Common Medications That Cause Acne Include Corticosteroids, Anabolic-Androgenic Steroids (AAS), Lithium, Isoniazid, Halogens, and EGFR Inhibitors (EGFR-I)

The Essential Info
Can Definitely Cause Acne: Based on research, common medications that often result in acne include:
- Corticosteroids
- Testosterone and other anabolic-androgenic steroids (AAS)
- Lithium
- Isoniazid
- Halogens
- EGFR inhibitors (EGFR-I)
May Cause Acne: High doses of vitamin B supplements may also cause acne, particularly in females, but the evidence is incomplete.
Might Cause Acne: A few case reports point toward a possibility that the following medications might also cause acne:
- Rifampicin
- Ethosuximide
- Interferon
- Olanzapine
- Some hormonal contraceptives that release progesterone

The Science
- Medications That Can Definitely Cause Acne
- Medications That May Cause Acne
- Medications That Might Cause Acne
- Skip Down to Summary
Factors that Determine Whether Someone May Develop Drug-induced Acne
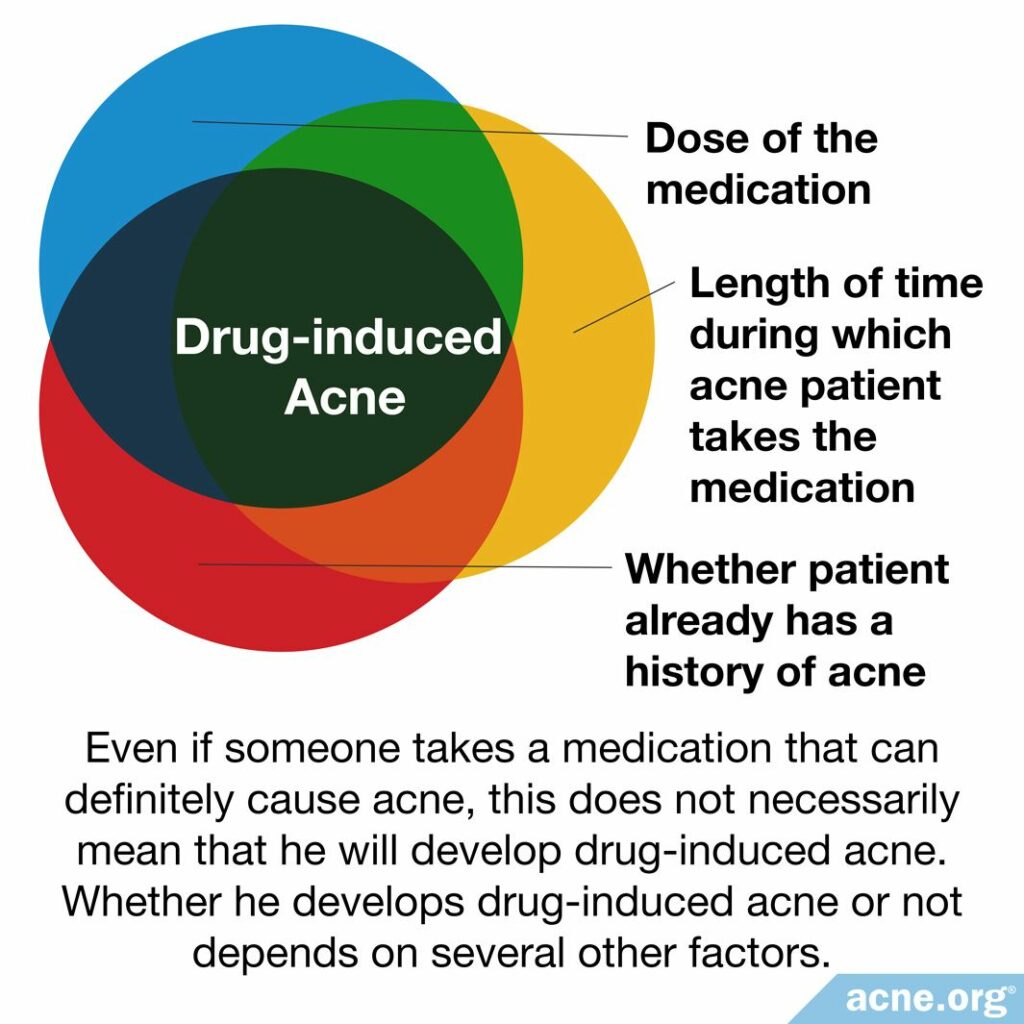
Whether someone develops drug-induced acne or not depends on several other factors, including:
- Dose of medication: If someone takes a smaller dose, he may not experience acne, but may develop acne if he takes a larger dose.
- Length of time: If someone takes the medication only a few times, he may not experience acne, but may develop acne if he takes it regularly for weeks or months.
