Are Some Worse Than Others?

The Essential Info
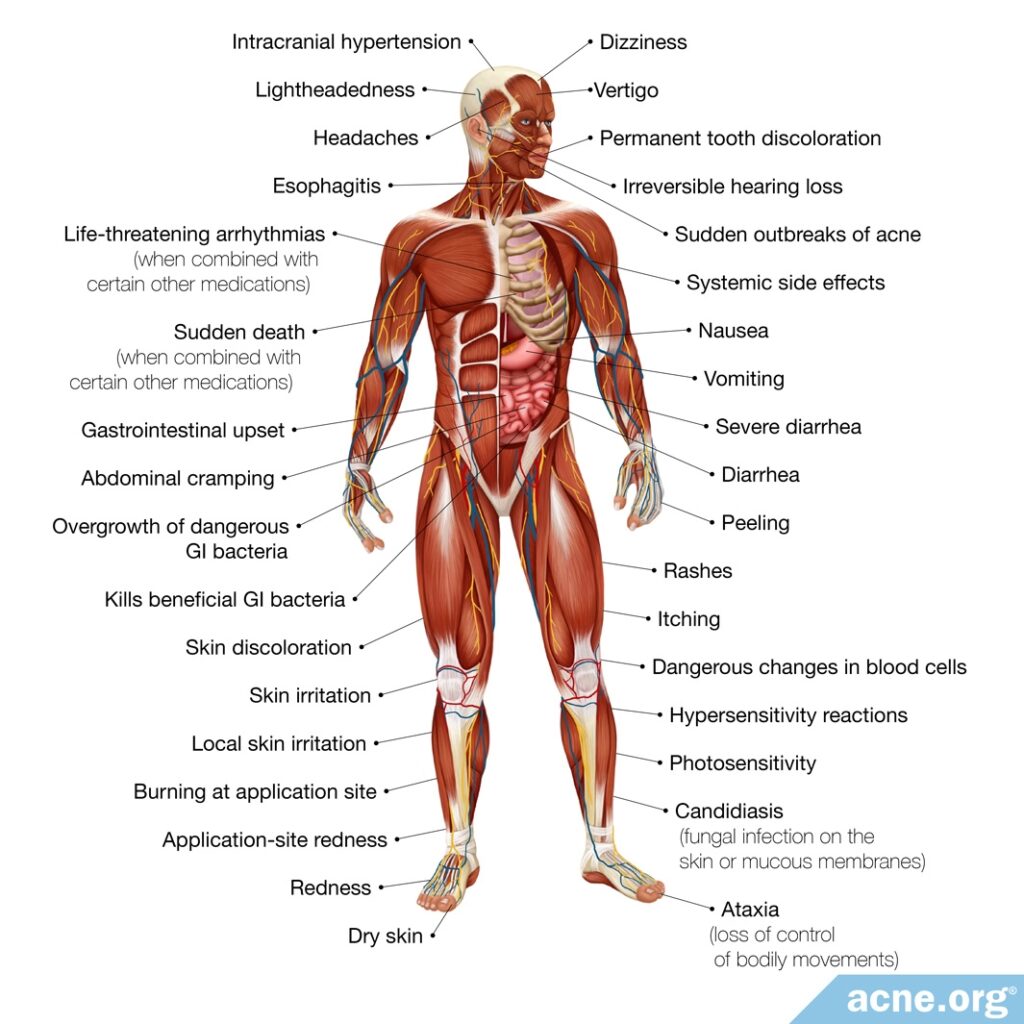
Topical antibiotics often produce skin irritation, and oral antibiotics are well known to produce gastrointestinal upset and nervous system problems, and sometimes more serious lifelong side effects like permanent tooth discoloration, hearing loss, or death.
Despite these side effects, and despite the fact that antibiotics produce only moderate results and only work for some people, doctors sometimes prescribe topical or oral antibiotics to treat acne.
If your doctor recommends antibiotics for your acne, ask about other treatments that come with fewer side effects and are more effective.
My Experience: When I had bad acne, my doctor put me on oral tetracycline, which did not improve my acne, but did upset my stomach. Later, a different dermatologist put me on clindamycin, a topical antibiotic, and while I did not suffer noticeable side effects, my skin was never worse in my life than when I was on clindamycin. I am only one person, but many people echo my experience. Antibiotics can come with side effects and often don’t help with acne.

The Science
- How Antibiotics Treat Acne
- Doctor Recommendations When Taking Antibiotics
- Topical Clindamycin Side Effects
- Topical Erythromycin Side Effects
- Oral Tetracycline Side Effects
- Oral Doxycycline Side Effects
- Oral Minocycline Side Effects
- Oral TMP-SMX Side Effects
- Oral Azithromycin Side Effects
- Oral Amoxicillin Side Effects
- Oral Erythromycin Side Effects
Despite not working at all for some people, and producing only moderate results when they do work, doctors frequently prescribe topical or oral antibiotics to treat acne. No antibiotic should be used for longer than 3 months, and therefore when they do produce results, the results are temporary. They also come with potentially serious side effects and should be used with caution.
How Antibiotics Treat Acne
The antibiotics used to treat acne fall into two broad categories.
- Topical antibiotics, which are applied to the skin, work locally, meaning that they affect the area of skin to which they are applied.
- Oral antibiotics, which are taken by mouth, are systemic medications, meaning that they affect the whole body.
Topical Antibiotics

Topical antibiotics work primarily by reducing inflammation rather than by killing bacteria.
Research indicates that while topical antibiotics can kill bacteria in the lab, they do not do so in human skin. When used to treat acne, they do reduce the numbers of acne bacteria by a minuscule amount, but not significantly.
According to a 2004 article in the journal Drugs, “Topical antibiotics have both anti-inflammatory and antibacterial mechanisms… Very little information is given in the literature concerning the [antimicrobial] effect of the topical antibiotics on C. acnes, and the published research suggests that both topical erythromycin and clindamycin have a moderate direct effect on C. acnes, not significantly reducing the number of surface and follicular bacteria… [This] means that topical antibiotics would act on inflammatory lesions by inhibiting inflammatory substances produced by C. acnes.”1
Oral Antibiotics

Oral antibiotics are usually prescribed for
- Severe acne
- Acne that affects the trunk (chest and/or back)
- Moderate acne that does not respond to topical treatments
Like topical antibiotics, they are also anti-inflammatory. However, unlike topical antibiotics, oral antibiotics do also kill bacteria to a significant degree. However, they do not completely clear acne: they only reduce the number of lesions.

