Acne Conglobata Is a Rare and Unusually Severe Form of Acne

The Essential Info
What It Is: Acne conglobata is a severe form of acne that comes with a range of lesions, most notably nodules, cysts, blackheads, abscesses, and draining sinuses. It often leaves large, disfiguring scars. The disease typically affects young males, but females may develop it too.
Treatment: Acne conglobata is difficult to treat. The most common treatment is isotretinoin, often known by its brand name Accutane®, which is sometimes prescribed in combination with oral corticosteroids.

The Science
Definition
Acne conglobata, a rare, severe form of acne that normally affects 18 – 30-year-old males, is very difficult to treat, and often leaves massive, disfiguring scars.1,2
It falls under the umbrella term nodulocystic acne, which is used to refer to acne that features large, red, painful acne lesions called nodules and/or cysts. Acne conglobata also often comes with blackheads and lesions called draining sinuses, which are large lesions that are created when multiple cysts merge with one another.
Incidence
Acne conglobata is uncommon.
It can develop in people with existing acne or in people who have never had a problem with acne.
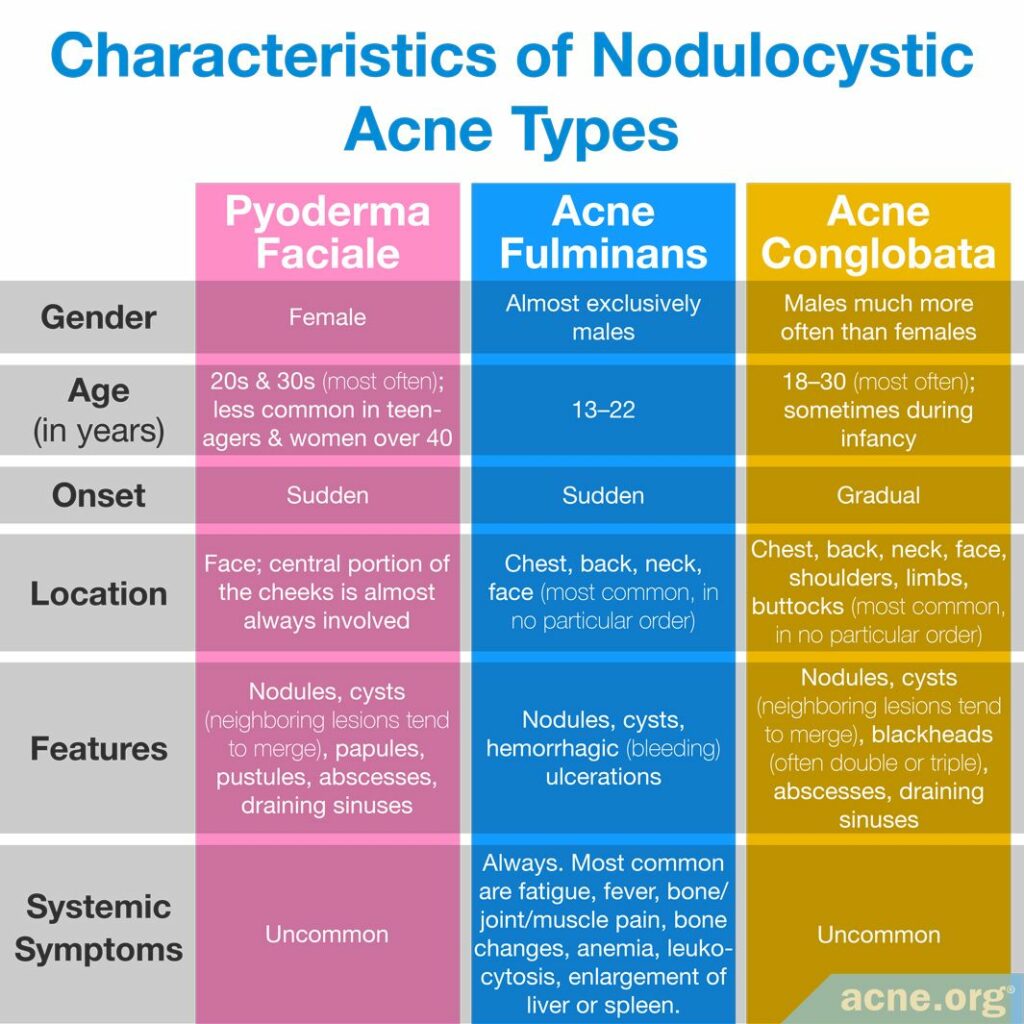
Typical patients are males between 18 and 30, though females can get it as well. Lesions begin to form in the late teen years, and the disease often persists into the late twenties and, sometimes, early thirties.2 In rare cases, infants may also suffer from the disease.1
For unknown reasons, the disease is more prevalent in tropical climates.3
Causes
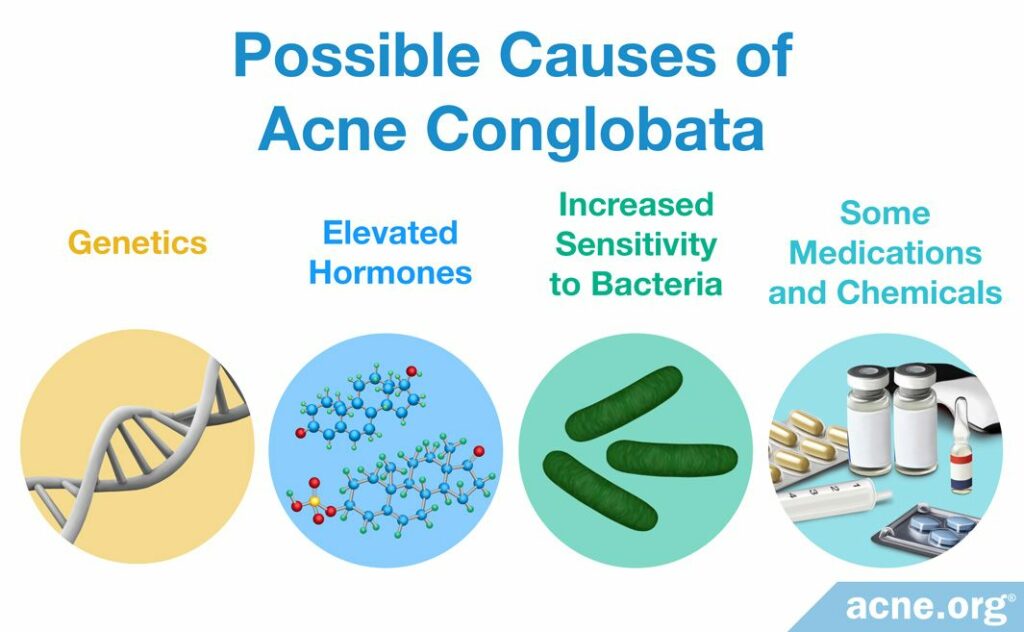
Nobody knows what causes acne conglobata, but the research suggests that the following four factors may play a role:
- Genetics: Researchers suspect there is a gene responsible for predisposition to acne conglobata because evidence shows that if a person’s parents had acne conglobata, that person’s chances of getting it are much higher. In addition, some males with acne conglobata suffer from a rare genetic condition called XYY syndrome, which means they have an extra Y chromosome.4
- Elevated hormones: Androgens (male sex hormones present in both males and females) very likely contribute to the disease. Increased dehydroepiandrosterone sulfate (DHEAS) and testosterone (both male sex hormones) are a frequent finding in patients with nodulocystic acne, but no major studies have been performed to determine if that is also true for acne conglobata.
- Increased sensitivity to bacteria: Some researchers hypothesize that an increased sensitivity to acne bacteria (C. acnes) causes the immune system in people with acne conglobata to overreact to the presence of the bacteria that, in other individuals, would bring about just regular acne.
- Some medications and chemicals: Occasionally, people who take thyroid medications may develop acne conglobata. Next, in some cases, using anabolic steroids may trigger acne conglobata. Lastly, being exposed to a type of chemicals called halogenated aromatic hydrocarbons may sometimes cause acne conglobata. This class of chemicals includes DDT, which is an insect repellent, and PCBs, which are found in some plastics and oil-based paints.4
Symptoms
Acne conglobata is an intense form of acne that affects large areas of the skin, including the chest, back, neck, face, shoulders, limbs, and buttocks, and very often leaves massive, disfiguring scars.5
It comes with a combination of lesions of all kinds, most notably nodules, cysts, blackheads, abscesses, and draining sinuses (several cysts merged together under the skin).1,2Whiteheads, papules, and pustules may be present as well, but they are not a dominant feature.