- History of acne: If someone has experienced acne before, he may be more likely to develop drug-induced acne.1,2
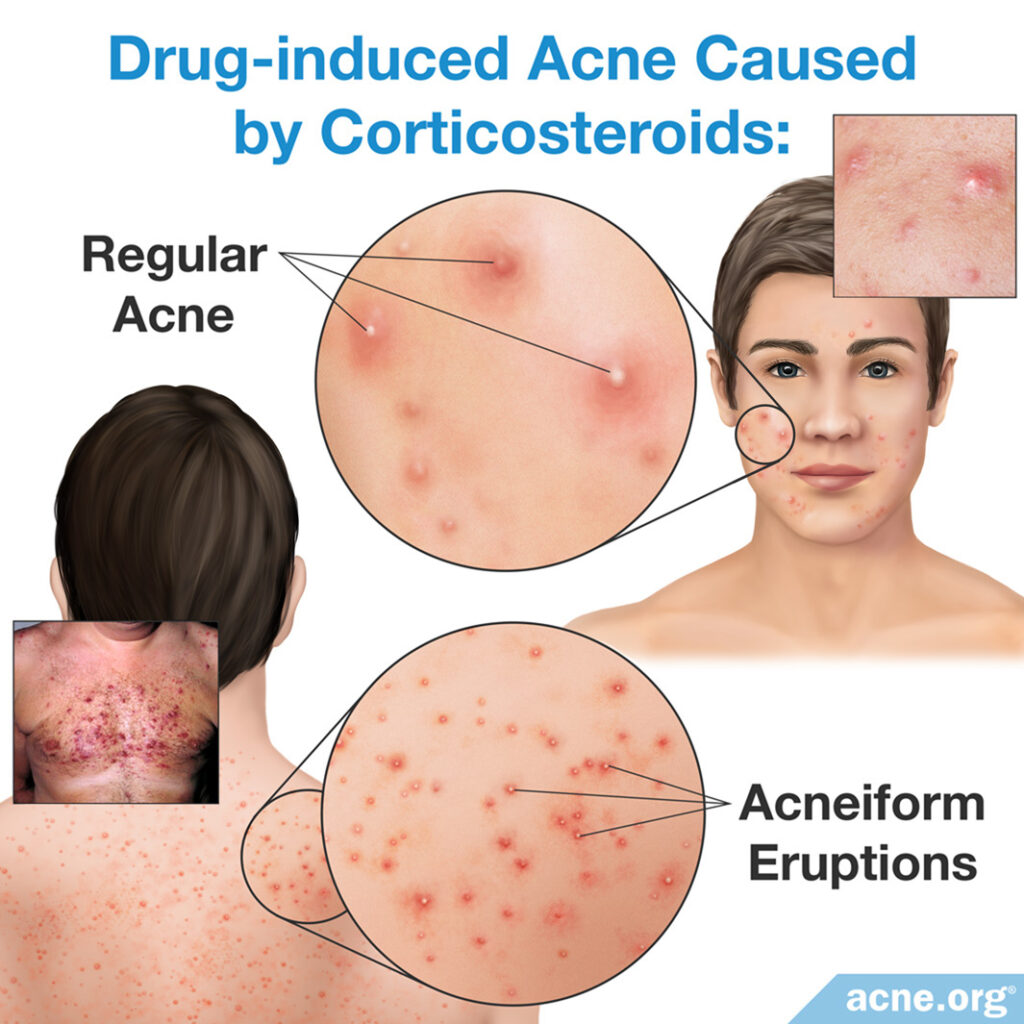
Regular Acne Vs. Drug-induced Acne
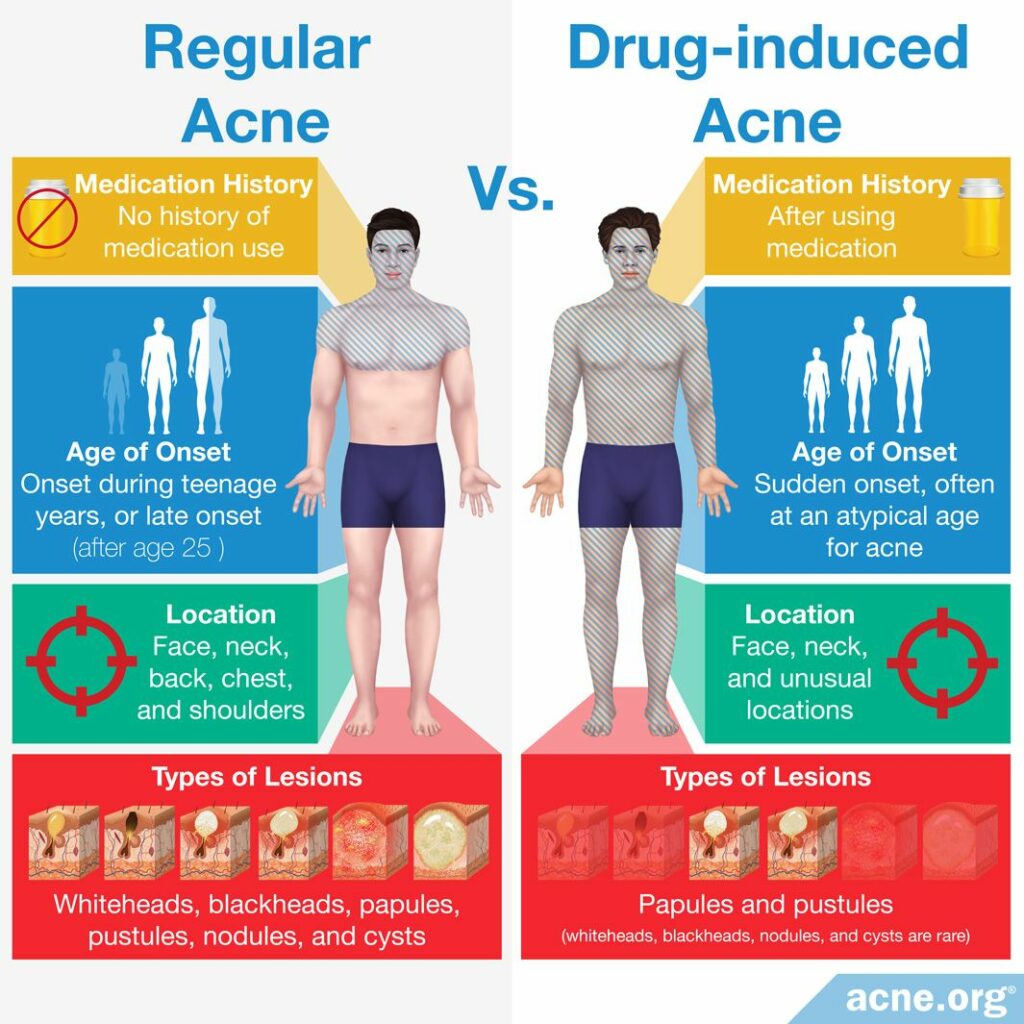
Regular acne is different from drug-induced acne (acne that is caused by medication) in four ways:
- Medication history: Regular acne can develop in a person who has not used any medication. In contrast, drug-induced acne only develops after he has used a medication that can cause acne.