A 2013 article in the Sao Paulo Medical Journal states, “[Oral antibiotics] act by reducing bacterial colonization and inflammation in the affected follicles. Despite their effectiveness in reducing the number of inflammatory lesions, no oral antibiotic completely clears acne.”2
Doctor Recommendations When Taking Antibiotics
When prescribing antibiotics, whether topical or oral, doctors recommend the following precautions:
- Only use antibiotics if other topical treatments, such as benzoyl peroxide or retinoids, do not work.1
- Always use antibiotics in combination with other medications, such as retinoids or benzoyl peroxide.1,2
- Never combine topical antibiotics with oral antibiotics.1,2
- Stop taking the medication if there is no improvement, or only slight improvement, within six to eight weeks.1
- Never use topical or oral antibiotics for more than 3 months.
Side Effects of Topical Antibiotics
The most commonly prescribed topical antibiotics for acne are:
- Clindamycin
- Erythromycin
Skin irritation is the most common side effect of both medications.

According to a 2015 article in the American Journal of Clinical Dermatology, “Local skin irritation that manifests as [redness], dryness, and burning at the application site is the most common adverse effect associated with topical antibiotic use. Similar to other topical agents, changing the formulation may help improve symptoms.”3
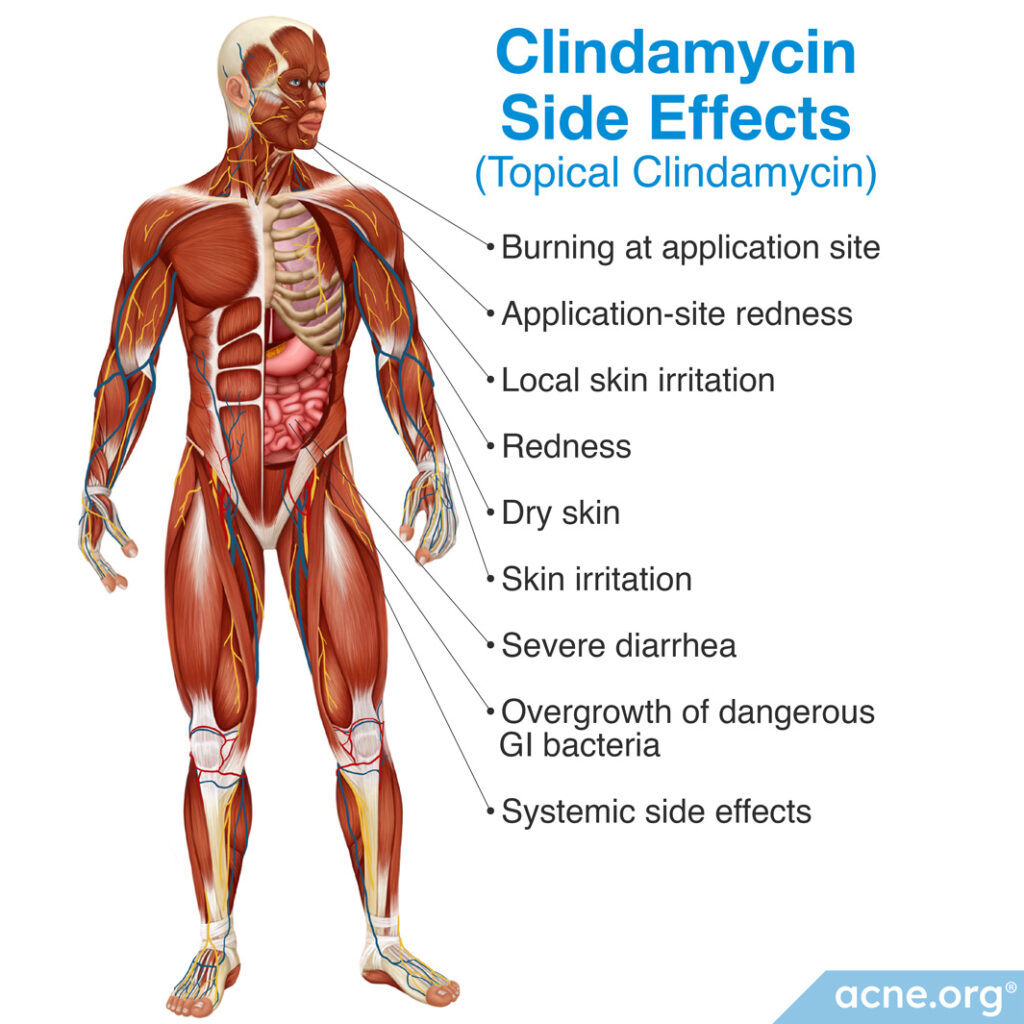
Topical Clindamycin Side Effects
Clindamycin’s most common side effect is skin irritation.4
When applied to large areas of skin, clindamycin can also be absorbed into the bloodstream and produce systemic side effects. Case reports indicate that absorption of clindamycin can cause gastrointestinal problems, such as severe diarrhea or overgrowth of dangerous bacteria that can disrupt the gastrointestinal system. Although research studies have not found a significant association between clindamycin use and such symptoms, doctors recommend the following precautions:
- Do not apply clindamycin to large areas of skin, such as the trunk.3
- Do not use clindamycin in patients who already suffer from gastrointestinal conditions.3,4
- If severe or prolonged diarrhea or other gastrointestinal symptoms develop while using clindamycin, discontinue the medication immediately.3
Topical Erythromycin Side Effects
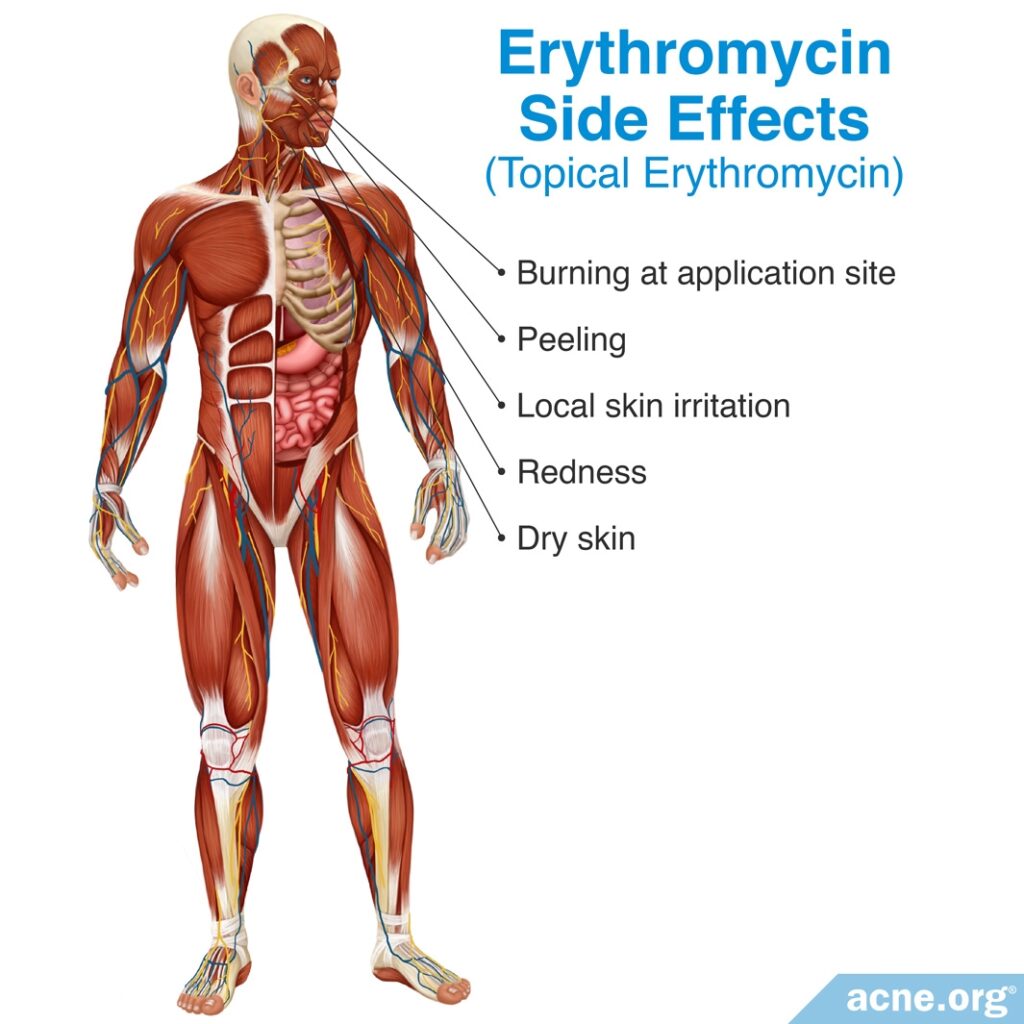
Erythromycin produces skin irritation in up to 20% of patients, but it is not absorbed into the body in the same manner as clindamycin, so it does not produce systemic side effects.

