An Acne Cyst Is a Large Acne Lesion Filled with Fluid or Pus

The Essential Info
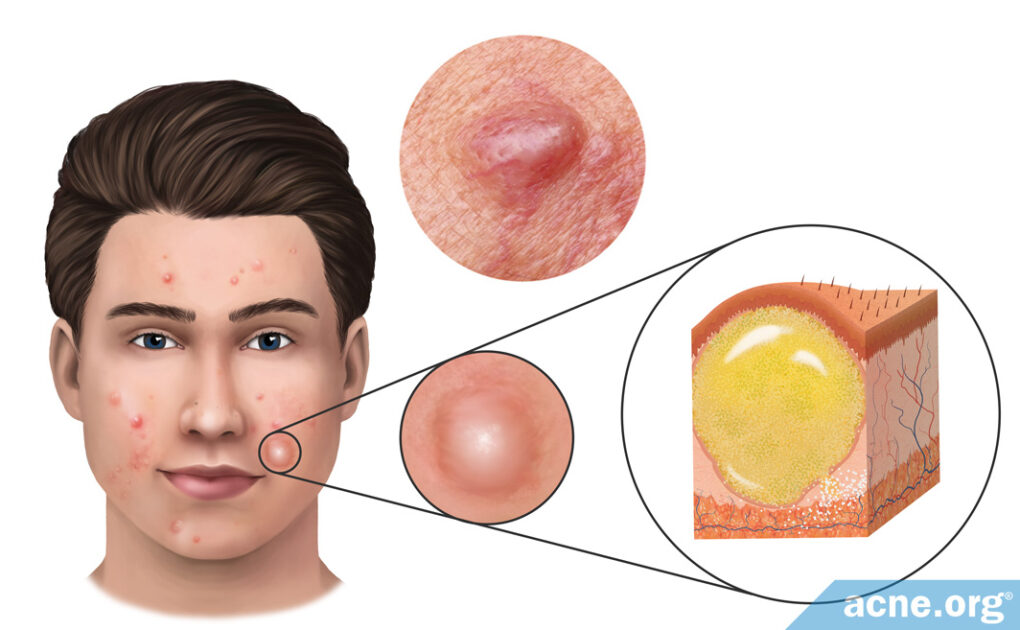
Acne cysts are very large (7 – 15 mm in diameter), skin-colored or red lesions that are filled with liquid or pus. They most often affect males in their teens and early 20s, and are part of a type of acne called “nodulocystic acne,” or more simply, “cystic acne.”
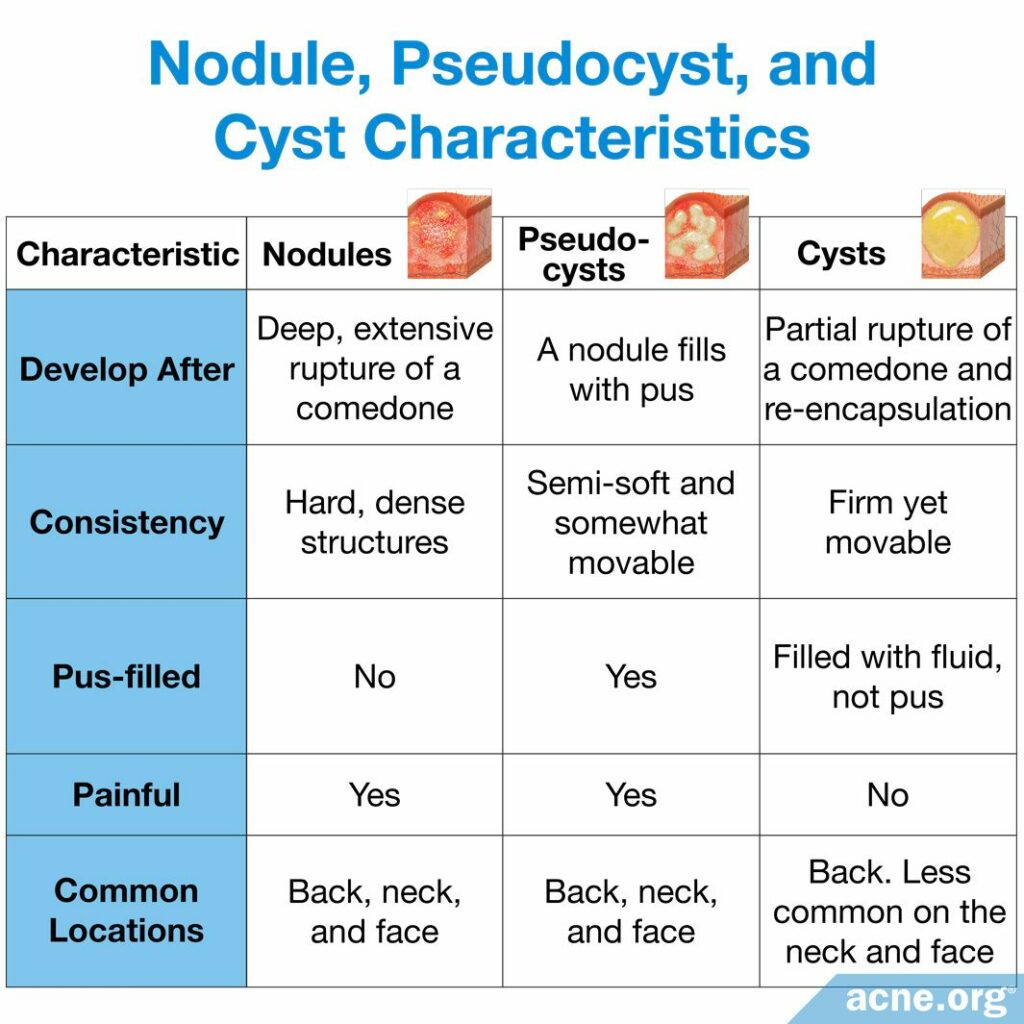
Not to be confused with a nodule: People often refer to a large acne lesion as a “cyst” when in fact most nodulocystic acne lesions are nodules. Nodules are firm, fibrous lesions that are not filled with liquid or pus and cannot be drained because there is nothing inside to come out. Acne cysts on the other hand, are soft to the touch because they have something that “fills them up.” There are two types of cysts:
- True acne cysts (extremely rare): A true cyst is a very large lesion, most often found on the back, that is filled with fluid, skin cells, oil, bacteria, and hair. They can last for months or even years, and very often leave scars behind.