- Age of onset: Regular acne is most common in adolescents (teens) and develops gradually, while drug-induced acne can occur at any age and often begins suddenly.1
- Location: Regular acne typically appears on the face, back, chest, and/or shoulders because the skin-oil-producing glands (sebaceous glands) located in these areas of the body tend to produce an abundance of skin oil (sebum). Medications that lead to drug-induced acne can also create acne lesions in these areas, but can also create acne lesions in unusual locations, such as the lower legs and the back of the arms.1
- Types of lesions: Regular acne usually produces many different types of lesions, including whiteheads, blackheads, papules, pustules, nodules, and cysts. Medications like AAS and lithium increase a person’s existing tendency to develop regular acne, so a person who takes these medications may experience all of these different types of lesions. In contrast, drug-induced acne typically produces only papules and pustules, which are reddened bumps on the skin that people commonly call “pimples” and “zits.” It is unusual for a person with drug-induced acne to develop whiteheads or blackheads, which are clogged pores that are not red.1 Because of these differences, drug-induced acne lesions are often called acneiform (pronounced acne-form), meaning “acne-like.”
Regular Acne Treatments Vs. Drug-induced Acne Treatments
A variety of treatments are available for regular acne. These treatments typically reduce acne symptoms slowly over weeks or months.
On the other hand, drug-induced acne does not respond well to regular acne treatments. It does, however, usually clear up gradually after the person stops using the offending medication.
In order to understand how some medications cause acne, it’s helpful to understand how acne develops. Open the drawer below for a quick crash course if you’d like:
Expand to read how acne develops
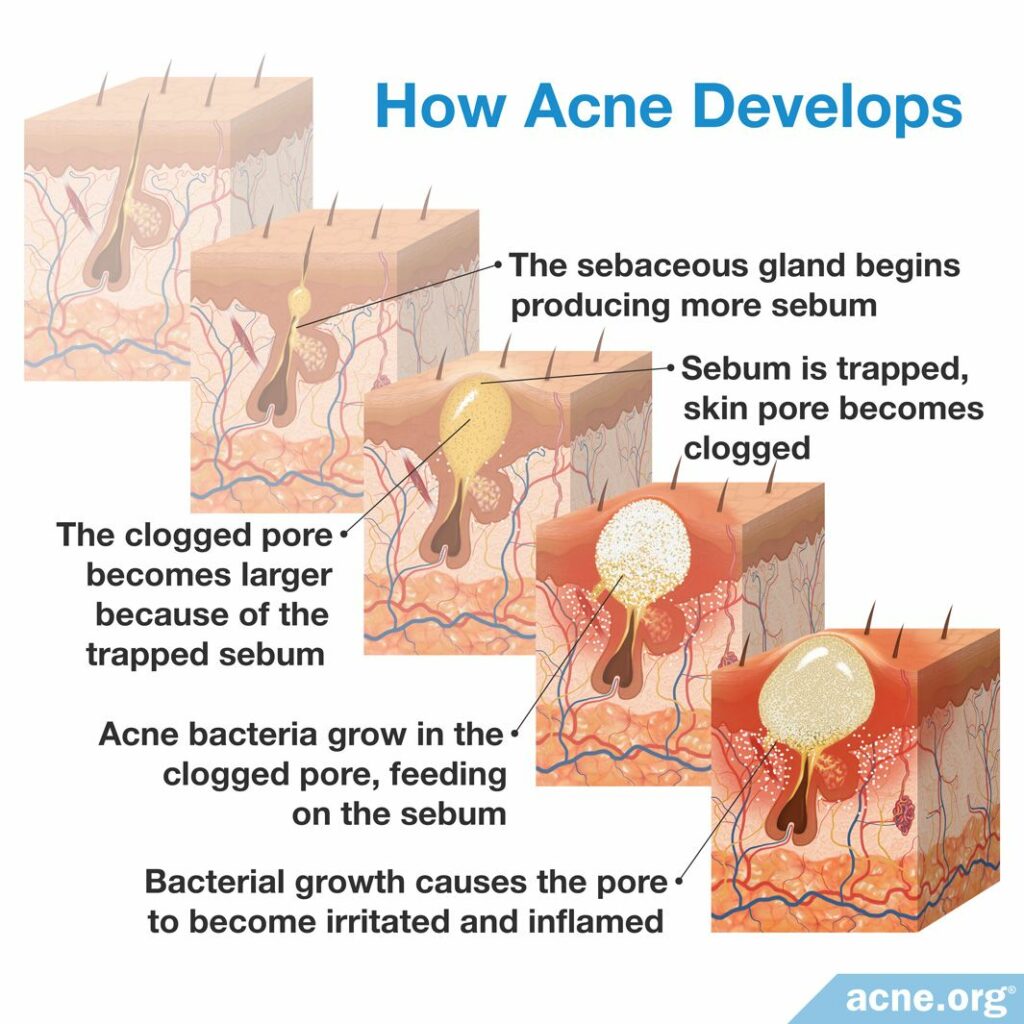
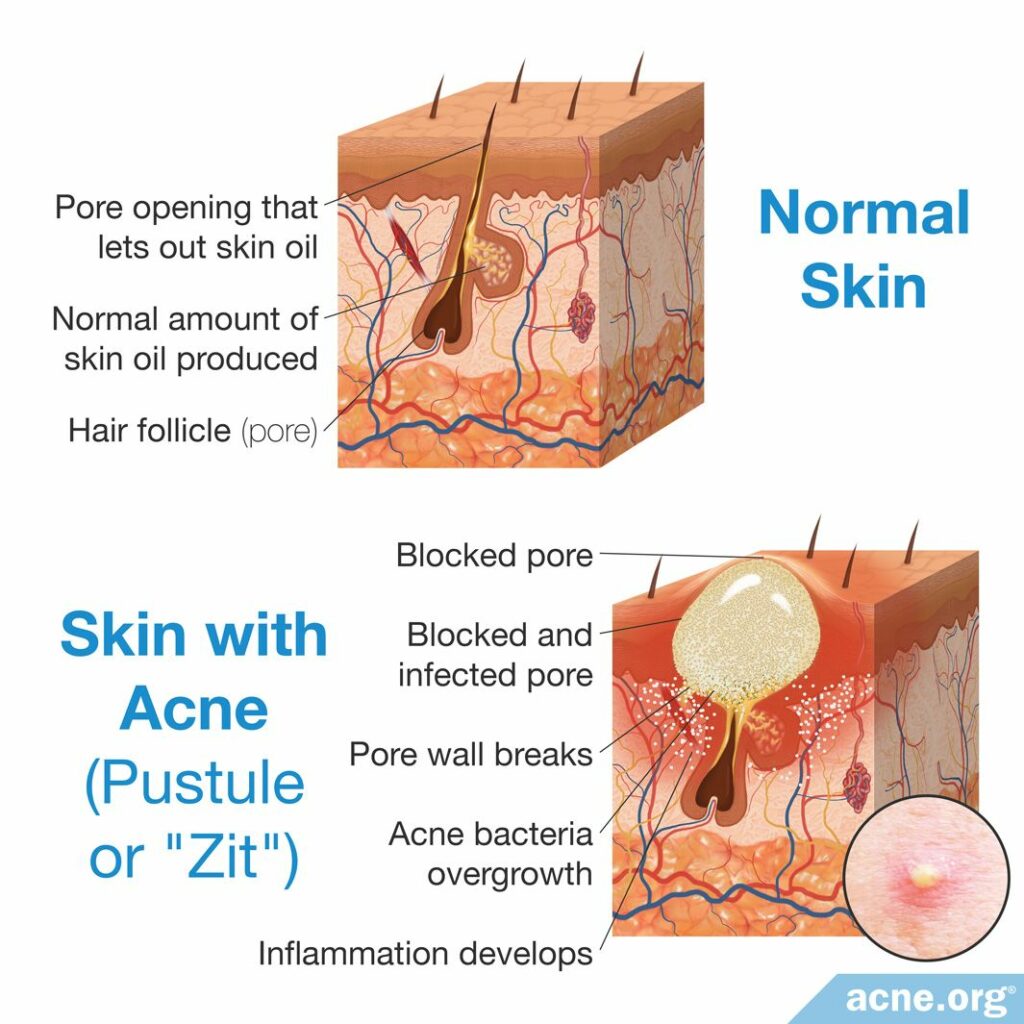
The skin oil glands (sebaceous glands) begin producing more skin oil (sebum). Skin pores become clogged, trapping the sebum inside. The clogged pores become larger because of the trapped sebum. Acne bacteria C. acnes begins to grow in the clogged pores, feeding on the sebum.
The bacterial growth causes the pores to become irritated and inflamed, meaning that the area becomes red, swollen, and sometimes sore.3
Drugs may also cause severe forms of acne. Expand the drawer below to learn more:
Expand to read about severe types of medication-induced acne
Sometimes medications can cause specific subtypes of severe acne, such as acne conglobata or acne fulminans.