According to a 2013 article in Expert Opinion on Drug Safety, “Common adverse effects of erythromycin use are burning, peeling, dryness, [itching], and [redness]. In a study of 208 patients in a 12-week, multicenter, double-blind, controlled study comparing 2% erythromycin to [the same formulation without erythromycin]…92% experienced no peeling and 80% experienced no [redness] in the treatment group.“4
Side Effects of Oral Antibiotics
Oral antibiotics are taken by mouth and are absorbed into the bloodstream. With all oral antibiotics, the most common side effect is gastrointestinal distress, such as nausea, vomiting, or diarrhea.
All oral antibiotics can cause side effects that range from uncomfortable to dangerous.
The most commonly prescribed oral antibiotics are:
- Tetracycline
- Doxycycline
- Minocycline
Other antibiotics that can also be prescribed for acne include:
- Sarecycline
- TMP-SMX (trimethoprim-sulfamethoxazole)
- Azithromycin
- Amoxicillin
- Erythromycin
Oral Tetracycline Side Effects
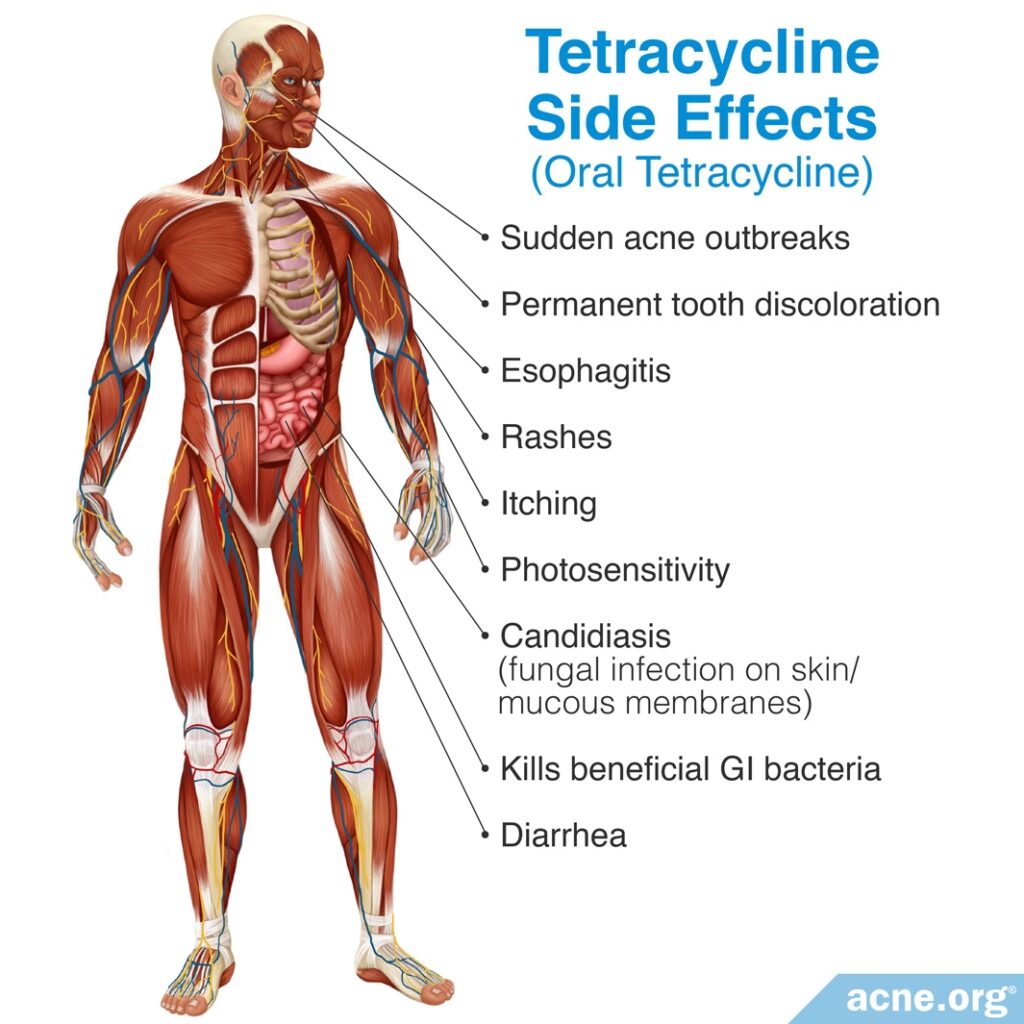
The most common side effect of tetracycline is gastrointestinal problems, which affect up to half of patients who take it. Tetracycline kills not only the harmful bacteria for which it is prescribed, but also beneficial bacteria that lives in the intestines and keeps them healthy. With prolonged use, these intestinal imbalances can be passed to close contacts, such as family members.

