Yes, They Usually Clear the Skin to a Significant Degree, but Carry Risk

The Essential Info
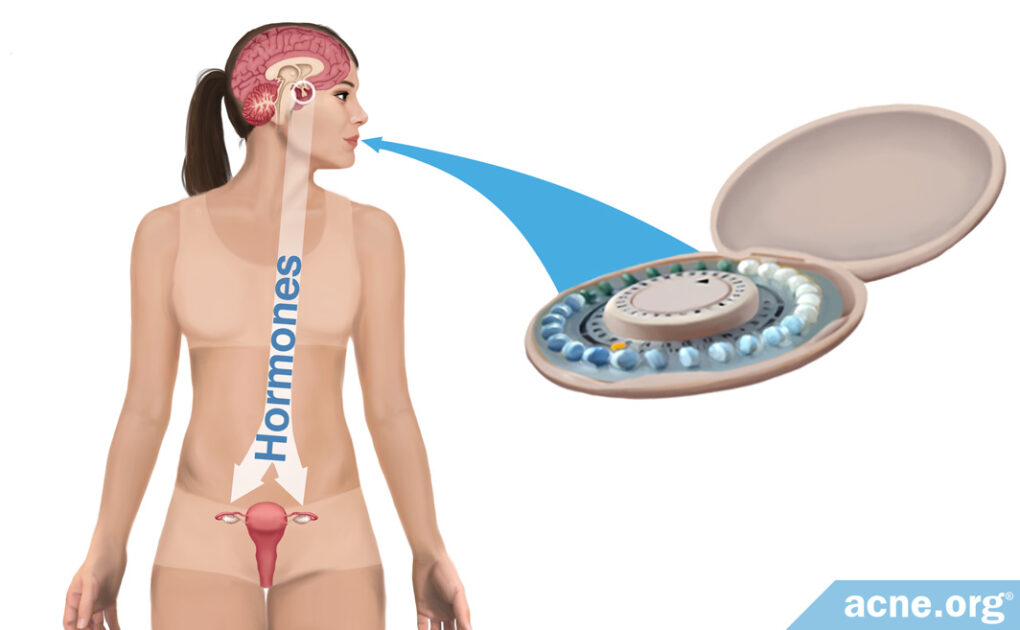
Acne is linked to hormones that fluctuate throughout the menstrual cycle, and for this reason, doctors sometimes prescribe birth control pills to stabilize hormones and reduce acne.
The most common type of birth control pill, called combined oral contraceptives (COCs), can help clear acne, normally by about 35% after 3 months and 55-60% after 6 months.
Studies show us that there are no stand-outs when it comes to which brand or type of COC is better for acne, and that they all work similarly and clear acne about equally well.
Oral contraceptives have become safer over the years but still carry risks, so it is important to consult a doctor before deciding to take them, and make sure you do not smoke while using them. As with any health decision, especially one that involves something as fundamental as your hormones, make sure to be your own advocate as you discuss the option of taking oral contraceptives with your doctor.
Rebound Acne: There are no studies looking at whether acne might rebound after you stop taking COCs. However, it makes sense that as your hormones return to their natural levels, you might see a return of acne symptoms, so this is something to keep in mind.

The Science
Many women report an increase in acne approximately 7 – 10 days before menstruation and then a decrease in acne once menstruation begins. These cyclical acne symptoms are a result of the fluctuation of several different hormones during the menstrual cycle, each of which plays a different role in acne:
- Androgens (increase acne): Androgens are male hormones that are present in both males and females. Androgens increase skin oil production, and more skin oil leads to more acne.
- Estrogens (reduce acne): Estrogens reduce the production of androgens. Lower amounts of androgens means lower skin oil production, which results in less acne.
- Progesterone (unknown effect on acne): Progesterone is a female hormone that is present in both males and females. Whether progesterone affects acne remains unknown.1-4
What Are Oral Contraceptives (Birth Control Pills), and How Do They Treat Acne?
Birth control pills, also called oral contraceptives, are a hormonal therapy. There are two types of birth control pill:
- Pills that contain a combination of progestin (a synthetic form of progesterone) + ethinyl estradiol (a synthetic form of estrogen): These pills, called combined oral contraceptives (COCs), contain both progestin and ethinyl estradiol, and are an acne treatment.
