the recommended dose of 50 – 100 mg per day can result in 75% – 90% improvement in acne within three months.5
Side effects: The most common side effects of CPA are irregularity in the menstrual cycle, breakthrough bleeding (bleeding between periods), breast tenderness, headache, and nausea. However, these side effects typically are temporary or go away with time. Using CPA in a COC rather than alone significantly reduces the menstrual side effects.5
A less common but more concerning side effect of CPA is liver damage. This is dose-dependent, meaning that higher doses carry more risk.5
Spironolactone

Spironolactone is a derivative of a natural hormone called aldosterone. Spironolactone is an anti-androgen, so it cannot be used in males or in pregnant women.5,7
Effectiveness: So far, rigorous scientific evidence on the effectiveness of spironolactone is still lacking. Two systematic reviews, one from 2009 and a more recent one from 2017, concluded that the small number of studies performed to date included too few patients to prove that spironolactone works for acne.8 Even so, a few more recent studies have shown impressive effectiveness. The review authors also noted that we should take doctors’ experience into account, and doctors will usually tell you that in the real world, spironolactone does work to improve acne.
Expand to read details of 2017 systematic review

This systematic review was published in the American Journal of Clinical Dermatology. The authors looked at 10 clinical trials and 21 case studies on spironolactone. They concluded there is not enough rigorous evidence to show that spironolactone is effective against acne at the doses doctors typically prescribe. They noted that higher doses, such as 200 mg per day, seem to be effective against acne, but doctors are hesitant to prescribe such high amounts due to the increased risk of side effects. In conclusion, the authors wrote, “Prescribing recommendations must continue to rely on consensus and expert opinion until high-quality evidence becomes available.”8 In other words, if doctors’ experience suggests that spironolactone works, that’s the best information we have to go on for now.
Doctors have been using spironolactone for more than 30 years to treat hormone-related skin diseases, such as acne, including acne on the face and body. And we now have 4 more studies that have been released since 2017. All 4 of these studies found that 71% – 86% of female patients improve on spironolactone.10-13
Expand for details of these 4 studies

The first 2017 study was published in the journal Dermatology. The researchers looked through the medical records of 400 female acne patients who had been treated with spironolactone during the preceding four years. Of these, 253 patients started taking spironolactone after trying other acne treatments, and 147 patients took spironolactone as their first and only acne treatment.
The researchers found that 86% of the patients experienced an improvement in acne after taking spironolactone. The study authors wrote, “The vast majority of our patients improved on spironolactone, despite many previously failing other acne treatments.”10

The second 2017 study was published in the European Journal of Dermatology. As in the previous study, the researchers went through past medical records of women with acne. They came up with 70 women who took 150 mg or less of spironolactone per day for an average of 6 months. The researchers found that for 71% of the women, spironolactone was effective at reducing acne.11
The third 2017 study was published in the International Journal of Women’s Dermatology. Like the previous two studies, this study relied on past medical records of female patients. Out of 110 female patients, 85% experienced an improvement in acne after taking spironolactone. On average, the women’s acne improved by 73% on the face, 76% on the chest, and 78% on the back after taking spironolactone.
However, the researchers noted that some of the women took other acne medications at the same time as spironolactone, making it difficult to be sure that spironolactone alone was responsible for the improvement. The scientists highlighted the need for studies testing spironolactone on new patients in a controlled manner instead of using past medical records.12

Finally, a study published in 2021 in the Journal of American Academy of Dermatology also looked at the medical records of 403 adult women that had taken spironolactone. In line with the previous studies, the researchers found that the majority of women treated with 100 mg of spironolactone experienced a reduction in acne severity or even complete clearing of acne. Facial acne improved in 75.5% of women, chest acne in 84% of women, and back acne in 80.2% of women. The majority of these patients had taken spironolactone for about 16 months (470 days) before stopping.13
However, this was another retrospective study that looked at past medical records, so there is still a need for studies testing spironolactone on new patients in a controlled manner.