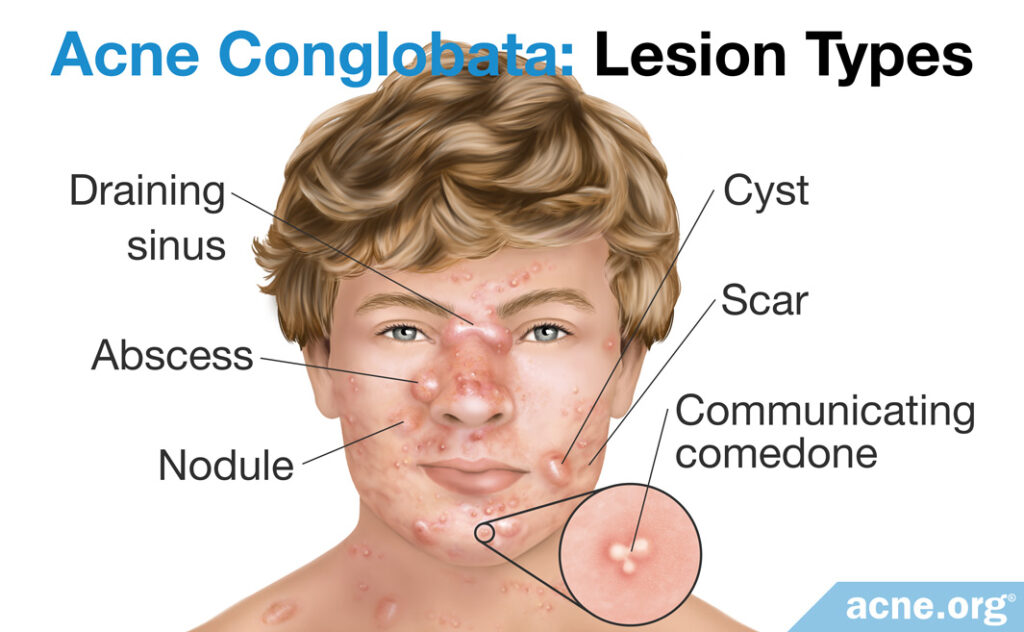
- Nodules and cysts: Nodules and cysts in acne conglobata are plentiful. Both types of acne lesions are over five millimeters in diameter and are tender and painful. The difference is that nodules are fibrous lesions that do not contain pus, whereas cysts contain “foul-smelling” pus-like material that returns after you drain them.
- Communicating comedones: Very typical of acne conglobata are lesions called communicating comedones, and can include double comedones and triple comedones, which are two to three blackheads that have merged into one extra-large blackhead. Communicating comedones commonly occur on the neck, the trunk, and, less frequently, on the upper arms and buttocks.1
- Abscesses: Abscesses are collections of pus that build up in the skin and tissue underneath the skin in response to harmful bacteria. They are red, painful, and feel fluid-filled when touched. Abscesses are surrounded by a wall of healthy cells, also called an abscess capsule, which the immune system builds to protect the body from the pus and bacteria inside the abscess.
- Draining sinuses: Draining sinuses are large, elongated lesions that form when two or more cysts merge together under the skin. Draining sinuses are a serious complication of chronic (persisting for a long time) acne conglobata. From the surface, a draining sinus is a red, elevated bump that is two to five centimeters long and periodically discharges pus. They are most common on the face, particularly between the nose and upper lip, and also on the neck.6
- Scars: Scars in acne conglobata are often widespread and can be atrophic (indented) or hypertrophic (raised above the skin).