- Pills that contain only progestin. These pills contain only progestin, and are not an acne treatment.4,5
Birth control pills not only prevent pregnancy but also regulate the menstrual cycle by stabilizing hormone levels throughout the month.
The estrogen in COCs prevents ovulation but also reduces the level of androgens in the body. This is important because lower levels of androgens normally result in a lower production of skin oil, and in general, less skin oil means less acne.
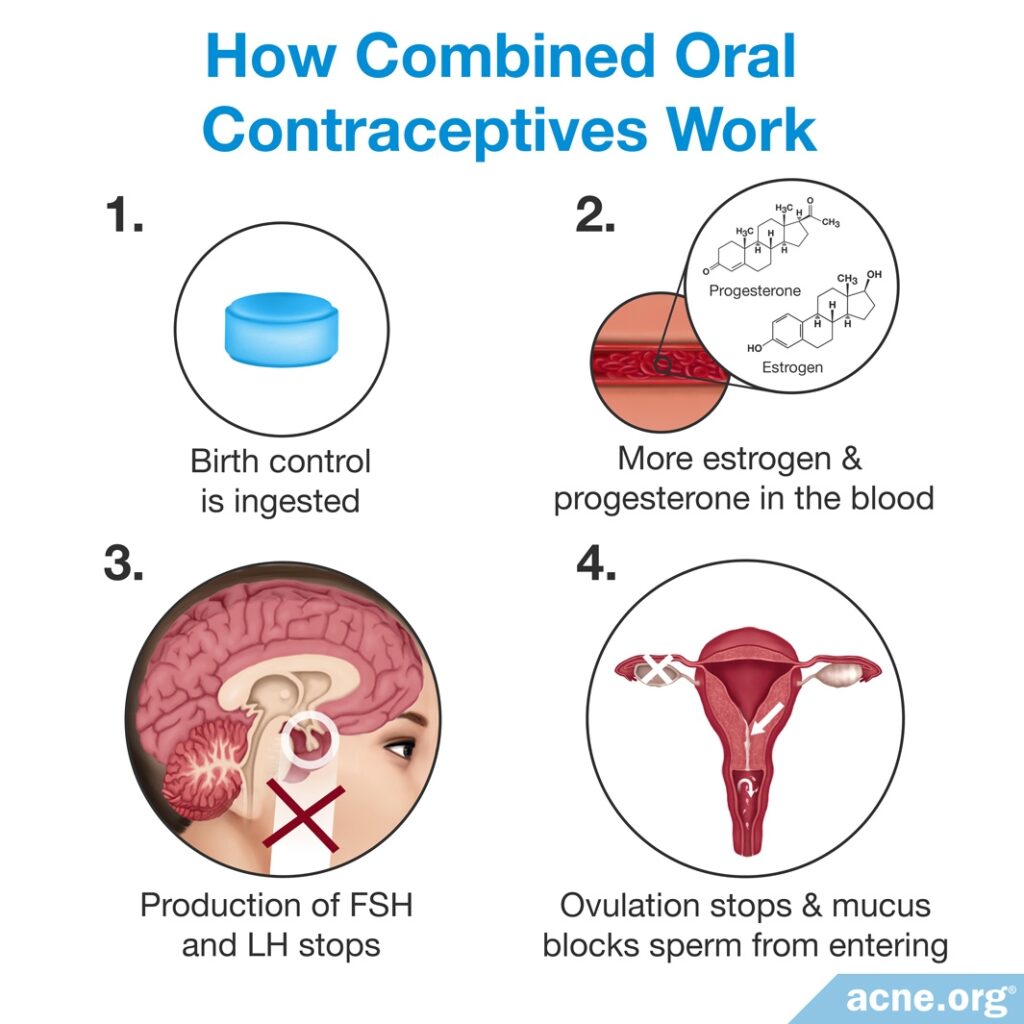
The role of progestin in acne treatment is unclear. Some studies indicate that progestin may reduce androgen and skin oil levels, which would theoretically help reduce acne.4 However, other studies show that it may worsen acne. In a 2018 article in the Dermatology Online Journal, researchers reviewed the evidence and concluded that we still do not fully understand how progestin levels impact acne, so more studies investigating this are needed.6
There are many COCs on the market. In the United States, the FDA (Food and Drug Administration) approved three COCs containing the progestins norgestimate, norethindrone, and drospirenone, for acne treatment.4 While only these three officially are approved in the U.S. for acne, this does not mean they are superior to other COCs in combatting acne. In fact, most studies comparing different COCs find that they are all about equally effective at treating acne.