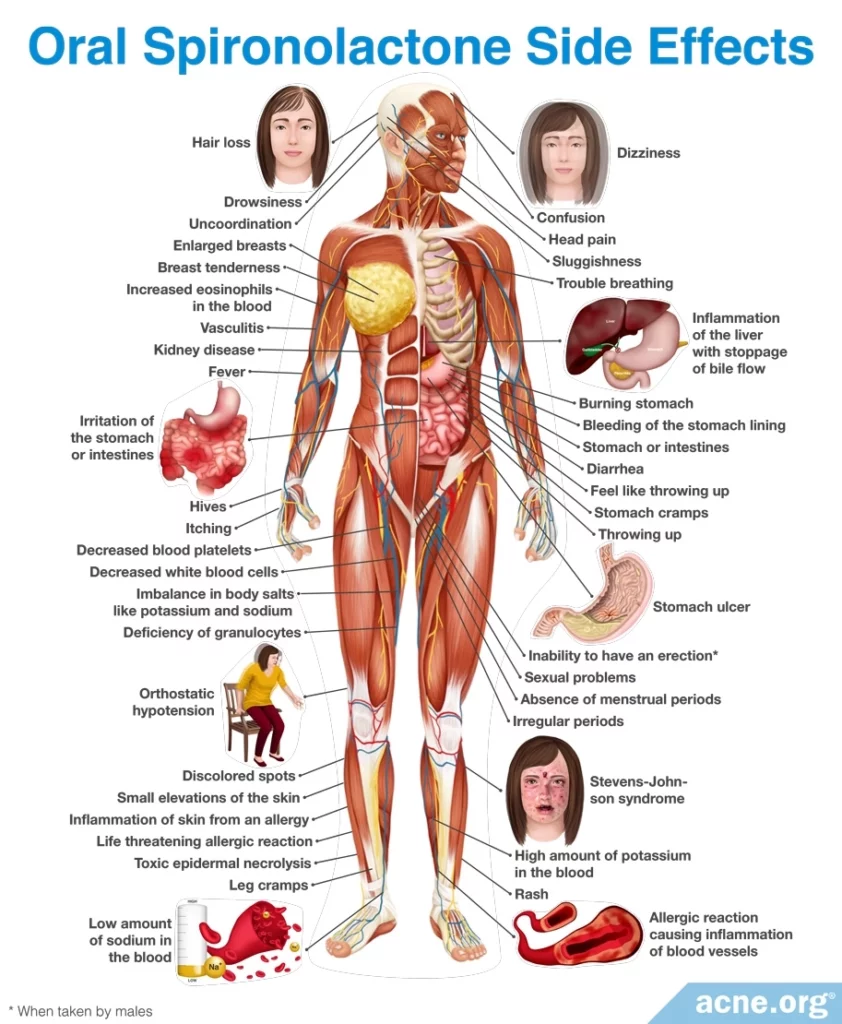
Side effects: Spironolactone can cause menstrual irregularities and tenderness or enlargement of the breasts. However, these side effects typically are mild and more common at higher doses. In addition, spironolactone can cause a high potassium level in the bloodstream, though this is not much of a concern in young, healthy acne patients. Nevertheless, people taking spironolactone should avoid taking ACE-inhibitors (a type of high blood pressure medication) or potassium supplements.5,7 To reduce potential side effects, doctors normally recommend starting with a low dose of spironolactone, such as 25 mg/day, and then slowly increasing the dose if necessary. The highest dose of spironolactone used to treat acne is 200 mg/day.14
Flutamide

Flutamide is an anti-androgen that is used to treat prostate cancer. It works by blocking androgen receptors.5,7