According to a 2015 article in the American Journal of Clinical Dermatology, “The most common reported side effect of oral tetracyclines is gastrointestinal upset. Studies have shown that long-term therapy favors multi-drug-resistant organisms in the intestines and can also affect the gastrointestinal flora of close contacts.”3

A 2013 article in Expert Opinion on Drug Safety also notes, “The most commonly reported side effect of oral tetracycline is gastrointestinal distress, such as nausea and esophagitis, with the reported rate of any type of gastrointestinal event in all the trials ranging from 0.54 to 51.7%.”4
The second most common side effect of tetracycline is skin reactions – which occur in up to 30% of patients taking it – including rashes, itching, and increased sensitivity to the sun (photosensitivity).4 It can also cause permanent tooth discoloration, candidiasis (a fungal infection of the skin or mucus membranes), and even sudden outbreaks of acne.

A 2015 article in the American Journal of Clinical Dermatology states that “tetracycline is the most likely antibiotic in its class to cause candidiasis and tooth discoloration.”3
Oral Doxycycline Side Effects
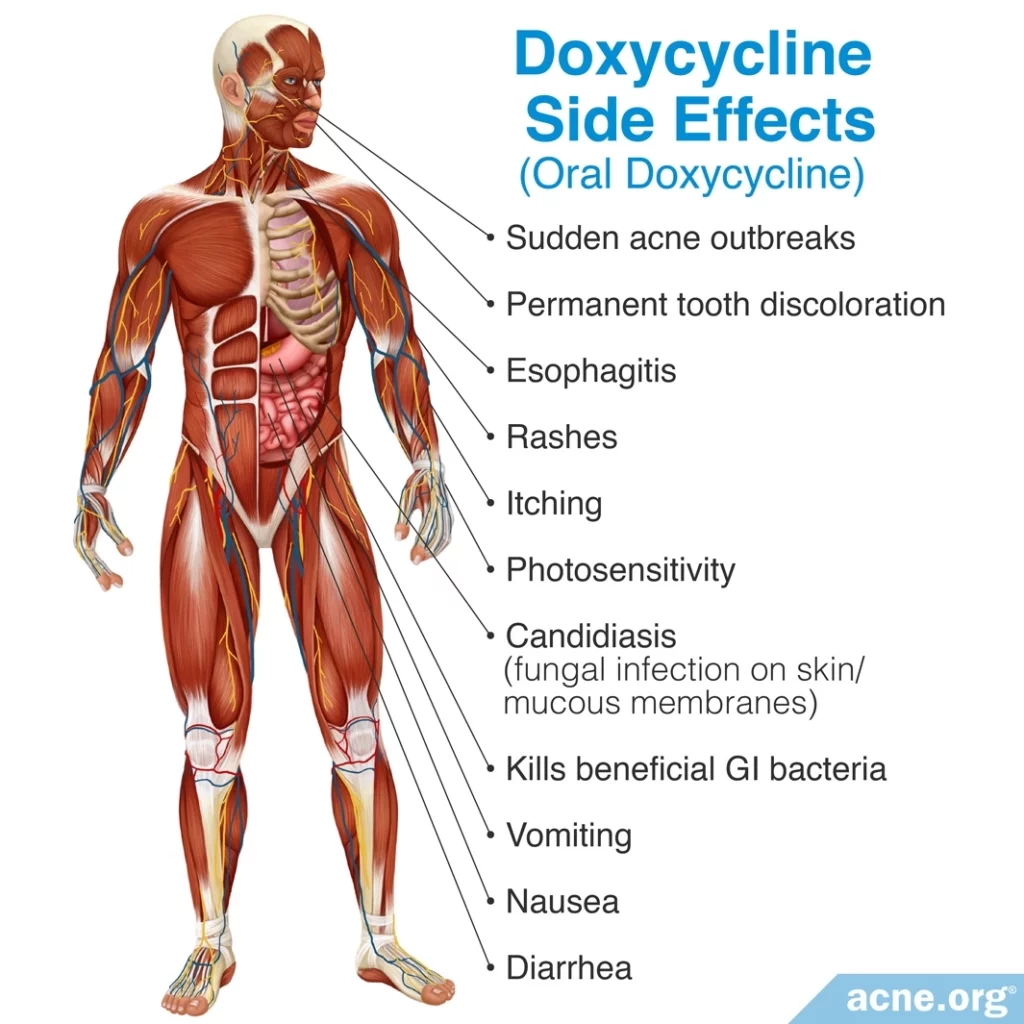
Doxycycline is in the tetracycline family of antibiotics, and therefore causes all of the same side effects to tetracycline, but is more likely than tetracycline to cause increased sensitivity to the sun.
The most common side effect is gastrointestinal upset, which affects 20 – 30% of patients taking it. The next most common side effect is photosensitivity, affecting up to 6% of patients on it.

A 2015 article in the American Journal of Clinical Dermatology notes, “The most common adverse effect of doxycycline is gastrointestinal distress. Unlike tetracycline, this agent should be taken with food to help minimize gastric irritation… Doxycycline is the most phototoxic of the tetracyclines, causing [redness] and [swelling from excess fluid accumulation] in sun-exposed areas…Patients need to be advised to avoid direct sun exposure and to wear appropriate sunscreen.“3

A 2023 study published in the Journal of Infection in Developing Countries found that gastrointestinal discomfort was more common in patients older than 50 and in those who took 200 mg of doxycycline a day rather than 100 mg.5
Doxycycline can also cause permanent tooth discoloration in children and can cause candidiasis.