Regardless of which COC might clear acne slightly better or worse than another, there is high quality research that shows that all COCs can treat acne:
- A systematic review that looked at the results of research on a total of over 12,000 participants concluded that COCs can reduce both inflammatory and non-inflammatory acne.7
- According to a meta-analysis that reviewed 13 high-quality research studies, COCs reduce acne lesions by 55 – 60% after 6 months of use.8
- In addition, 3 newer studies compared the efficacy of 2 different oral contraceptive pills at treating acne. These two studies found that both oral contraceptive pills reduced acne symptoms, but disagreed on whether one pill might be better than the other.9-11
Expand to read details of research

A 2012 systematic review published in the Cochrane Database of Systematic Reviews looked at 31 clinical trials with a total of 12,579 participants in order to determine whether COCs were effective or not in treating acne. The researchers found that COCs reduced the number of acne lesions, the severity of acne, and the degree of self-assessed acne. The authors concluded, “The six COCs evaluated in placebo-controlled trials are effective in reducing inflammatory and non-inflammatory facial acne lesions.”7
This systematic review also found that COCs containing the progestins, chlormadinone acetate or cyproterone acetate, seemed to reduce acne better than those containing levonorgestrel. Also, COCs containing drospirenone may be more effective than those containing norgestimate or nomegestrol acetate. However, the evidence for these findings is limited. Overall, all COCs improved acne, but there is not enough evidence to say which one works best.7

A 2014 meta-analysis published in the Journal of the American Academy of Dermatology reviewed 13 randomized clinical trials that compared the efficacy of COCs to placebo. The authors concluded that COCs were effective in treating acne, with approximately 35% reduction in acne lesions after three months and 55 – 60% reduction after 6 months.8
Newer studies comparing 2 different oral contraceptive pills

A 2019 study published in the Journal of Endocrinological Investigation tested 2 different COCs on women with acne caused by a hormonal imbalance. A total of 120 women participated in the study. The researchers divided the women into 2 groups of 60:
- Group 1 took a COC containing ethinyl estradiol and drospirenone
- Group 2 took a COC containing ethinyl estradiol and chlormadinone acetate
After 6 months of taking the pills, the women in both groups experienced a significant reduction in acne lesions. Both COCs were equally effective at treating acne. The researchers wrote, “No statistically significant difference was observed in the effect…between the two treatments.”9
A 2018 study published in the journal Contraception and Reproductive Medicine also compared the same 2 COCs. A total of 180 women with mild-to-moderate acne participated in the study. The researchers divided the women into 2 groups of 90:
- Group 1 took a COC containing ethinyl estradiol and chlormadinone acetate
- Group 2 took a COC containing ethinyl estradiol and drospirenone
After 6 months of taking the pills, the women in both groups experienced an improvement in their acne. However, more women in Group 1 rated their improvement as “excellent” than in Group 2. Specifically, 66% of the women taking the pill with chlormadinone acetate felt that their acne improvement was excellent, compared to 48% of the women taking the pill with drospirenone.10
To sum up, while these 2 studies disagree on whether COCs containing chlormadinone acetate might be better than COCs containing drospirenone, they agree in finding that both types of COCs significantly reduce acne symptoms.

A 2020 study published in the journal Dermatologic Therapy compared the efficacy of 2 other oral contraceptive pills for treating acne. A total of 80 women, only 20 of whom had acne, participated in the study. The researchers divided them into 2 equal groups:
- Group 1 took a COC containing levonorgestrel and ethinyl estradiol
- Group 2 took an oral contraceptive pill containing only levonorgestrel
After 6 months of treatment, acne decreased by 45.67% in Group 1 and by 29.72% in Group 2. The researchers concluded that a COC containing both levonorgestrel and ethinyl estradiol was more effective for treating acne than levonorgestrel alone.11 We should note that only 10 women in each group in this experiment had acne, which is too few to draw any strong conclusions.