- Pseudocysts: Sometimes an acne nodule can fill with pus. In that case, it is often referred to as a cyst, but is actually just a pus-filled nodule. They are most often found on the back, neck, and face, can last for weeks or months, and often leave scars behind.
Treatment Options:
- Benzoyl peroxide
- Isotretinoin (Accutane®)
- Oral antibiotics
- Cortisone shots
- Cryotherapy
- Photodynamic therapy
- Incision and draining
- Hormonal treatment (females only)
Never Attempt to Pop A Cyst! You should never, under any circumstance, attempt to pop or drain a cyst on your own. It won’t work and will very likely lead to increased scarring. Always see a dermatologist for this.

The Science
- Characteristics of Acne Cysts
- How Cysts Develop
- What Causes Acne Cysts?
- Never Attempt to Pop a Cyst
- Treatment Options for Acne Cysts
An acne cyst is a severe acne lesion that occurs in people with severe acne and differs from other cysts in the body. When you hear about someone having a “cyst” somewhere on the body, these cysts are like small balls filled with liquid or air, and they contain a lining that forms a sac to hold the contents. This sac never contains pus. However, in acne, there are two types of cysts: one without pus and one with pus.
- True cysts (rare – without pus): A “true” cyst is similar to other cysts in the body, as it has a lining and contains no pus. These cysts are filled with fluid, skin cells, skin oil, and hair.
- Pseudocysts (with pus): A pseudocyst, or “fake” cyst, differs from other cysts in the body because it has no lining and is filled with pus. Acne cysts are most always pseudocysts, which develop from acne nodules–red, swollen, fibrous acne lesions that do not contain liquid or pus. Pseudocysts form when acne nodules fill with pus, so an acne cyst is essentially a pus-filled acne nodule.1-3
Characteristics of Acne Cysts
True acne cysts (rare)
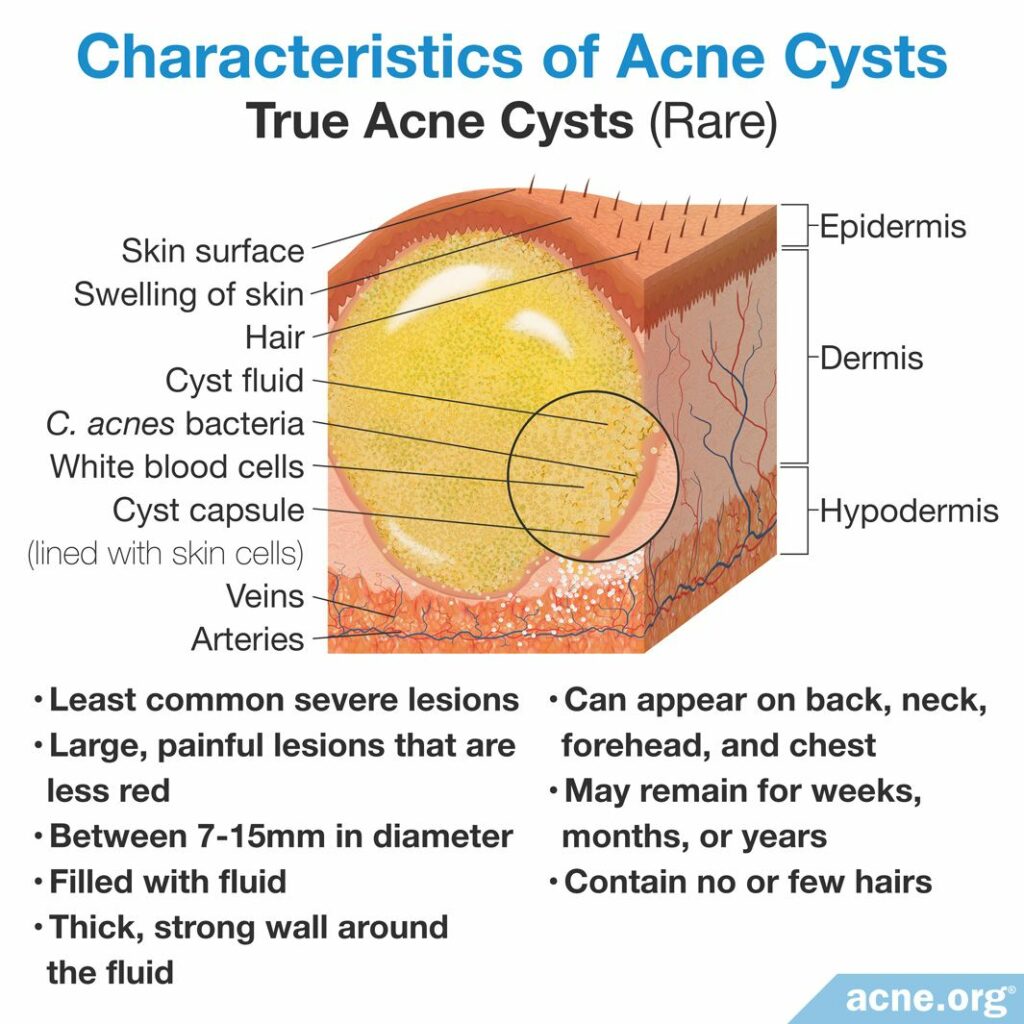
True acne cysts are smooth, skin-colored, painless bumps that appear somewhat raised above the skin and are normally between 7 and 15 millimeters in diameter. They are also called epidermoid cysts. Occasionally, one can grow up to five centimeters in diameter. Sometimes neighboring cysts may merge as well.