According to a 2013 article in Expert Opinion on Drug Safety, “Tetracyclines can also lead to permanent discoloration of teeth in children whose teeth are developing, as the drug incorporates into tissues that are calcifying at the time of their administration leading to yellow or gray to brown discoloration of both the primary and permanent [teeth]. In addition, vaginal candidiasis can manifest with use of tetracycline, and typically Candida albicans [the fungus that causes candidiasis] is present at the involved site.“4
Oral Minocycline Side Effects
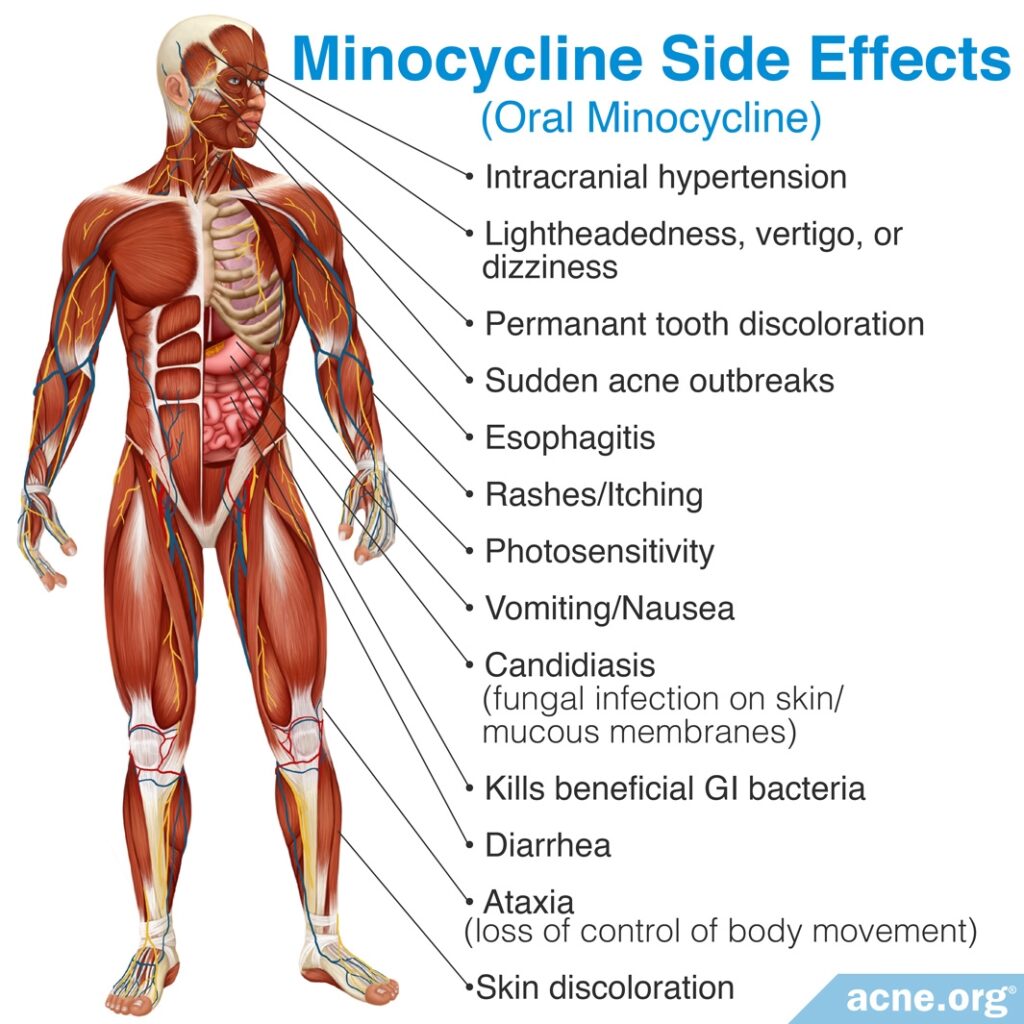
Minocycline is also in the tetracycline family of antibiotics, and causes the same side effects as other tetracyclines, but also comes with other side effects, and causes the most serious side effects of all the tetracyclines.
In addition to the usual gastrointestinal symptoms, it causes central nervous system side effects, such as lightheadedness and vertigo, in up to 67% of patients who take it.

According to a 2015 article in the American Journal of Clinical Dermatology, “Minocycline is more likely to cause central nervous system disturbances than are other tetracyclines. Vertigo (significantly higher prevalence in women), dizziness, ataxia [lack of muscle control], and lightheadedness occur…and tend to resolve with cessation of treatment. Starting treatment at a lower dose or using the extended-release formula can help prevent these effects.”3 Like tetracycline and doxycycline, minocycline can also cause permanent tooth discoloration, but can also cause skin discoloration.

According to the same 2015 article in the American Journal of Clinical Dermatology, “Minocycline therapy has been associated with either a blue/black or ruddy brown discoloration of the skin that most commonly occurs in acne scars, over the shins, or in sun-exposed areas. As with doxycycline, pigmentation of teeth is also possible, especially if given to children aged less than 8 years.”3
In rare cases, prolonged use can cause autoimmune diseases.

The same article notes, “The development of autoimmune diseases has been reported with the use of minocycline and represents a rare but serious adverse effect. These diseases include drug-induced lupus, autoimmune hepatitis, serum sickness-like reaction, and hypersensitivity syndrome.”3
In addition, minocycline can cause another rare but serious side effect called intracranial hypertension, which is an increase in the pressure inside the skull. Because this side effect occurs more frequently in people who are also taking oral retinoids, such as isotretinoin, doctors recommend that minocycline not be combined with them.3
Because minocycline, like other antibiotics, kills beneficial bacteria alongside harmful bacteria, it can disrupt the balance of bacteria in the body. The skin and gut are home to many species of beneficial bacteria that perform important functions, including keeping harmful bacteria in check. When minocycline kills these beneficial bacteria, that allows some other harmful species of bacteria that are unaffected by minocycline to run wild. For example, one study found that taking minocycline for a month caused a dramatic increase in the number of Pseudomonas and Streptococcus bacteria in acne patients.6 Pseudomonas can cause a skin infection called gram-negative folliculitis, while Streptococcus is responsible for respiratory infections like strep throat.7