Acne Conglobata Vs. Other Severe Forms of Acne
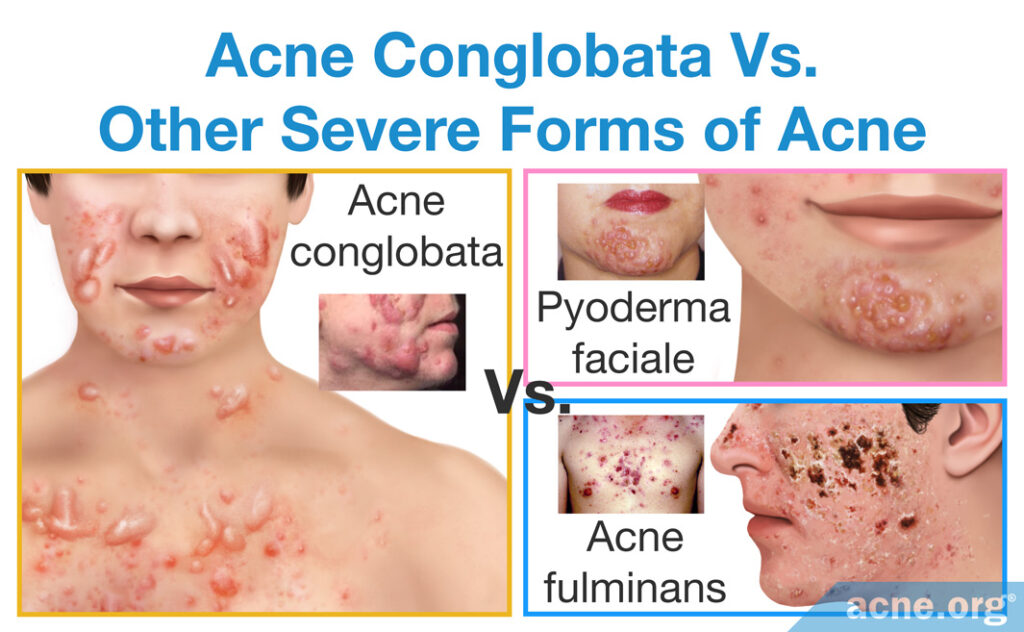
Acne conglobata is different from other severe forms of nodulocystic acne–acne fulminans and pyoderma faciale.
Acne fulminans
In acne fulminans, lesions tend to appear on the same areas of the face and body as in acne conglobata. Also, like in acne conglobata, neighboring nodules/cysts often merge together and form extra-large inflammatory lesions. What helps to differentiate between the two conditions is that nodules and cysts in acne fulminans fill with blood and rapidly turn into open wounds, while in acne conglobata they normally do not fill with blood and persist as raised lesions covered by the skin for long periods of time. In addition, acne fulminans comes with systemic symptoms (symptoms that affect the whole body), such as fever, joint pain, and weight loss, which are very uncommon in acne conglobata.7
Pyoderma faciale
Pyoderma faciale is another dramatic form of nodulocystic acne, characterized by a sudden emergence of intense redness and large merging nodules and/or cysts on the face. The disease is relatively easy to differentiate from acne conglobata because pyoderma faciale occurs exclusively in females and affects the face only.
Treatment

Acne conglobata is difficult but possible to treat. The oral medication isotretinoin is usually the go-to treatment and is normally prescribed for a course of 4 – 6 months. Studies show that isotretinoin reduces the total number of lesions by 60 – 95%, on average, depending on the dose and duration of treatment.8-10 However, it must be used only under close supervision by a doctor because it is associated with a wide array of worrying side effects, some of which can be lifelong.
Clinical trials on the effectiveness of isotretinoin in acne conglobata

In a 1979 study published in The New England Journal of Medicine, 14 patients with severe nodulocystic acne including, but not limited to, acne conglobata underwent a four-month treatment course with isotretinoin at a high dosage of 2mg/kg/day, which is more than usually prescribed these days.8 All but one patient, 75% of whose lesions cleared, experienced 100% clearance of the lesions. Most of the facial cysts/nodules cleared in the first month, while lesions on the trunk were more stubborn and took longer to resolve, particularly in males. Some degree of remission was achieved in all 14 patients. Twenty months after the completion of the treatment, 11 patients remained free of nodules/cysts, and the other 3 patients shared a total of nine cysts or nodules. The researchers did not specify how many cysts or nodules each person had, but we can say with assurance that they had drastically fewer than they had before treatment.