True acne cysts are most often found on the back, but are also found to a lesser extent on the face, neck, and earlobes.
Acne cysts have a lining that keeps the contents encapsulated. To the touch, these cysts feel soft, and movement of the cyst’s contents can be felt beneath the skin. Although you should never, under any circumstance, attempt this yourself, true acne cysts release a cheesy or waxy material that gives off a foul, rotting smell when squeezed or cut open with a scalpel by a doctor. Occasionally, a true acne cyst releases its foul-smelling contents spontaneously onto the surface of the skin. These components include fluid, dead skin cells, skin oil, some bacteria, and remnants of hairs.4
True acne cysts are stubborn acne lesions and can remain on the skin for months or years, and often leave scars.
Abscesses (also rare)
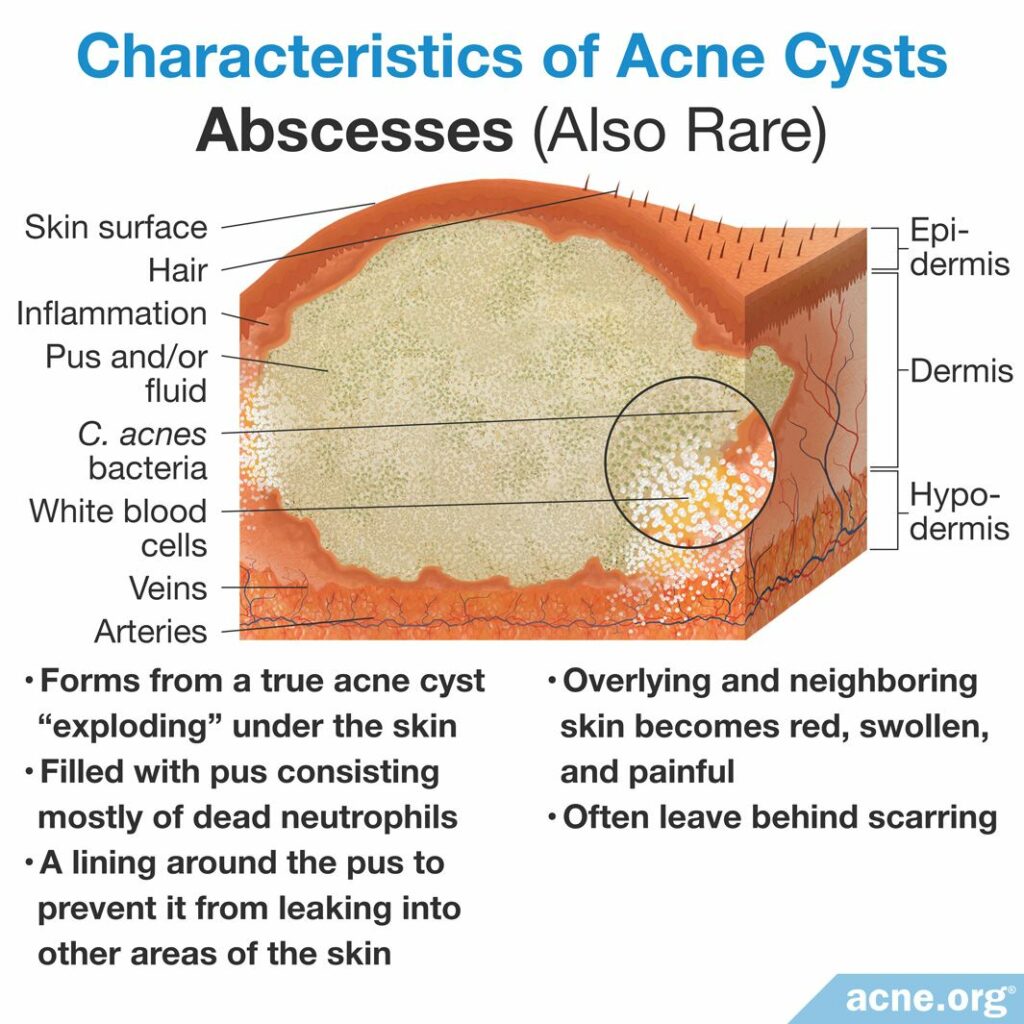
A true acne cyst will at some point “explode” under the skin. Abscesses are lesions that form when this occurs. After the cyst rupture, the area begins to fill with pus. Pus is a white or yellow fluid consisting mostly of dead immune cells called neutrophils. As more dead neutrophils accumulate, more pus fills the burst acne cyst. Eventually, the body forms a lining around this pus to prevent it from leaking into other areas of the skin. Once an abscess forms, the overlying and neighboring skin becomes red, swollen, and painful. Like true acne cysts, abscesses often leave behind scarring.