Effectiveness: A 2011 clinical trial indicated that flutamide was as effective as COCs containing CPA in treating acne lesions. However, the authors suggested that their results should be confirmed in future studies with larger numbers of patients.15
Another 2011 study looked at past medical records of women who had taken flutamide, and found that the women’s acne had improved by 80% on average after 6 months of treatment. Women who continued taking flutamide for several years stayed almost completely clear of acne.16
Other studies also indicate that at the standard dose of 62.5 – 500 mg per day, flutamide can result in an 80% improvement in acne.5 Some research suggests that with long-term use, the lowest dose of 62.5 mg/day may be enough to maintain the results.16
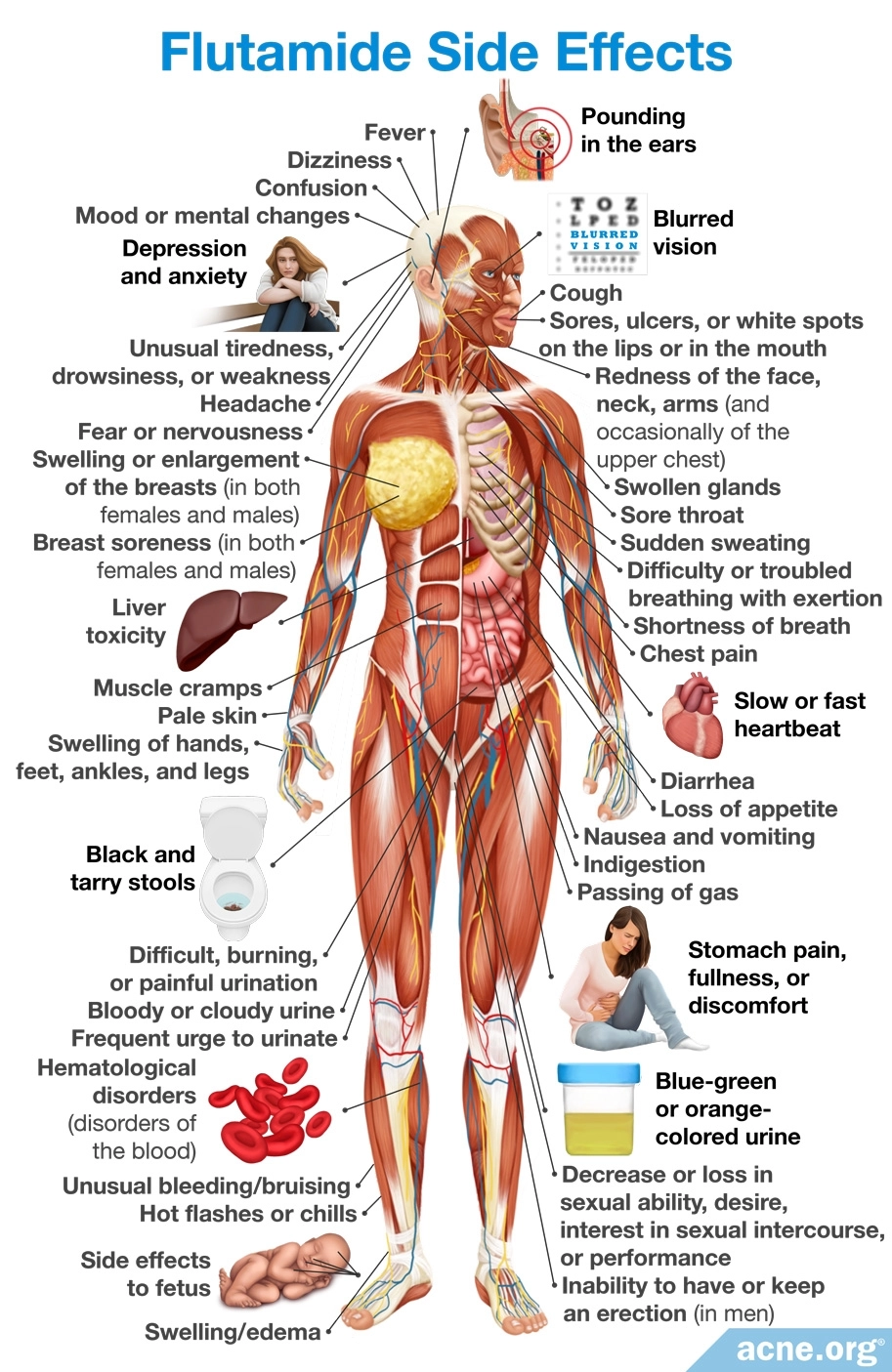
Side effects: The most concerning side effect of flutamide is liver toxicity, which appears to be related to dose and older age. Because of this, researchers advise starting with a low dose and increasing the dose only if necessary.