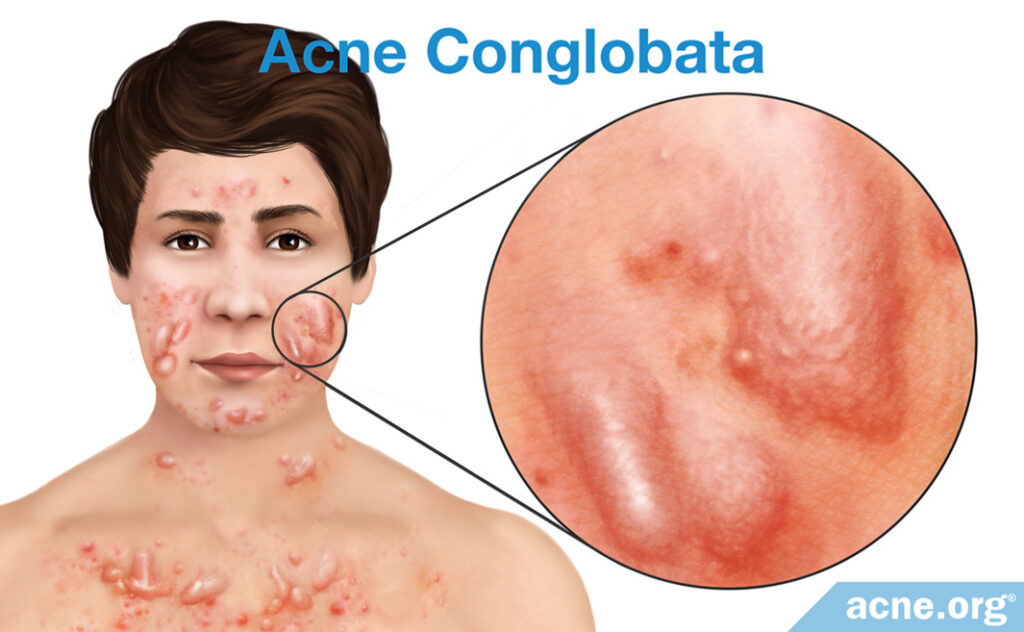
Acne conglobata: This is a rare and particularly severe form of nodulocystic acne, which is a type of acne in which people develop nodules (large, inflamed, painful, firm-to-the-touch lesions) and cysts (large, fluid-filled lesions). People with acne conglobata suffer from lesions on the body and face, and inevitably develop scarring, which can be particularly severe.4

Acne fulminans: This type of acne is as severe as acne conglobata, but cause additional systemic (bodily, as the result of medication transferred via the blood) symptoms – such as fever and joint pains.4
We can place potentially acne-causing medications into three categories, based on the amount of research that links them to acne:
- Medications that can definitely cause acne: A large amount of evidence links these medications to acne.
- Medications that may cause acne: A considerable but insufficient amount of evidence links these medications to acne.
- Medications that might cause acne: A small amount of evidence links these medications to acne.1
Let’s start by looking at the medications that can definitely cause acne.
Medications That Can Definitely Cause Acne
Corticosteroids
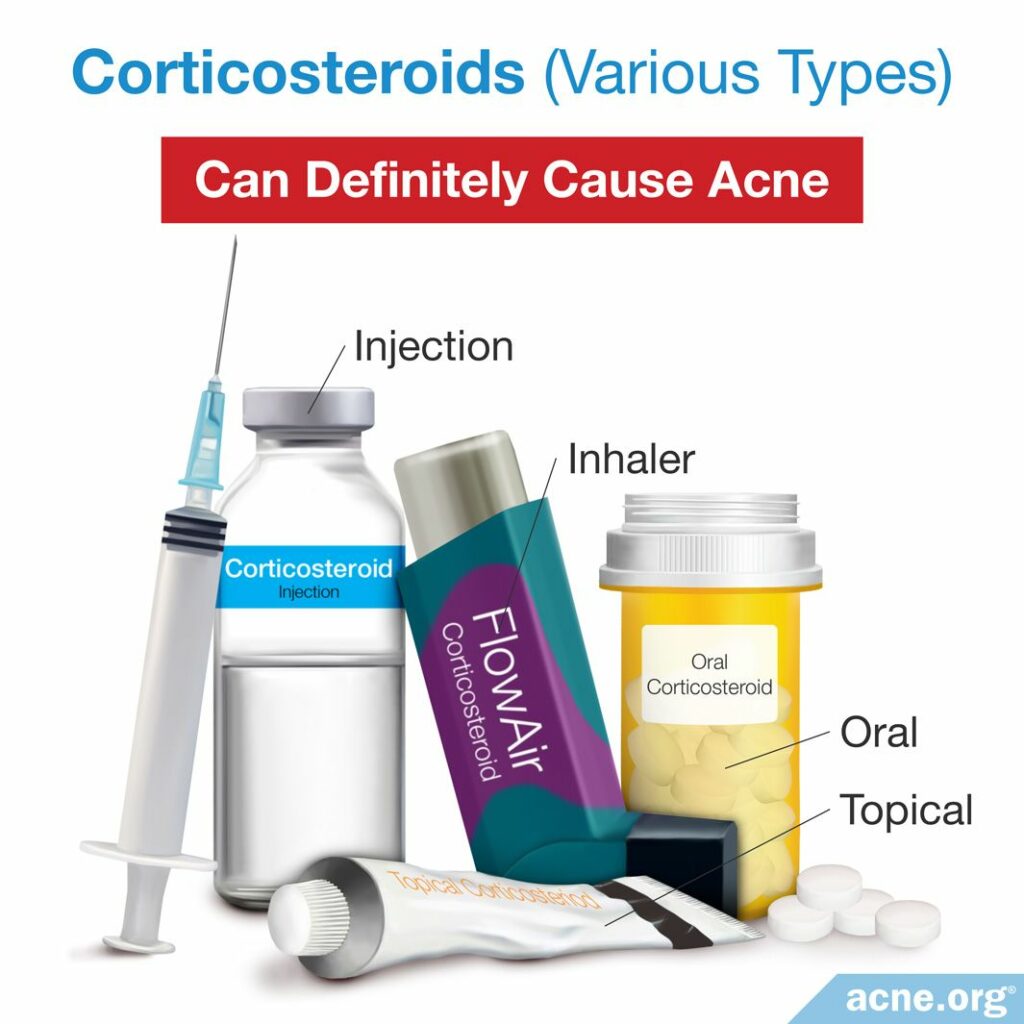
What They Are: Corticosteroids, not to be confused with anabolic steroids, which people take for bodybuilding, are medications that suppress the immune system. The immune system is the body’s natural defense mechanism against infection and disease.