Safety Concerns
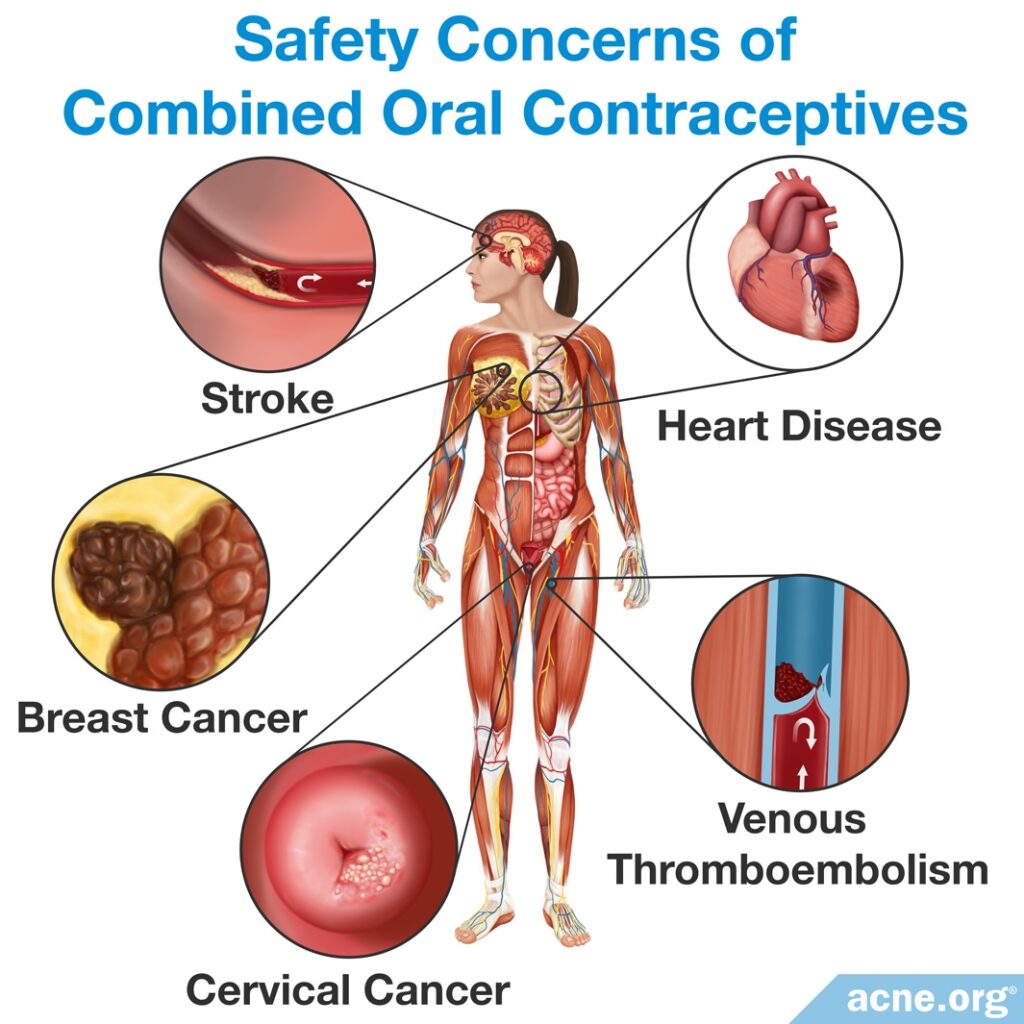
Overall, researchers have determined that COCs are relatively safe and generally only cause temporary side effects such as flu-like symptoms or nausea, if any.12 A study done on 23,000 people taking COCs found that the risk of death was the same in women who had used COCs as it was in women who had not.4
However, it is important to consult a doctor before starting combined oral contraceptive treatment. This is because oral contraceptives pose risks.