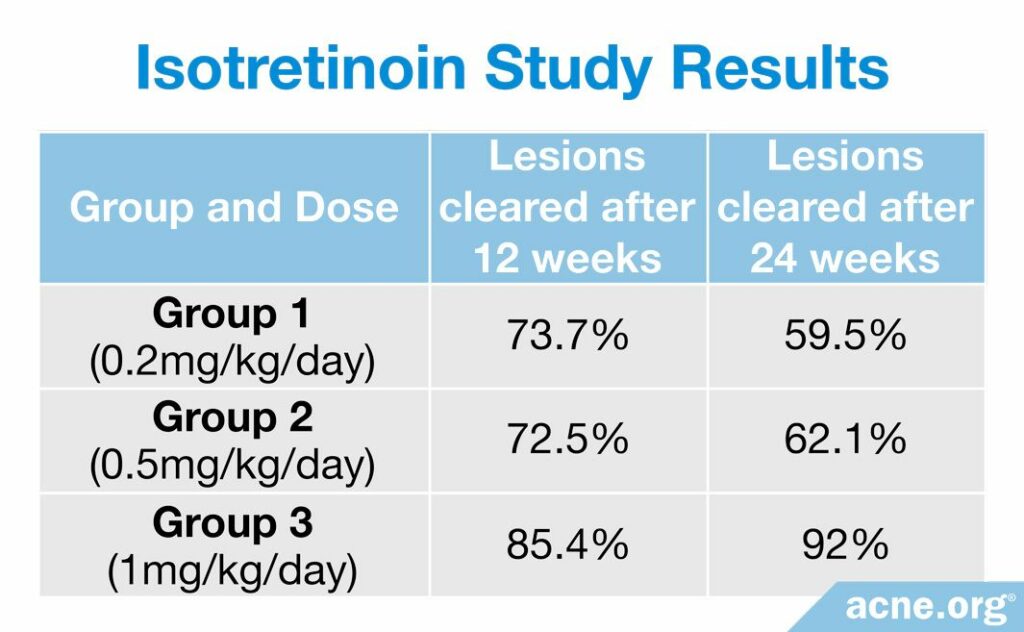
A study published in the German journal Der Hautarzt in 1983 reported good results with isotretinoin in 171 patients with acne conglobata.9 The patients were allocated to three groups, receiving either 0.2, 0.5, or 1 mg/kg/day of isotretinoin for 24 weeks. After 12 weeks, the researchers adjusted the dose based on how well acne cleared. If at least two thirds of lesions resolved, the initial dosage of 0.2 mg/kg/day was continued for another 12 weeks; 0.5 mg/kg/day was reduced to 0.2 mg/kg/day, and 1 mg/kg/day was either reduced to 0.2 mg/kg/day or isotretinoin simply was discontinued. If less than two thirds of lesions cleared, 0.2 mg/kg/day was raised to 0.5 mg/kg/day and 0.5 mg/kg/day was raised to 1 mg/kg/day. The patients in the 1 mg/kg/day group noticed the best results. Full results of the study are given in the table below.

A study on 46 patients, published in another German journal Zeitschrift für Hautkrankheiten in 1984, reported comparable results: after six months of therapy with isotretinoin, the overall number of lesions reduced, on average, by 94.4% on the face and 85.8% on the chest and back.10 The patients initially received 40, 60, or 80 mg of isotretinoin daily, which, for an average 70-kilo person, would equate to approximately 0.5 – 1 mg/kg/day, and the doses were then adjusted according to how well the patients responded to treatment.
Isotretinoin’s effectiveness in acne conglobata treatment likely lies in its ability to reduce production of sebum (skin oil).11-13 Sebum is a crucial factor in the development of acne. In fact, individuals who do not produce sebum, such as castrated men, never experience acne.
Clinical trials on how isotretinoin reduces sebum in people with nodulocystic acne

In a 1980 study in the Journal of the American Academy of Dermatology, 1 mg/kg/day of isotretinoin taken orally for 12 weeks reduced sebum production in patients with nodulocystic acne by almost 90%.10 A study published in the Journal of the American Academy of Dermatology in 1984 reported that 40 mg of isotretinoin daily for 16 weeks decreased the production of sebum by up to 55%.12

A 1986 study in the Journal of Investigative Dermatology discovered that as sebum production dropped with the administration of isotretinoin, the amount of C. acnes in the affected skin pores reduced as well.13 This makes sense because C. acnes feeds on sebum. This finding is particularly relevant because the study was performed on 40 patients with acne conglobata.
Despite being highly effective for severe acne, isotretinoin comes with a long list of side effects and, sometimes, even severe toxic reactions. This is why isotretinoin is approved for use only for severe, nodulocystic acne.