Pseudocysts (more common)
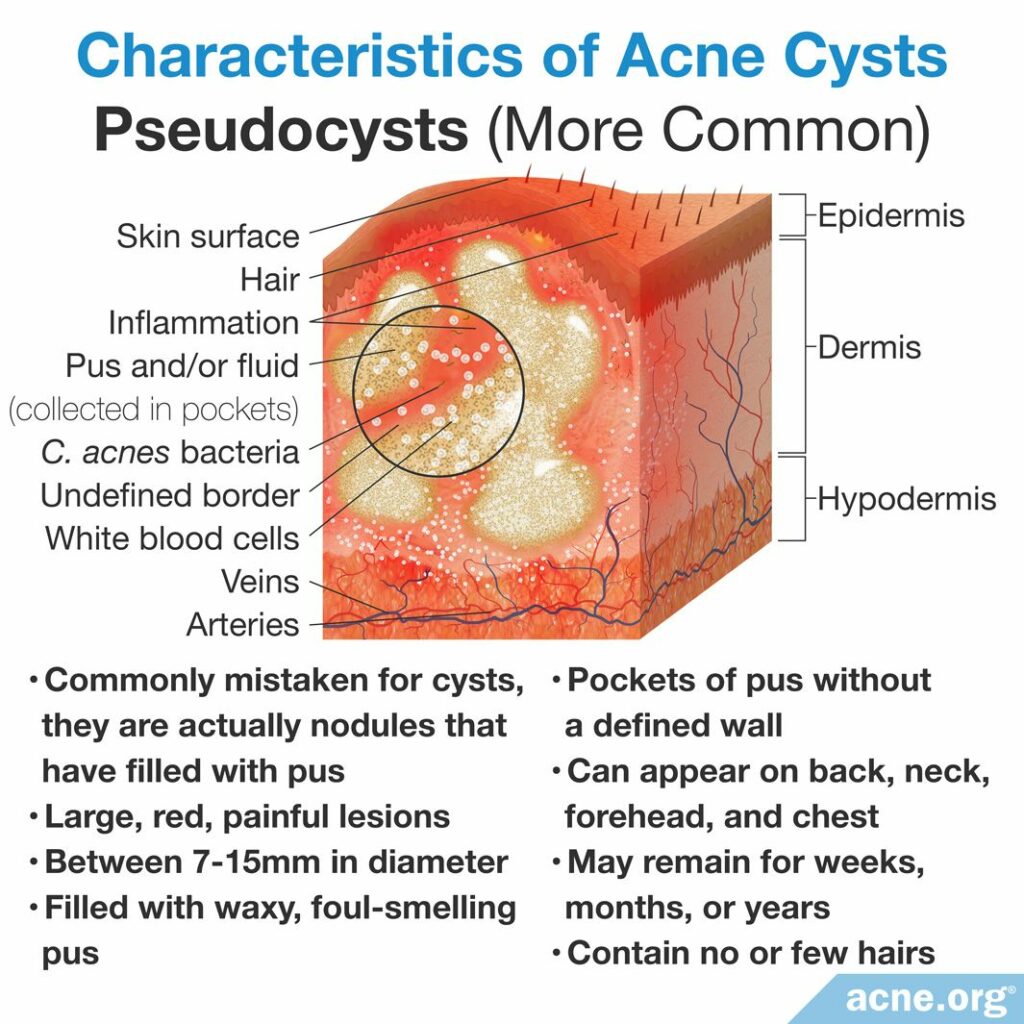
Pseudocysts, or “fake” cysts, are deep, red, swollen, sore bumps that contain pus. They form from acne nodules that fill with pus, but do not contain the lining that true cysts or abscesses have. This pus makes pseudocysts soft, and can be felt beneath the skin when they are touched or squeezed. Pseudocysts are by far the most common form of acne cysts, and are the most common cyst in nodulocystic acne, which is a type of acne with multiple nodules and pseudocysts.1-3
Pseudocysts are most often located on the cheeks, followed by the temple region, and then the chin.5
How Cysts Develop
Since they are most common, let’s first look at how pseudocysts develop.