Corticosteroids can be taken by mouth, inhaled, injected into a vein, or used as a topical cream or ointment on the face and other areas of the body. Using corticosteroids in high doses can result in so-called “steroid acne.”
A person who has a previous history of acne is more likely to develop steroid acne, and the severity depends on how long and at what dose the person uses the corticosteroids.2
The first symptoms of steroid acne are usually inflammatory (red) papules and pustules.4 Months later, these lesions gradually disappear, and whiteheads and blackheads (not red – so called “secondary comedones”) appear in their place. These are not the kind of comedones that develop in regular acne. Rather, these secondary comedones develop due to repeated damage to the pores from the previous papules and pustules.5
Note on asthma medication: In people who have asthma and inhale steroids using a mask, steroid acne may appear on the part of the face that the mask covers.1
How They Cause Acne: We do not know exactly how corticosteroids cause acne. Research suggests that they may increase the amount of skin oil (sebum) in skin pores, the same place where acne develops. This may be problematic because acne bacteria (C. acnes), which lives in skin pores, obtains its energy from sebum. When the amount of sebum in pores increases, the number of C. acnes also increases – which can lead to inflammation. This is when pimples form.4
Treatment of Steroid Acne: Steroid acne usually disappears gradually after patients stop using corticosteroids. However, sometimes they need to continue using them–for example, if they have asthma. In that case, their doctor may prescribe an acne treatment for ongoing prevention of acne.2
Anabolic-androgenic Steroids
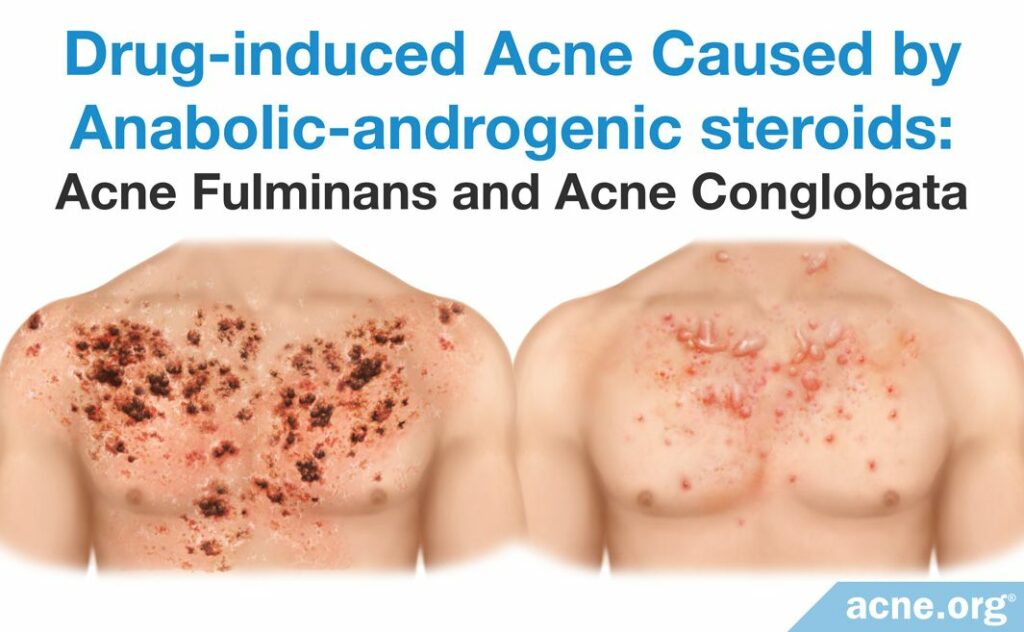
What They Are: Androgenic steroids are male sex hormones that are artificially synthesized in a laboratory. The structures of most AAS are similar to that of testosterone,7 a male sex hormone that is also found in females in small amounts.
The anabolic portion of “anabolic-androgenic steroids” means that these steroids can be used to increase muscle mass. Thus, AAS are the type of steroids that bodybuilders and athletes employ when looking to enhance their performance.