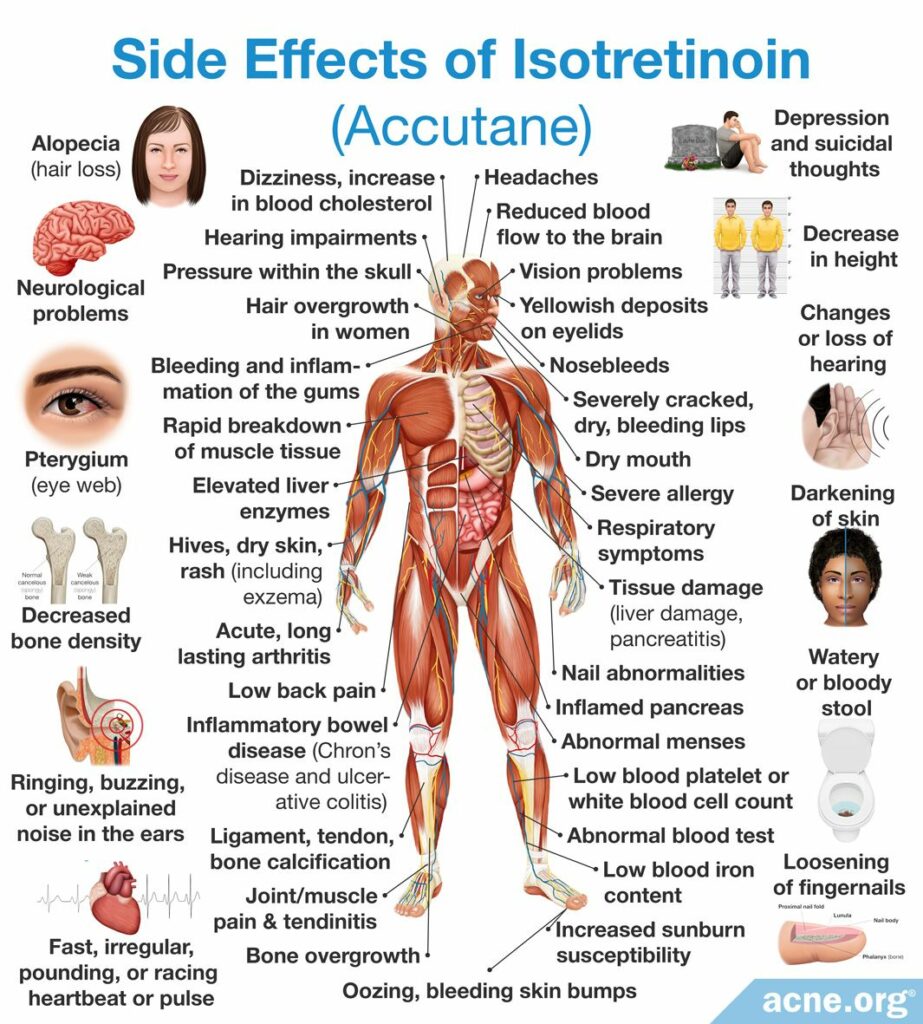
The most frequent side effects of isotretinoin include:
- Inflammation of lips (90%*)
- Dryness of skin and mucous membranes (80%)
- Pink eye (40%)
- Itching (40%)
- Gastrointestinal symptoms, such as nausea, vomiting, and abdominal pain (20%)
- Muscle and/or joint pain (16%)
- Increased sensitivity to light (10%)
*% incidence
Toxic reactions: Possible toxic reactions associated with the administration of isotretinoin might include inflammatory bowel disease and increased intracranial (in the head) pressure that causes moderate-to-severe headaches and visual impairments, such as blurred and double vision, difficulty seeing to the side, and brief episodes of blindness.14 The incidence of these events is unknown, but they are uncommon.
Lifelong side effects: Some side effects of isotretinoin may last forever. For instance, after taking a course of isotretinoin, the user may be left needing to regularly use lip balm for the rest of their life. In addition, because of concerns about permanent vision changes, the U.S. military will not allow anyone who has ever taken isotretinoin to be a fighter pilot.
EXTREME CAUTION! Isotretinoin is contraindicated in pregnancy due to its severe adverse effect on the fetus.14 In fact, isotretinoin is the leading birth defect-causing medication on the market. Birth defects are very severe, including death. This is why it is required that females obtain two (2) negative pregnancy tests prior to starting therapy. Additionally, females must use two (2) forms of contraception for 30 days before treatment, throughout treatment, and for 30 days after treatment with isotretinoin.