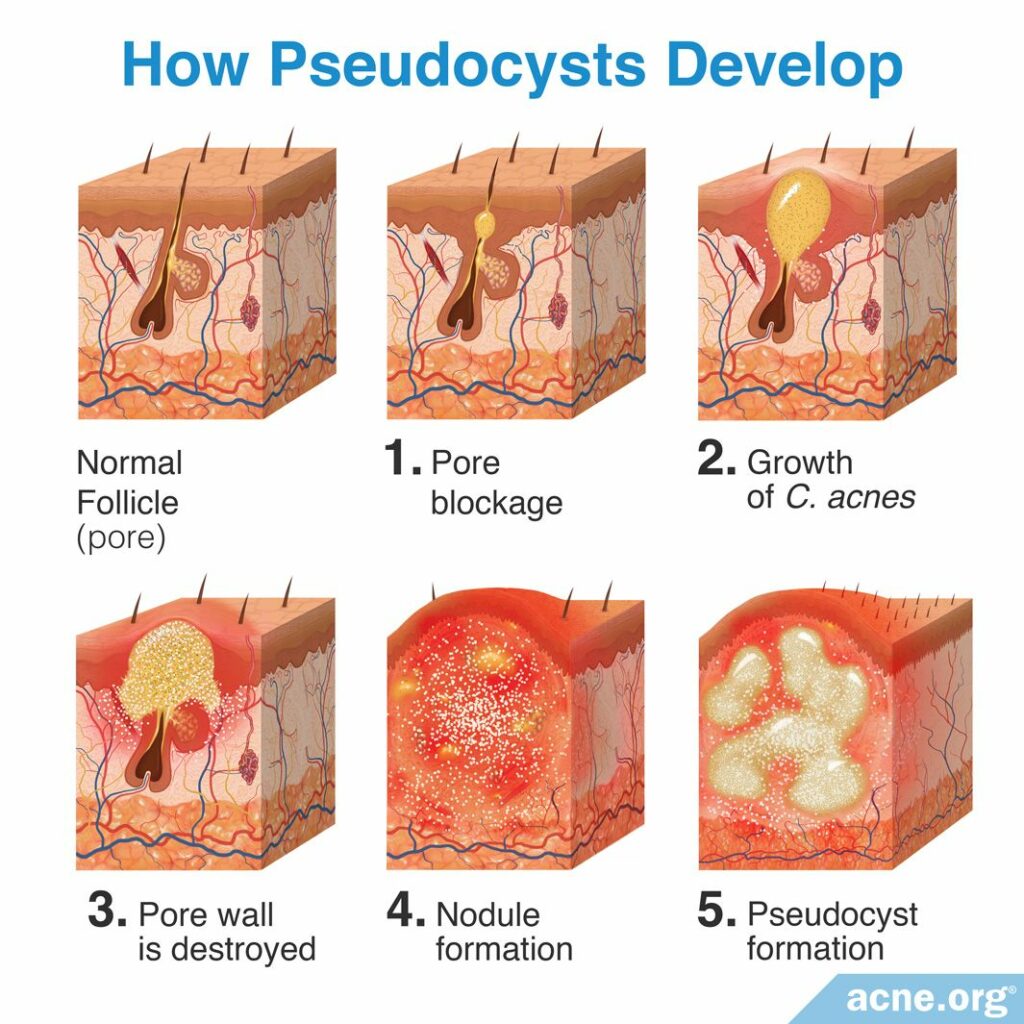
Step 1 – Pore blockage: All acne lesions begin with microscopic hair follicles, often referred to as pores. Attached to these hair follicles are glands, called sebaceous glands, that produce skin oil, called sebum. Normally, sebum is freely expelled from the hair follicle and onto the surface of the skin. Acne develops when skin cells called keratinocytes (cells of the top layer of the epidermis) block the hair follicle, and this blockage results in sebum accumulating inside the pore.
Step 2 – Growth of C. acnes: A blocked pore contains a large accumulation of sebum, but little to no oxygen, which is the ideal environment for skin bacteria called Cutibacterium acnes (C. acnes) to reproduce.
Step 3 – Pore wall is destroyed: Small amounts of acne bacteria (C. acnes) in healthy pores are expected, but as the amount of C. acnes inside the pore increases, the body responds by sending in immune system cells called neutrophils to clear out the C. acnes and its byproducts. Neutrophils release enzymes that attack C. acnes to clear it from the clogged pore, causing the bacteria to fight back by releasing chemicals. However, these chemicals not only damage the neutrophils, but also weaken the pore wall, which eventually causes the pore to rupture.
Step 4 – Nodule formation: Papules, and pustules, commonly referred to as “pimples” or “zits,” develop when only a small portion of the wall ruptures and releases the contents of the pore only in the upper areas of the skin. Nodules develop when the rupture destroys the follicular wall, and the contents of the pore are released into much deeper areas of the skin, forming a firm, fibrous lesion that is not filled with fluid or pus.
Step 5 – Pseudocyst formation: Over the course of a few days, sometimes nodules fill with pus, and are then called pseudocysts.
Now let’s look at how a true cyst develops.
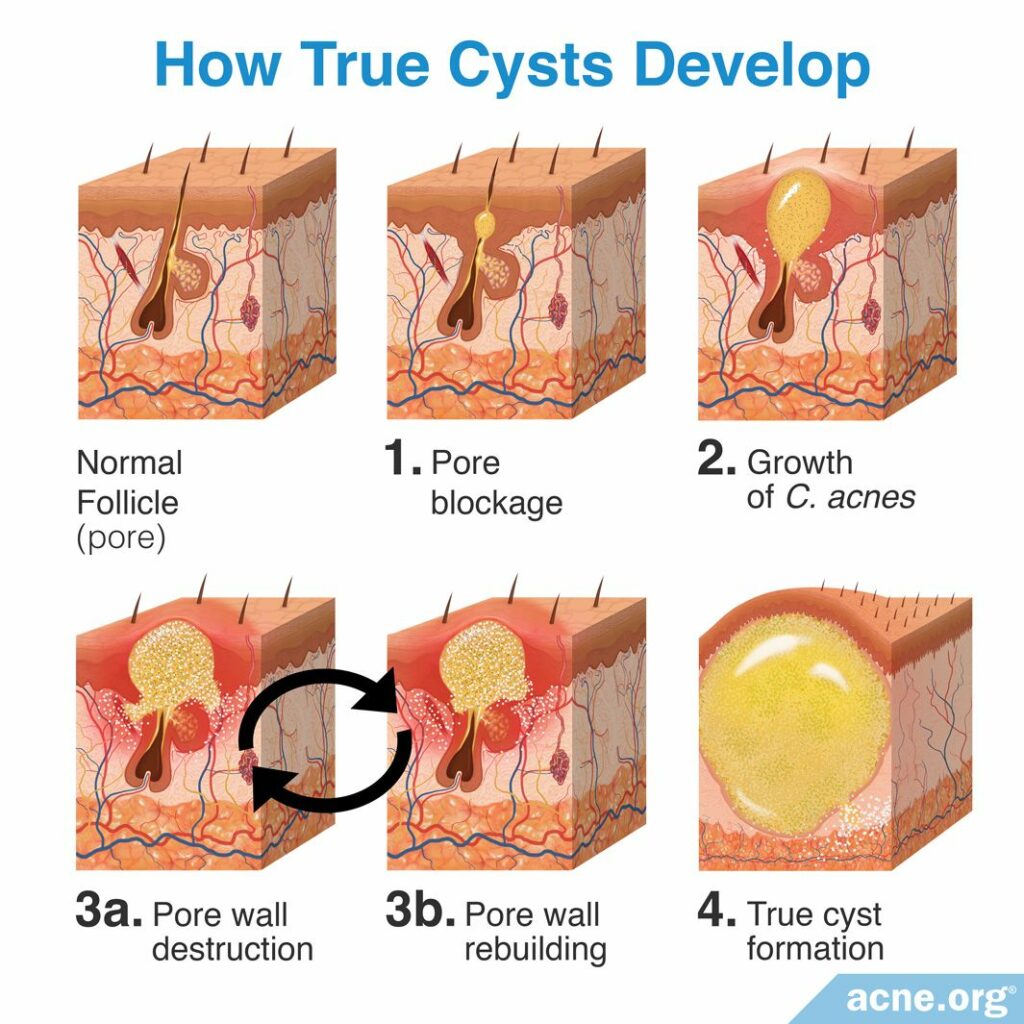