Heart Disease
Older COCs that contained high doses of ethinyl estradiol resulted in more side effects when compared to newer ones, which contain lower doses. High-dose COCs were associated with higher incidence of heart disease, and the introduction of low-dose COCs has reduced this risk. Healthy women who do not smoke and who use a COC with less than 50 micrograms of estrogen are not at increased risk of heart disease. However, women who do not fall into the “healthy, non-smoking” category are more susceptible to heart disease when taking a COC. Risk factors for heart disease when taking COCs include age over 35, smoking 15 or more cigarettes a day, high blood pressure, cholesterol problems, diabetes, and obesity.4
Venous thromboembolism (VTE)
Venous thromboembolism is a blood clot in the veins that can be life-threatening. This risk when taking COCs is dependent on the dose of estrogen, with higher amounts of estrogen increasing the risk. Also, notably, some studies reported that newer progestins such as drospirenone increase the risk of VTE. To minimize this risk, experts advise that women take newer COCs that contain norgestrel, levonorgestrel, or norgestimate. Other risk factors for VTE include age, obesity, smoking, immobilization (for example, being in a cast), and certain blood-clotting diseases. People with blood-clotting diseases should not take COCs.4,11,13
Stroke
Stroke is listed as a risk when taking COCs. The degree of risk is unclear, but it is low in young, healthy women taking COCs.4
Breast and Cervical Cancers
There is some evidence that COCs can increase the risk of breast and cervical cancers. However, the evidence for this is controversial and limited. Any increased risk for either of these cancers is reduced upon stopping the pills and is eliminated 10 years after stopping the pills.4
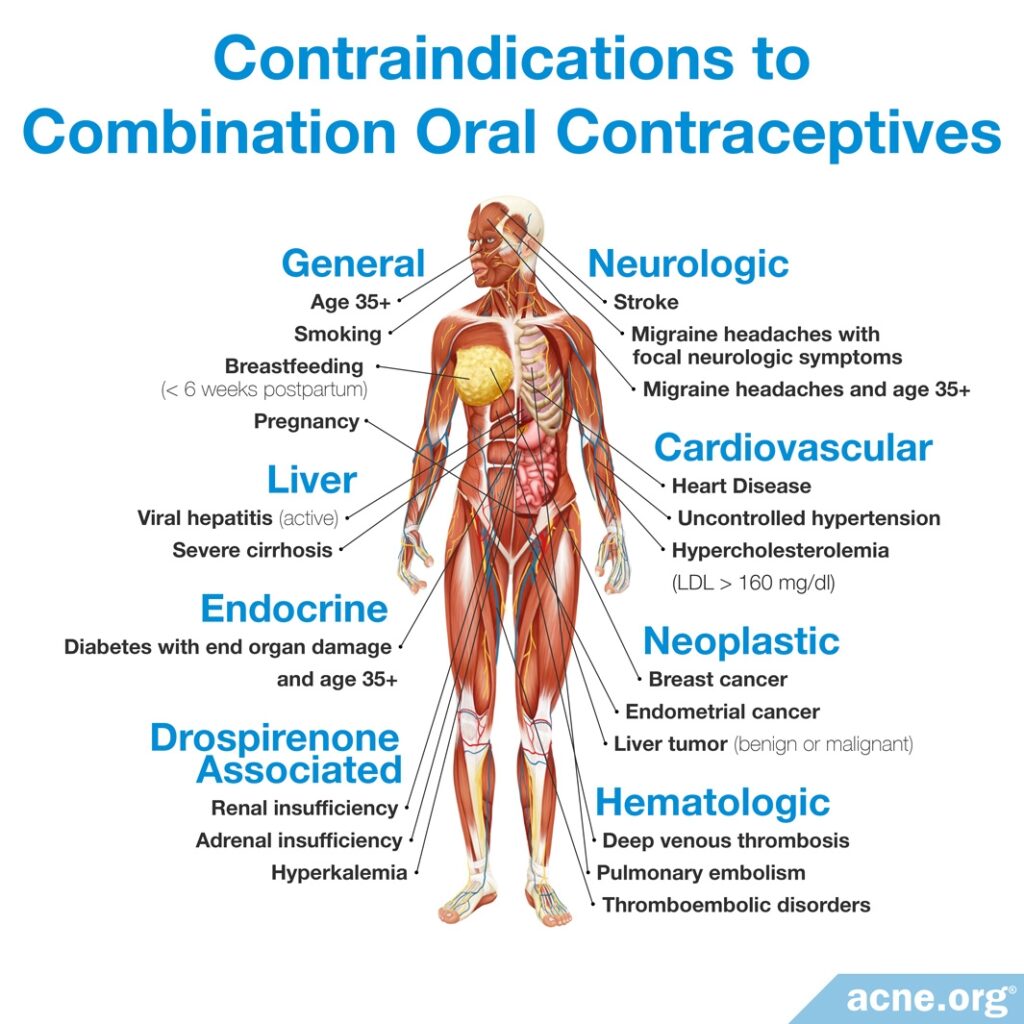
The following graphic gives an overview of conditions under which women should not take COCs.