Oral corticosteroids are sometimes added
Simultaneous administration of oral corticosteroids (e.g., prednisone) in the first two to four weeks of an isotretinoin course may quickly reduce inflammation and give the treatment a head start.1,15
Alternative treatments

- Tetracycline oral antibiotics: Tetracyclines are sometimes prescribed as alternatives to isotretinoin, although their effectiveness in acne conglobata has not been established.1 Tetracyclines should never be combined with isotretinoin because of a risk of increased intracranial pressure.17 Instead, tetracycline oral antibiotics can sometimes be combined with topical retinoids such as tretinoin, adapalene, tazarotene, and trifarotene.18
- Cryotherapy: Cryotherapy requires a doctor or nurse to apply a probe with a cooling agent directly onto nodules/cysts, cooling down the lesions to temperatures at which they “die.” The method may help to get rid of a few particularly stubborn nodules/cysts, but does not treat the cause of acne conglobata. In other words, cryotherapy does not get to the root of the disease, but may help to heal existing nodules/cysts.
Clinical trial on cryotherapy in acne conglobata

A study published in 1974 in the British Journal of Dermatology investigated the ability of cryotherapy to treat 25 patients with acne conglobata.16 Most lesions resolved within 7 – 10 days and did not return at the follow-ups 12 – 28 months later.
- Photodynamic therapy: Photodynamic therapy is a painful procedure that includes illuminating the affected areas of skin with powerful medical lamps (usually red light) after applying a special substance called a sensitizing agent. Photodynamic therapy may prove to be a valuable alternative to isotretinoin, but more research is still needed on exactly the right way to use it for acne conglobata. Of concern, one study showed that photodynamic therapy worsened the symptoms of the disease in about 1 in 6 people.
Clinical trial on photodynamic therapy in acne conglobata
A study published in Photodermatology, Photoimmunology & Photomedicine in 2013 reported treating acne conglobata on the face with red light photodynamic therapy.17 The investigators applied a sensitizing agent, called 5-aminolevulinic acid (ALA), onto facial skin and illuminated the cysts with red light for 20 minutes. After three procedures, 88% (28/32) of the patients had their cysts cleared. However, 16% (5/32) of the patients developed significant swelling and pain in the areas exposed to light, and the number of cysts increased.
- Oral dapsone: Dapsone is an antibacterial and anti-inflammatory medication used to treat several skin conditions unrelated to acne. However, one case report described a patient with acne conglobata who had experienced no improvement on isotretinoin but cleared up after taking oral dapsone. More research is necessary to determine whether oral dapsone is a good alternative to isotretinoin for people with acne conglobata.4,19
Case report on oral dapsone in acne conglobata

A case report published in 2018 in the Oman Medical Journal described a 21-year-old male with acne conglobata. The patient took oral isotretinoin at various doses for several months but experienced no significant improvement. In fact, his acne worsened. His doctor then prescribed oral dapsone, first at a dose of 100 mg/day for four months, and then at a dose of 50 mg/day for another two months. After this treatment, the patient’s acne improved to the level of mild acne. The report authors wrote, “Oral dapsone…might also be a promising and hopeful alternative treatment for [acne conglobata] when isotretinoin fails.”19
Other emerging treatments: Some preliminary research suggests that medications called infliximab (brand name Remicade®) and adalimumab (brand name Humira®), which are used to treat autoimmune diseases like Crohn’s disease, might also help with acne conglobata. These medications suppress the body’s immune response. Since an overactive immune response might also play a role in severe acne, it makes sense that a medication like infliximab or adalimumab might help.18 However, more research into this emerging treatment is needed.
Laser therapy, specifically carbon dioxide (CO2) laser, might also show promise for acne conglobata. In general, laser therapy is known to improve acne scars but tends to be less effective for acne. New research will show whether it can produce substantial results in acne conglobata.