It starts in much the same way as a pseudocyst, with a clogged pore that fills with sebum, the growth of acne bacteria, and a breakage of the pore wall. However, a true acne cyst forms when the pore wall rupture only partially destroys the wall, and the body repairs the wall after the rupture. During the formation of a true cyst, there can be repeated episodes of wall rupture and reconstruction. With each rupture and rebuilding, the amount of C. acnes inside the cyst begins to decrease for an unknown reason. During each one of these rupture-and-rebuilding cycles, the wall becomes thinner. This causes the wall to become more flexible, allowing for it to stretch as it fills up with mostly dead skin cells, but also sebum, C. acnes, and remnants of hairs. These contents become the foul-smelling, cheesy/waxy material found inside of a true cyst.6-8
What Causes Acne Cysts?
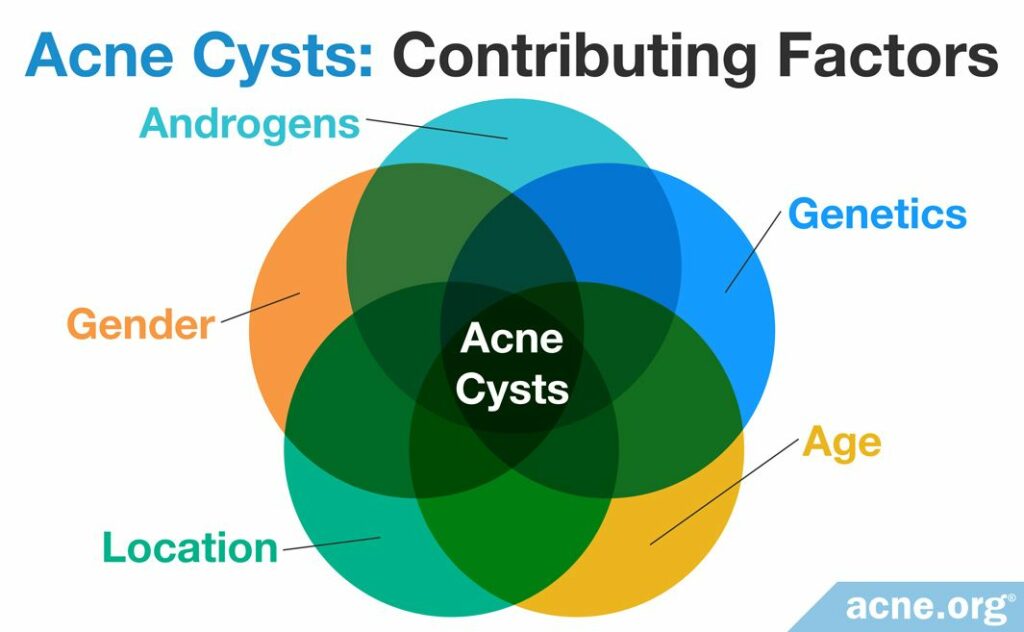
Several characteristics make developing nodulocystic acne more likely:
- Hormones: Androgens are male hormones present in both males and females, and many acne patients with acne nodules and cysts possess increased androgen levels. Higher levels of these hormones increase the production of sebum, and this may lead to more acne and more severe forms of acne.
- Genetics: A person is more likely to develop acne nodules and cysts if a close relative also suffered from nodulocystic acne. Because of this, scientists believe that one or more genes may be involved in the development of severe acne lesions, including acne cysts.
- Age: People are more likely to develop acne pseudocysts during their teenage years or early 20s. Acne is more commonly observed during these ages due to hormonal changes that occur during this time.
- Gender: In general, males are more likely to develop severe acne nodules and cysts. However, females can also suffer from nodulocystic acne and, while uncommon, are more likely to develop it during pregnancy, especially during the third trimester.