References
- Raghunath, R. S., Venables, Z. C. & Millington, G. W. The menstrual cycle and the skin. Clin. Exp. Dermatol. 40, 111 – 115 (2015). https://www.ncbi.nlm.nih.gov/pubmed/25683236
- Farage, M. A., Neill, S. & MacLean, A. B. Physiological changes associated with the menstrual cycle: a review. Obstet. Gynecol. Surv. 64, 58 – 72 (2009). https://www.ncbi.nlm.nih.gov/pubmed/19099613
- Arora, M. K., Yadav, A. & Saini, V. Role of hormones in acne vulgaris. Clin. Biochem. 44, 1035 – 1040 (2011). https://www.ncbi.nlm.nih.gov/pubmed/21763298
- Lam, C. & Zaenglein, A. L. Contraceptive use in acne. Clin. Dermatol. 32, 502 – 515 (2014). https://www.ncbi.nlm.nih.gov/pubmed/25017461
- Harper, J. C. Use of oral contraceptives for management of acne vulgaris. Dermatol. Clin. 34, 159 – 165 (2016). https://www.ncbi.nlm.nih.gov/pubmed/27015775
- Bosanac, S. S., Trivedi, M., Clark, A. K., Sivamani, R. K. &, Larsen, L. N. Progestins and acne vulgaris: a review. Dermatol. Online J. 24, 5 (2018). https://www.ncbi.nlm.nih.gov/pubmed/30142728
- Arowojolu, A. O., Gallo, M. F., Lopez, L. M. & Grimes, D. A. Combined oral contraceptive pills for treatment for acne. Cochrane Database Syst. Rev. 7, CD04425 (2012). https://www.ncbi.nlm.nih.gov/pubmed/22786490
- Koo, E. B., Petersen, T. D. & Kimball, A. B. Meta-analysis comparing efficacy of antibiotics versus oral contraceptives in acne vulgaris. J. Am. Acad. Dermatol. 71, 450 – 459 (2014). https://www.ncbi.nlm.nih.gov/pubmed/24880665
- Podfigurna, A., Meczekalski, B., Petraglia, F. & Luisi, S. Clinical, hormonal and metabolic parameters in women with PCOS with different combined oral contraceptives (containing chlormadinone acetate versus drospirenone). J. Endocrinol. Invest. 43, 483-492 (2019). doi: 10.1007/s40618-019-01133-3. https://www.ncbi.nlm.nih.gov/pubmed/31654312
- Jaisamrarn, U & Santibenchakul, S. A comparison of combined oral contraceptives containing chlormadinone acetate versus drospirenone for the treatment of acne and dysmenorrhea: a randomized trial. Contracept. Reprod. Med. 3, 5 (2018). https://www.ncbi.nlm.nih.gov/pubmed/29662684
- Moubasher, A. E. A., Abdel Basset, H. A., Khalil, A. A. M. & Youssef, E. M. K. Levonorgestrel vs combined oral contraceptive pills in treatment of female acne and hirsutism. Dermatol. Ther. 33, e13700 (2020). https://pubmed.ncbi.nlm.nih.gov/32713062/.
- Sun, X., Qian, F., He, Y., Gu, X. & Di, W. Safety and efficacy of combined oral contraceptive ethinyl estradiol/drospirenone (YAZ) in Chinese women: A single-arm, open-label, multicenter, post-authorization study. Adv. Ther. 37, 906-917 (2020). https://pubmed.ncbi.nlm.nih.gov/31950432/
- Grandi, G., Guariglia, G. & Facchinetti, F. The role of combined oral contraceptives containing norgestimate for acne vulgaris treatment: a review. Eur. J. Contracept. Reprod. Health Care 28, 184-191 (2023). https://pubmed.ncbi.nlm.nih.gov/37042197/
 Acne.org Products
Acne.org Products