The authors of the study, published in JAMA Dermatology in 2019, wrote, “The transient growth of bacterial populations, such as Pseudomonas species, immediately following antibiotic treatment points toward the possibility of opportunistic skin infections, such as gram-negative folliculitis, with prolonged antibiotic therapy for acne.”6
Oral Sarecycline Side Effects
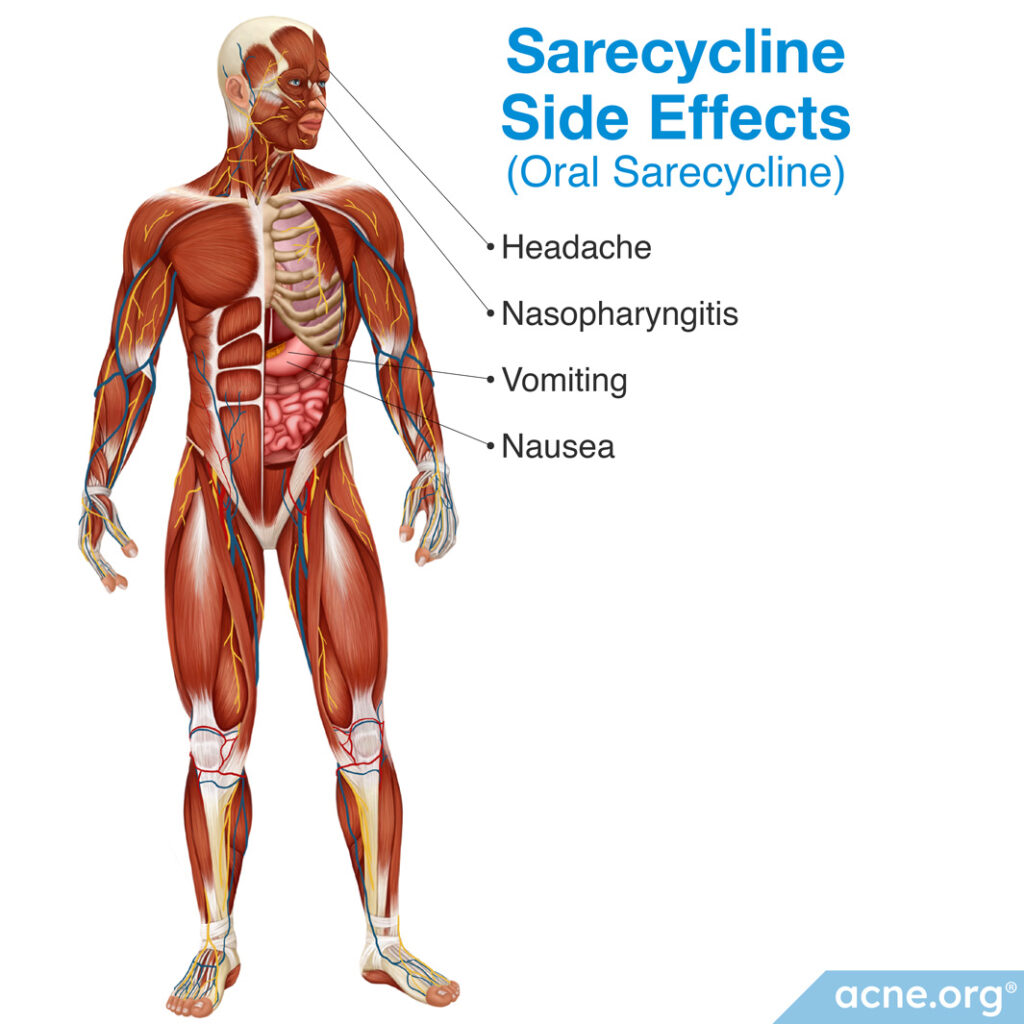
Sarecycline is a relatively new oral antibiotic approved for acne in 2018. It belongs to the tetracyclines group of antibiotics together with doxycycline and minocycline, but the data available so far suggest that sarecycline causes fewer side effects than the other antibiotics in this group. However, sarecycline can still cause gastrointestinal issues like nausea and vomiting as well as nasopharyngitis (runny nose, sneezing, and coughing).8,9

According to a 2018 study published in Journal of Drugs in Dermatology, the most common side effects of sarecycline ware nausea, nasopharyngitis (runny nose, sneezing, and coughing), and vomiting. However, the authors noted that most of these side effects seen in the study may have been coincidental and not due to the sarecycline.9