- Location: Nodulocystic acne is more common in people who live in tropical regions of the world, and ongoing research is attempting to determine why this occurs.9
Never Attempt to Pop a Cyst
You should never try to pop a true acne cyst or a pseudocyst. Both types of acne cysts lie deep within the skin. Attempting to pop either acne cyst will likely result in releasing the contents of the cyst deeper into the skin. This would only make the cyst worse, and is more likely to leave scars and permanently damage the skin. Therefore, acne cysts should always be treated by a medical professional.10,11
Treatment Options for Acne Cysts
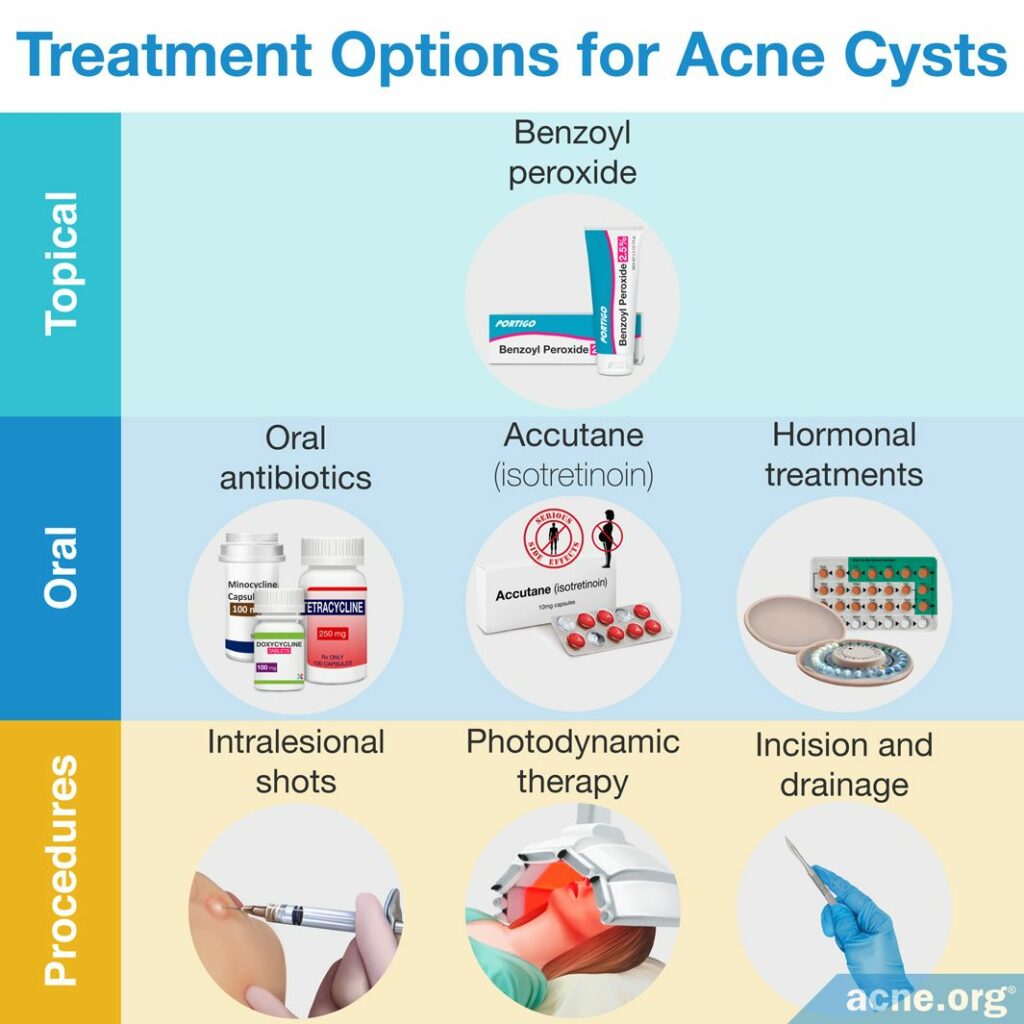
The treatment options for true acne cysts and pseudocysts are different. Let’s start by looking at treatments for pseudocysts.
Treating pseudocysts
Since pseudocysts develop from acne nodules, the treatment options for clearing acne nodules will also work to clear acne pseudocysts:
- A properly applied benzoyl peroxide regimen: To prevent future nodules, applying benzoyl peroxide in the correct manner can stop the development of any type of acne lesion, including nodules.
- Accutane® (isotretinoin) and corticosteroids: Isotretinoin (Accutane®) is only approved for severe acne, and for good reason. It is an oral medication that permanently and irreversibly changes the entire body. It is a treatment of last resort for extreme cases of severe acne. When cysts and/or nodules are numerous, severe, widespread, and deeply scarring, doctors sometimes advise its use, often combined with oral corticosteroids.12 Doctors usually prescribe corticosteroids for the first two to four weeks of treatment because corticosteroids work much faster than isotretinoin and can quickly decrease inflammation, redness, and pain. A few weeks into the corticosteroid treatment, patients begin taking an isotretinoin dosage of 0.5 – 1 milligram/kilogram/day, normally for 15 – 20 weeks. Isotretinoin is the workhorse that ends up clearing the skin and is highly effective, but taking it is a serious decision. Side effects include sometimes lifelong changes to the body, and the drug predictably causes drastic birth defects or fetal death if taken by pregnant women. Due to the severity of side effects and the permanent changes to the body, many people prefer to forgo isotretinoin treatment and embark on other treatment options.