Finally, external beam radiation, which is a type of radiation therapy used to treat cancer patients, might also help with acne conglobata, but at this point, we do not have enough information to say how effective it might be.4
References
- Schwartz, R. “Acne Conglobata”. Emedicine.medscape.com. 2017. Web. 10 June 2017. https://emedicine.medscape.com/article/1072716-overview
- Habif, T. Clinical Dermatology: A Color Guide to Diagnosis and Therapy (6th Edition). 231 – 233 (Saunders, 2015) https://www.elsevier.com/books/clinical-dermatology/habif/978-0-323-26183-8
- Morris-Jones, R. & Meaden, A. ABC Of Dermatology. 92 (2014) https://archive.org/stream/ABCOfDermatology6E/ABC of Dermatology 6E_djvu.txt
- Hafsi, W. & Badri, T. Acne Conglobata. [Updated 2019 May 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459219/
- Kalashnikova, N. G., Albanova, V. I. & Jafferany, M. Laser treatment of acne conglobatа with concomitant oral isotretinoin use. Dermatol Ther 34, e14553 (2021). https://pubmed.ncbi.nlm.nih.gov/33205848/
- Jansen, T., Lindner, A. & Plewig, G. Draining sinus in acne and rosacea. A clinical, histopathologic and experimental study. Hautarzt 46, 417 – 420 (1995) https://pubmed.ncbi.nlm.nih.gov/7642386/
- Jansen, T. & Plewig, G. Acne fulminans. Int J Dermatol 37, 254 – 257 (1998). https://link.springer.com/chapter/10.1007/978-3-642-59715-2_24
- Peck, G. et al. Prolonged Remissions of Cystic and Conglobate Acne with 13-cis-Retinoic Acid. New Engl J Med 300, 329 – 333 (1979) https://pubmed.ncbi.nlm.nih.gov/153472/
- Meigel, W., Gollnick, H., Wokalek, H. & Plewig, G. Oral treatment of acne conglobata using 13-cis-retinoic acid. Results of the German multicentric study following 24 weeks of treatment. Der Hautarzt 34, 387 – 397 (1983) https://www.karger.com/Article/Abstract/17848
- Schmidt, J. & Fanta, D. 13-cis-retinoic acid-an effective therapy for acne conglobata. Zeitschrift fur Hautkrankheiten 59, 279 – 287 (1984) https://pubmed.ncbi.nlm.nih.gov/6232766/
- Farrell, L., Strauss, J. & Stranieri, A. The treatment of severe cystic acne with 13-cis-retinoic acid. J Am Acad Dermatol 3, 602 – 611 (1980) https://www.ncbi.nlm.nih.gov/pubmed/6451637
- Strauss, J. et al. Isotretinoin therapy for acne: Results of a multicenter dose-response study. J Am Acad Dermatol 10, 490 – 496 (1984) https://pubmed.ncbi.nlm.nih.gov/6233335/
- Leyden, J., McGinley, K. & Foglia, A. Qualitative and Quantitative Changes in Cutaneous Bacteria Associated with Systemic Isotretinoin Therapy for Acne Conglobata. J Invest Dermatol 86, 390 – 393 (1986) https://pubmed.ncbi.nlm.nih.gov/2943823/
- Hodgson, B. & Kizior, R. Saunders nursing drug handbook 2012. (W. B. Saunders Co., 2014)
- Hafsi, W., Arnold, D. L. & Kassardjian, M. Acne Conglobata. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023. https://pubmed.ncbi.nlm.nih.gov/29083736/
- Leyden, J., Mills, O. & Kligman, A. Cryoprobe treatment of acne conglobata. Br J Dermatol 90, 335 – 341 (1974) https://pubmed.ncbi.nlm.nih.gov/4274644/
- Yang, G. et al. Short-term clinical effects of photodynamic therapy with topical 5-aminolevulinic acid for facial acne conglobata: an open, prospective, parallel-arm trial. Photodermatol Photoimmunol Photomed 29, 233 – 238 (2013). https://pubmed.ncbi.nlm.nih.gov/24001378/
- Greydanus, D. E., Azmeh, R., Cabral, M. D., Dickson, C. A. & Patel, D. R. Acne in the first three decades of life: An update of a disorder with profound implications for all decades of life. Dis Mon 67, 101103 (2021). https://pubmed.ncbi.nlm.nih.gov/33041056/
- Al-Kathiri L, Al-Najjar T. Severe nodulocystic acne not responding to isotretinoin therapy successfully treated with oral dapsone. Oman Med J 33, 433‐436 (2018). https://pubmed.ncbi.nlm.nih.gov/30210724/
 Acne.org Products
Acne.org Products