Another study published in The Journal of Clinical and Aesthetic Dermatology in 2019 found that sarecycline causes less side effects than other tetracyclines. The researchers wrote, “Patients…with moderate-to-severe acne vulgaris who received sarecycline once daily for up to 40 weeks showed low rates of adverse effects, with nasopharyngitis, upper respiratory tract infection, headache, and nausea being the only adverse effects reported by 2% or more of patients.”10
Oral TMP-SMX Side Effects
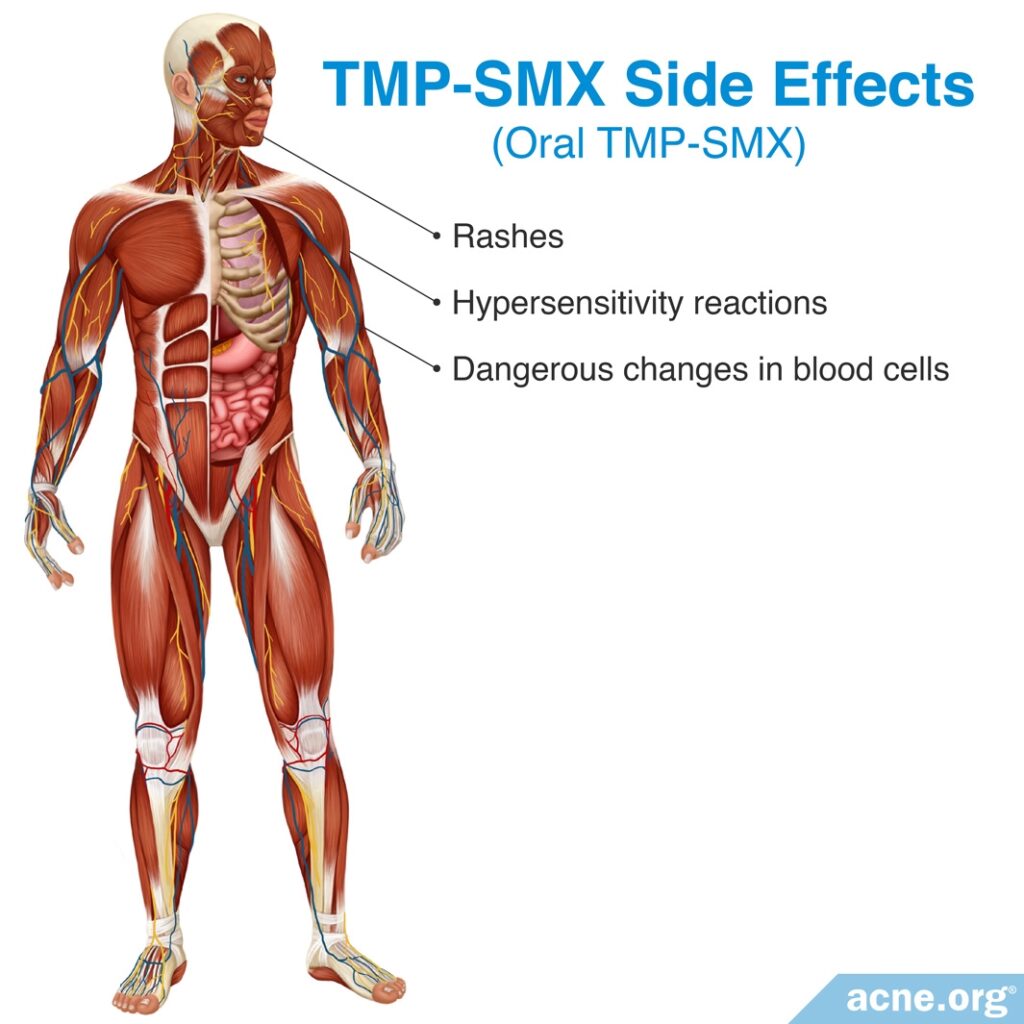
TMP-SMX (trimethoprim-sulfamethoxazole) is occasionally prescribed for acne. It can cause severe side effects such as rashes, hypersensitivity reactions, and dangerous changes in blood cells. Because of the severity of these side effects, doctors use caution when prescribing TMP-SMX and typically reserve its use for patients who cannot tolerate other medications.3
Oral Azithromycin Side Effects
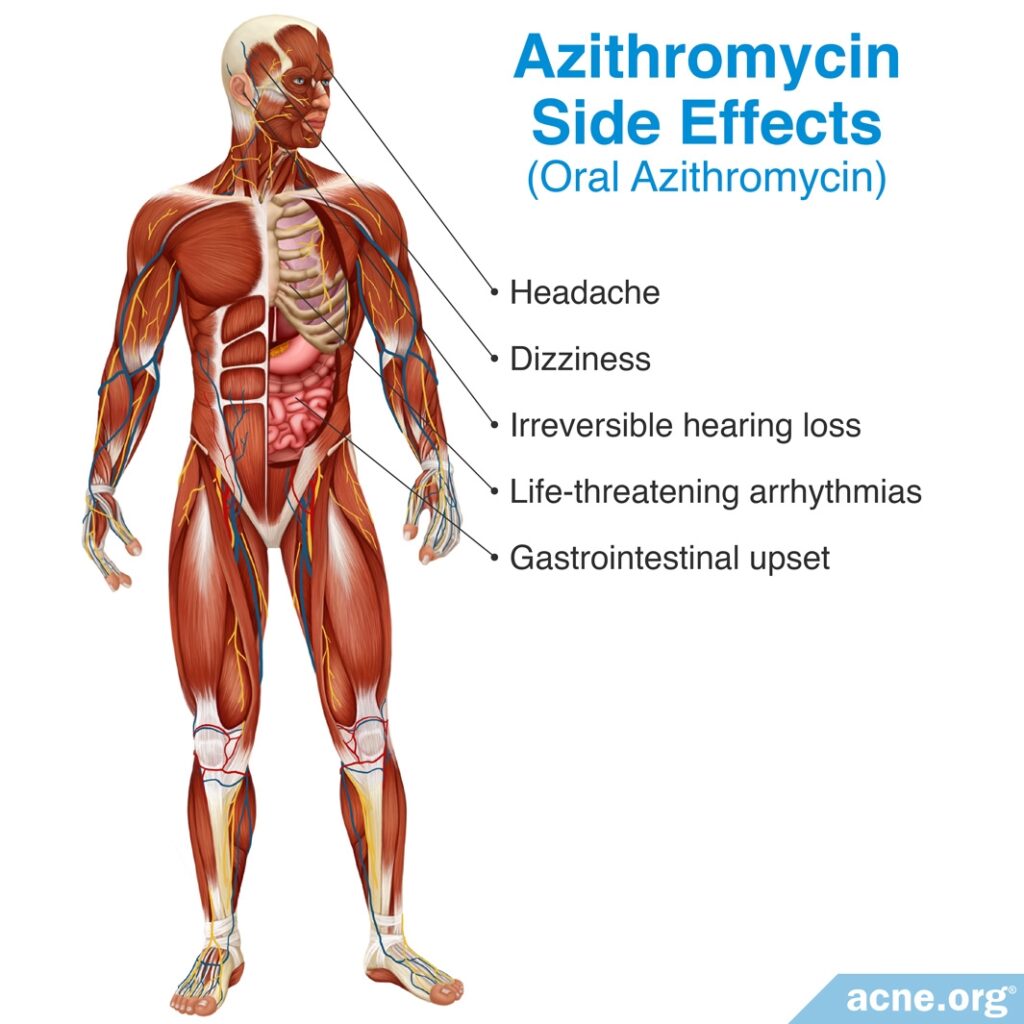
Like all other oral antibiotics used for acne, azithromycin frequently causes gastrointestinal upset, though typically to a lesser degree than other antibiotics. Other common side effects include headache and dizziness. So why doesn’t everyone use azithromycin? Because while the most common side effects of azithromycin are relatively mild, recent studies indicate that azithromycin can also cause serious side effects, such as life-threatening arrhythmias (irregular heart rhythm) and irreversible hearing loss.3,11