Doctors may prescribe AAS to treat muscle atrophy (wasting), and small doses can also treat hereditary angioedema (swelling of the deeper layers of the skin that runs in families). Doctors sometimes prescribe testosterone, which is an anabolic-androgenic steroid itself, to extremely tall boys to prevent further growth in height. A study that was published in 1992 in the journal Acta Dermato-Venereologica shows that about 1 – 2% of these boys develop acne fulminans.2
Doctors examined 176 Norwegian teen boys who received testosterone injections to stop growth in height. The researchers compared these boys to 23 boys who were untreated, and they found that those who received testosterone experienced a clear increase in acne one to eight weeks after the treatment. The acne lesions developed on the face and trunk (torso) and were severe in some of the boys – for example, there were four cases of acne fulminans.5
A main place that women produce testosterone is the ovaries, so doctors also occasionally prescribe testosterone treatment to women whose ovaries have been surgically removed. However, this therapy is controversial in women. Some studies report that testosterone replacement therapy causes acne in up to 38% of women, but other studies report numbers as low as 5%.2
How They Cause Acne: Male sex hormones increase the production of skin oil (sebum). When this occurs, the number of acne bacteria (C. acnes) also increases, potentially leading to the inflammation seen in acne pimples.
AAS can cause acne to erupt in both males and females. It can also make pre-existing acne worse in either sex, particularly in females. If a person who already has acne takes high doses of AAS, the skin oil glands in his/her skin may increase in size dramatically and begin producing more skin oil. He or she may also experience alopecia (hair loss) as a side effect of the medications. In addition, AAS can cause severe forms of acne.2
Treatment for Acne Caused by AAS: Once someone stops using AAS, acne may gradually disappear. However, in 30 – 60% of women who develop acne due to AAS, the acne does not clear up after ceasing use. In such cases, or for people who need to continue using AAS, doctors may prescribe the topical acne treatment.2
Lithium

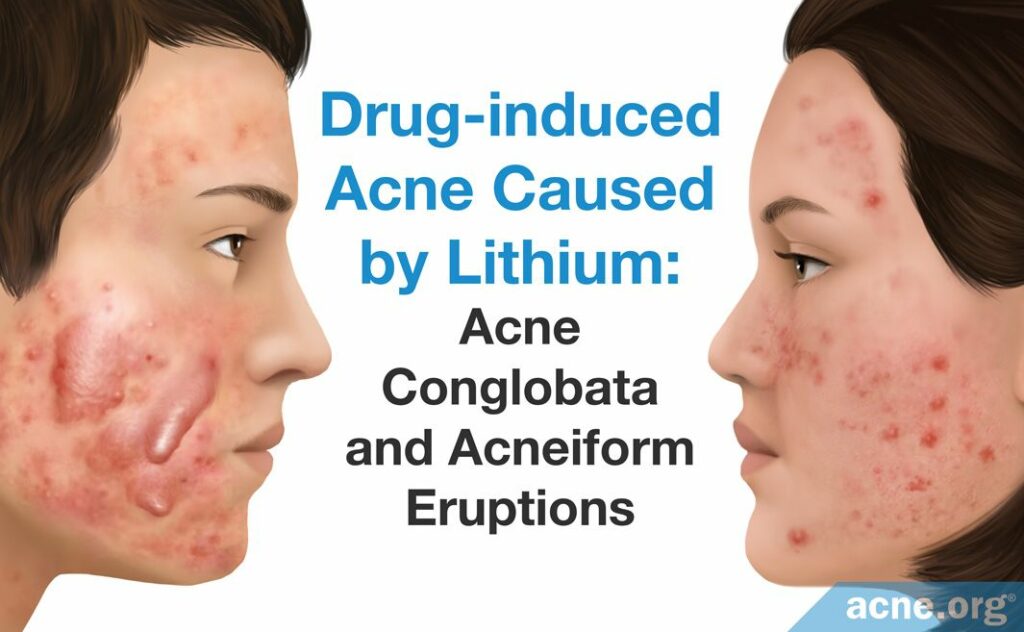
How It Causes Acne: In some people, even small doses of lithium can cause acne, but typically, people develop acne when large amounts of lithium build up in the body.
When lithium accumulates in the skin, it can damage skin cells. Damaged skin cells can clog skin pores, increasing the likelihood of acne to develop. Scientists also speculate that lithium may trigger inflammation in the skin. Since acne is primarily an inflammatory disease, this could be a reason why lithium lead to acne.2,5
Treatment of Acne Caused by Lithium: Stopping the use of lithium usually leads to a gradual clearing of the skin. A psychiatrist may also recommend replacing lithium with another mood stabilizer which does not cause acne. If lithium is determined to be the best treatment option for a person’s mood, using an acne therapy alongside lithium may help.
When it comes to acne due to lithium, a potential roadblock presents itself with the medication called isotretinoin, commonly known as Accutane®, which is approved to treat severe cases of acne. About 1% of people who take isotretinoin may experience depression as a side effect, which would defeat the purpose of taking lithium in the first place.1 Therefore, if you develop acne as a result of taking lithium, your doctor may hesitate to prescribe isotretinoin to you.
Tetracyclines, a class of oral antibiotics that can treat acne, are also not an option for treating acne caused by lithium, because the combination of tetracyclines and lithium can be toxic to the body.