- Oral antibiotics: Oral antibiotics, including minocycline, doxycycline, and tetracycline are alternatives to isotretinoin that can only temporarily reduce acne pseudocysts. They should be used for a maximum of three months, and during this time they may partially clear the skin of some acne pseudocysts. Oral antibiotics also come with side effects, including gastrointestinal issues, and can permanently stain the teeth or skin. Oral antibiotics should never be taken with isotretinoin because there is a risk of developing a disease called pseudotumor cerebri, which causes a buildup of pressure inside the skull.13
- Intralesional shots (cortisone shots): Intralesional shots, otherwise known as cortisone shots, are corticosteroid injections directly into an acne pseudocyst. This reduces inflammation and helps to heal the lesion and prevent scarring. Intralesional shots are effective at clearing one pseudocyst or a few pseudocysts, but are not a feasible treatment option for those with numerous and widespread pseudocysts.
- Photodynamic therapy: A less common treatment for acne pseudocysts is photodynamic therapy. This painful but sometimes effective therapy is performed by treating the skin with a photosensitizing agent followed by illumination with light, usually red light. There is little research on the effectiveness of this treatment option, but it shows some promise in treating nodulocystic acne, and can be an alternative to isotretinoin.14
- Incision and draining: Doctors can treat a pseudocyst by cutting it open and draining the pus. Cutting and draining a pseudocyst is a procedure that must only be performed by a medical professional, as it involves cutting open the cyst in sterile conditions and draining the cyst of its contents. This procedure should never be attempted at home.
- Hormonal treatments (females only): Hormonal treatments, including oral contraceptives (birth control) and spironolactone (anti-androgen), are treatments females can use to clear acne pseudocysts. These treatments work by balancing hormones. Hormonal treatments can only be taken by females because they can cause feminization symptoms, including breast growth and sexual dysfunction in males. In females, however, these treatments can be highly effective at clearing and preventing acne pseudocysts.
Doctors will often treat acne pseudocysts with a combination of the above therapies. For instance, one common therapy for acne patients with only a few pseudocysts includes a combination of short-term oral antibiotics, conventional topical therapies such as benzoyl peroxide or retinoids (tretinoin, adapalen, or tazarotene), and cortisone shots. This combination can be highly effective at clearing the skin of a few pseudocysts, with minimal side effects.15
Treating true cysts
The main treatment for true acne cysts is to drain the contents of the cyst. This procedure must only be performed by a medical professional, as it involves cutting open the cyst with a needle or blade in sterile conditions and draining the cyst of its contents. This should never be attempted at home, and doing so will most likely result in a much more severe lesion and potentially radically increased scarring. Once the cyst is drained, it can heal and clear from the skin. True acne cysts should not be treated with antibiotics, isotretinoin, or hormonal therapies used for pseudocysts.11
References
- Usatine, R., Quan, M. & Strick, R. Acne Vulgaris: A Treatment Update. Hosp Pract 33, 111 – 127 (1998). https://www.ncbi.nlm.nih.gov/pubmed/9484299
- Usatine, R. & Quan, M. Pearls in the management of acne. Prim Care 27, 289 – 308 (2000). https://www.researchgate.net/publication/12502963_Pearls_in_the_management_of_acne_An_advanced_approach
- Oberemok, S. & Shalita, A. Acne vulgaris, I: Pathogenesis and diagnosis. Cutis 70, 101 – 105 (2002). https://www.ncbi.nlm.nih.gov/pubmed/12234155
- Hoang, V. T., Trinh, C. T., Nguyen, C. H., Chansomphou, V., Chansomphou, V. & Tran, T. T. T. Overview of epidermoid cyst. Eur J Radiol Open 6, 291‐301 (2019). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6732711/
- Wortsman, X., Claveria, P., Valenzuela, F., Molina, M. T. & Wortsman, J. Sonography of acne vulgaris. J Ultrasound Med 33, 93‐102 (2014). https://www.ncbi.nlm.nih.gov/pubmed/24371103
- Plewig, G. & Kligman, A. Acne and Rosacea. (Springer International PU, 2000). https://www.springer.com/gp/book/9783642640964
- Mascaro, J. Pathogenesis of acne. J Dermatolog Treat 11, 1 – 4 (2000). https://www.tandfonline.com/doi/abs/10.1080/09546630050517739-1
- Plewig, G. & Kligman, A. Acne. 108 – 119 (Springer Verlag, 1975). https://www.springer.com/gp/book/9783642962462
- Arndt, K. Manual of Dermatologic Therapeutics (7th Edition). 5 – 8 (LWW (PE), 2007).
- Zaidi, Z. Dispelling the myths and misconceptions of acne. J Pak Med Assoc 59, 264 – 265 (2009). https://jpma.org.pk/article-details/1684
- Pimple popping: Why only a dermatologist should do it | American Academy of Dermatology. Aad.org (2017). https://www.aad.org/diy/pimple-popping
- Chien, A. L., Qi, J., Rainer, B., Sachs, D. L. & Helfrich, Y. R. Treatment of acne in pregnancy. J Am Board Fam Med 29, 254-262 (2016). https://pubmed.ncbi.nlm.nih.gov/26957383/
- Schwartz, R. Acne Conglobata Treatment & Management: Medical Care, Surgical Care, Consultations. Emedicine.medscape.com (2016). https://emedicine.medscape.com/article/1072716-treatment
- Yao, Y., Zuo, J. & Chen, L. Clinical efficacy of tanshinone capsules combined with varying concentrations of 5-ALA-PDT in the treatment of cystic acne. Am J Transl Res 13, 10816-10822 (2021). https://pubmed.ncbi.nlm.nih.gov/34650760/
- Habif, T. Clinical Dermatology: A Color Guide to Diagnosis and Therapy (6th Edition). 231 – 233 (Saunders, 2015). https://www.elsevier.com/books/clinical-dermatology/habif/978-0-323-26183-8