According to a 2015 article in the American Journal of Clinical Dermatology, “Azithromycin is generally well-tolerated, causing only mild and transient gastrointestinal disturbances that can be alleviated with the use of antacids prior to treatment.”3

A 2015 article in Australian Prescriber also notes, “Azithromycin is generally well tolerated, but relatively common adverse effects (1 – 5% of patients) include gastrointestinal upset, headache and dizziness.”11
Oral Amoxicillin Side Effects
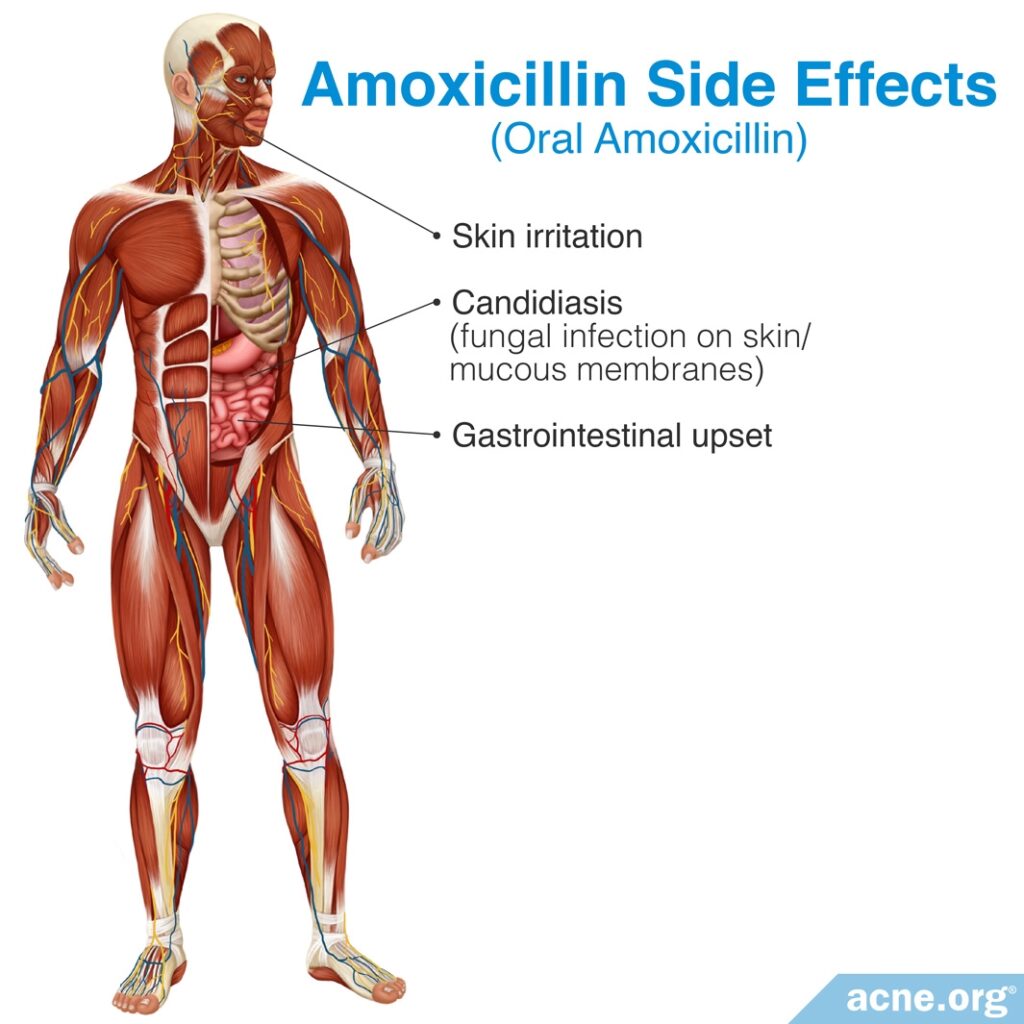
Amoxicillin is occasionally prescribed for acne, though there is little evidence indicating whether it is effective for this condition.
According to a 2007 article in Advances in Dermatology, “Amoxicillin has been used anecdotally in the treatment of refractory acne vulgaris, but there are no studies of efficacy for amoxicillin for this indication.”12
Amoxicillin is generally well tolerated, with relatively mild side effects. The most common side effects are similar to those of other oral antibiotics: gastrointestinal upset, skin irritation, and candidiasis.3,13
Oral Erythromycin Side Effects
Doctors sometimes prescribe oral erythromycin as an alternative antibiotic to patients who are allergic to tetracyclines or amoxicillin or to those who are pregnant, as it is one of the few antibiotics that can be prescribed during pregnancy.4 Like other oral antibiotics, erythromycin causes gastrointestinal side effects, such as nausea, abdominal cramping, and vomiting. However, it also frequently interacts with other medications, and these interactions can cause serious side effects, such as arrhythmias (irregular heartbeat) and sudden death.4,14
The Bottom Line
Neither topical nor oral antibiotics will completely clear acne. When they work at all, they should only be used for 3 months, which means results will be temporary at best. Topical antibiotics often produce skin irritation, and oral antibiotics are well known to produce gastrointestinal upset and nervous system problems, and sometimes more serious lifelong side effects like permanent tooth discoloration, hearing loss, or death.
Acne therapy has come a long way since the time when doctors only had antibiotics to prescribe to patients. If your doctor prescribes antibiotics for your acne, be sure to ask why this is the treatment of choice, and get a second opinion.
References
- Dreno, B. Topical antibacterial therapy for acne vulgaris. Drugs. 64, 2389-2397 (2004). https://www.ncbi.nlm.nih.gov/pubmed/15481998
- Costa, C. S. & Bagatin, E. Evidence on acne therapy. Sao Paulo Med. J. 18, 193-197 (2013). http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1516-31802013000300193
- Oudenhoven, M. D., Kinney, M. A., McShane, D. B., Burkhart, C. N. & Morrell, D. S. Adverse effects of acne medications: recognition and management. Am. J. Clin. Dermatol. 16, 231-242 (2015). https://www.ncbi.nlm.nih.gov/pubmed/25896771
- Tripathi, S. V., Gustafson, C. J., Huang, K. E. & Feldman, S. R. Side effects of common acne treatments. Expert Opin. Drug Saf. 12, 39-51 (2013). https://www.ncbi.nlm.nih.gov/pubmed/23163336
- Eljaaly, K., Alghamdi, H., Almehmadi, H., Aljawi, F., Hassan, A. & Thabit, A. K. Long-term gastrointestinal adverse effects of doxycycline. J. Infect. Dev. Ctries. 17, 281-285 (2023). https://pubmed.ncbi.nlm.nih.gov/36897904/
- Chien, A. L., Tsai, J., Leung, S. et al. Association of systemic antibiotic treatment of acne with skin microbiota characteristics. JAMA Dermatol. 155, 425 – 434 (2019). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6459106/
- Levy, R. M., Huang, E. Y., Roling, D., Leyden, J. J. & Margolis, D. J. Effect of antibiotics on the oropharyngeal flora in patients with acne. Arch. Dermatol. 139, 467 – 471 (2003). https://www.ncbi.nlm.nih.gov/pubmed/12707094
- Moore, A. Y., Del Rosso, J., Johnson, J. L. & Grada, A. Sarecycline: A review of preclinical and clinical evidence. Clin. Cosmet. Investig. Dermatol. 13, 553-560 (2020). https://pubmed.ncbi.nlm.nih.gov/32884318/
- Moore, A., Green, L. J., Bruce, S., Sadick, N., Tschen, E., Werschler, P., Cook-Bolden, F. E., Dhawan, S. S., Forsha, D., Gold, M. H., Guenthner, S., Kempers, S. E., Kircik, L. H., Parish, J. L., Rendon, M. I., Rich, P., Stein-Gold, L., Tyring, S. K., Weiss, R. A., Nasir, A., Schmitz, C., Boodhoo, T. I., Kaoukhov, A. & Berk, D. R.. Once-daily oral sarecycline 1.5 mg/kg/day is effective for moderate to severe acne vulgaris: Results from two identically designed, Phase 3, randomized, double-blind clinical trials. J. Drugs Dermatol. 17, 987-996 (2018). https://pubmed.ncbi.nlm.nih.gov/30235387/
- Pariser, D. M., Green, L. J., Lain, E. L., Schmitz, C., Chinigo, A. S., McNamee, B. & Berk, D. R. Safety and tolerability of sarecycline for the treatment of acne vulgaris: Results from a Phase III, multicenter, open-label study and a Phase I phototoxicity study. J. Clin. Aesthet. Dermatol. 12, E53-E62 (2019). https://pubmed.ncbi.nlm.nih.gov/32038757/
- McMullan, B. J. & Mostaghim, M. Prescribing azithromycin. Aust. Prescr. 38, 87-90 (2015). https://www.ncbi.nlm.nih.gov/pubmed/26648627
- Turowski, C. B. & James, W. D. The efficacy and safety of amoxicillin, trimethoprim-sulfamethoxazole, and spironolactone for treatment-resistant acne vulgaris. Adv. Dermatol. 23, 155-163 (2007). https://www.ncbi.nlm.nih.gov/pubmed/18159900
- Gillies, M. et al. Common harms from amoxicillin: a systematic review and meta-analysis of randomized placebo-controlled trials for any indication. CMAJ. 187, E22-E31 (2015). https://www.ncbi.nlm.nih.gov/pubmed/25404399
- Schoenholtz, J. C. Oral erythromycin and the risk of sudden death. N. Engl. J. Med. 352, 301-304 (2005). https://www.ncbi.nlm.nih.gov/pubmed/15356306
 Acne.org Products
Acne.org Products