According to a 2015 article in the British Journal of Dermatology, “Monitoring of liver function is mandatory [when taking flutamide] as cases of fatal [liver toxicity] have been reported.”5
Other side effects include diarrhea, hematological disorders (disorders of the blood), muscle cramps, and breast enlargement.9 Like other anti-androgens, it cannot be taken during pregnancy.5
GnRH Agonists

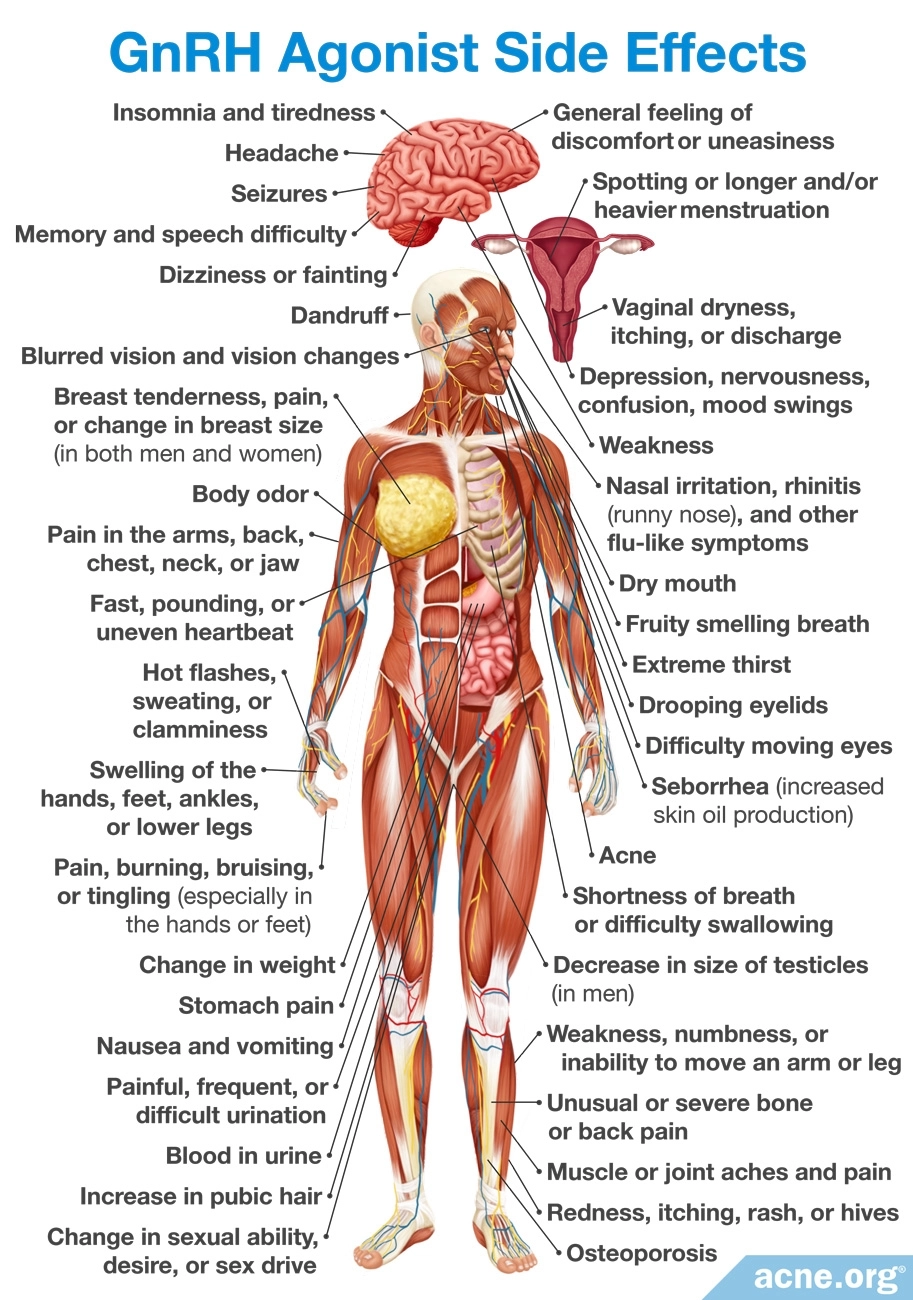
Gonadotropin-releasing hormone agonists (GnRH agonists), such as buserelin, nafarelin, and leuprolide, suppress hormones that stimulate androgen production. These medicines are reserved for women who do not respond to or who cannot tolerate COCs.5
Effectiveness: There is some evidence that GnRH agonists may help treat acne, but their use is limited because of high costs. In addition, there are no controlled trials of GnRH agonists–partly because of the high cost and partly because they can cause menopausal symptoms.5,7
Side effects: While GnRH agonists suppress androgens, they also suppress the production of estrogens. The lack of estrogen may lead to menopausal symptoms, such as bleeding, osteoporosis, and flushing. GnRH agonists cannot be used during pregnancy, breastfeeding, or if there is vaginal bleeding unrelated to periods.7,17
References
- Raghunath, R. S., Venables, Z. C. & Millington, G.W. The menstrual cycle and the skin. Clin Exp Dermatol 40, 111 – 115 (2015). https://www.ncbi.nlm.nih.gov/pubmed/25683236
- Farage, M. A., Neill, S. & MacLean, A. B. Physiological changes associated with the menstrual cycle: a review. Obstet Gynecol Surv 64, 58 – 72 (2009). https://www.ncbi.nlm.nih.gov/pubmed/19099613
- Arora, M. K., Yadav, A. & Saini, V. Role of hormones in acne vulgaris. Clin Biochem 44, 1035 – 1040 (2011). https://www.ncbi.nlm.nih.gov/pubmed/21763298
- Lam, C. L. & Zaenglein, A. L. Contraceptive use in acne. Clin Dermatol 32, 502 – 515 (2014). https://www.ncbi.nlm.nih.gov/pubmed/25017461
- Bettoli, V., Zauli, S. & Virgili, A. Is hormonal treatment still an option in acne today? Br J Dermatol 172 suppl 1, 7 – 46 (2015). https://www.ncbi.nlm.nih.gov/pubmed/25627824
- Koo, E. B., Petersen, T. D. & Kimball, A. B. Meta-analysis comparing efficacy of antibiotics versus oral contraceptives in acne vulgaris. J Am Acad Dermatol 71, 450 – 459 (2014). https://www.ncbi.nlm.nih.gov/pubmed/24880665
- Katsambas, A. D. & Dessinioti, C. Hormonal therapy for acne: why not as first line therapy? Facts and controversies. Clin Dermatol 28, 17 – 23 (2010). https://www.ncbi.nlm.nih.gov/pubmed/20082945
- Layton, A. M., Eady, E. A., Whitehouse, H., Del Rosso, J. Q., Fedorowicz, Z. & van Zuuren, E. J. Oral spironolactone for acne vulgaris in adult females: A hybrid systematic review. Am J Clin Dermatol 18, 169-191 (2017). https://pubmed.ncbi.nlm.nih.gov/28155090/
- Husein-Elahmed, H. Management of acne vulgaris with hormonal therapies in adult females. Dermatol Ther 28, 166 – 172 (2015). https://www.ncbi.nlm.nih.gov/pubmed/25845307
- Grandhi, R,. & Alikhan, A. Spironolactone for the treatment of acne: A 4-year retrospective study. Dermatology 233, 141-144 (2017). https://pubmed.ncbi.nlm.nih.gov/28472793/
- Isvy-Joubert, A., Nguyen, J. M., Gaultier, A. et al. Adult female acne treated with spironolactone: a retrospective data review of 70 cases. Eur. J. Dermatol. 27, 393 – 398 (2017). https://www.ncbi.nlm.nih.gov/pubmed/28862134
- Charny, J. W., Choi, J. K. & James, W. D. Spironolactone for the treatment of acne in women, a retrospective study of 110 patients. Int. J. Womens Dermatol. 3, 111 – 115 (2017). https://www.ncbi.nlm.nih.gov/pubmed/28560306
- Garg, V., Choi, J. K, James, W. D. & Barbieri, J. S. Long-term use of spironolactone for acne in women: A case series of 403 patients. J. Am. Acad. Dermatol. 84, 1348-1355 (2021). https://pubmed.ncbi.nlm.nih.gov/33434594/
- Searle, T. N., Al-Niaimi, F. & Ali, F. R. Spironolactone in dermatology: uses in acne and beyond. Clin. Exp. Dermatol. 45, 986-993 (2020). https://pubmed.ncbi.nlm.nih.gov/32844462/
- Adalatkhah, H., Pourfarzi, F. & Sadeghi-Bazargani, H. Flutamide versus a cyproterone acetate-ethinyl estradiol combination in moderate acne: a pilot randomized clinical trial. Clin Cosmet Investig Dermatol 4, 117-121 (2011). https://pubmed.ncbi.nlm.nih.gov/21833162/
- Paradisi, R., Fabbri, R., Porcu, E., Battaglia, C., Seracchioli, R. & Venturoli, S. Retrospective, observational study on the effects and tolerability of flutamide in a large population of patients with acne and seborrhea over a 15-year period. Gynecol. Endocrinol. 27, 823-829 (2011). https://pubmed.ncbi.nlm.nih.gov/21117864/
- Elsaie, M. L. Hormonal treatment of acne vulgaris: un update. Clin Cosmet Investig Dermatol 9, 241 – 248 (2016). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5015761/
 Acne.org Products
Acne.org Products