Isoniazid


What It Is: Isoniazid is one of the main medications for the treatment of tuberculosis (a bacterial disease that affects the lungs). According to two large studies, approximately 1.4 – 2.5% of people who take isoniazid develop acne, usually after taking the drug over a long period of time.2
Taking it with other tuberculosis drugs may increase the chances of developing acne. One study of 2600 people found that among people who took isoniazid in combination with aminosalicylic acid, another tuberculosis medication, 16% developed acne.4
How It Causes Acne: We do not yet know how isoniazid causes acne. Research suggests that in some people, isoniazid tends to build up in the body, and these people may be more likely to develop acne due to it.
Treatment of Acne Caused by Isoniazid: In most cases, once someone stops taking isoniazid, her acne will gradually disappear.2
Halogens

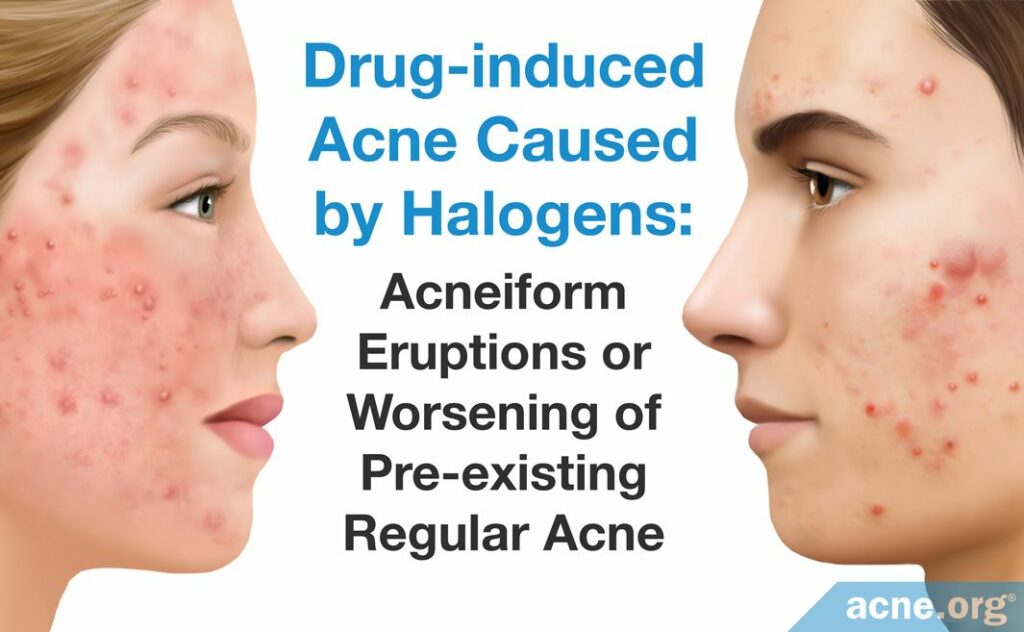
What They Are: Halogens are medications that contain the following chemicals: iodides, bromides, and/or chlorides. They are part of:
- Many asthma medications, such as potassium iodide (Quadrinal®) and (Theophylline Ki).
- Some expectorants (cough medicines), such as potassium iodide.
- Some vitamin supplements, such as supplements that contain kelp and many multivitamins.2
Bromides, specifically, are found in:
- Some sedatives, such as potassium bromide.
- Some cold remedies, such as the oral medication dextromethorphan hydrobromide (Bromfed DM®) and the nasal spray compound ipratropium bromide.2
- Some medications for treating ulcers, such as mepenzolate bromide.
- Some medications for treating the muscle disease myasthenia gravis, such as pyridostigmine bromide and neostigmine bromide.
Halogens often cause acne. Iodides and bromides are especially likely to cause acne or worsen existing acne, but iodides tend to cause more severe acne than bromides do.2 Acne due to halogens usually consists of comedo-like lesions and yellow cysts on the face.1
Iodine in food should not be an issue. There is no evidence that the small amount of iodine in salt or seaweed salad, for instance, will lead to acne.
How They Cause Acne: We currently do not know how halogens cause acne.
Treatment of Acne Caused by Halogens: Once a person stops using medications containing halogens, his acne should gradually disappear.
EGFR inhibitors

What They Are: Epidermal growth factor receptor (EGFR) inhibitors are a class of drugs for treating cancer, and they include cetuximab and erlotinib. As many as 85% of patients who take these drugs develop acne. More than 50% of people start to see acne after just one week of taking EGFR-I. Unlike regular acne, acne caused by EGFR-I can also appear on the lower legs and the back of the arms, and the breakouts typically are red and inflamed and do not include non-inflamed whiteheads or blackheads.2,3
How They Cause Acne: EGFR-I block the normal life cycle of skin cells, leading to clogging of skin pores. In addition, they speed up inflammation of the skin pores, so if acne has already started to form, these drugs will speed up the process.2
Treatment of Acne Caused by EGFR-I: Acne caused by EGFR-I, just like regular acne, can be treated with a variety of therapies. Treatment, however, is nonspecific. The lesions are known to respond to the regimens used in the standard treatment of acne, including commonly used anti-acne medications.8
Medications That May Cause Acne
Vitamin B Compounds

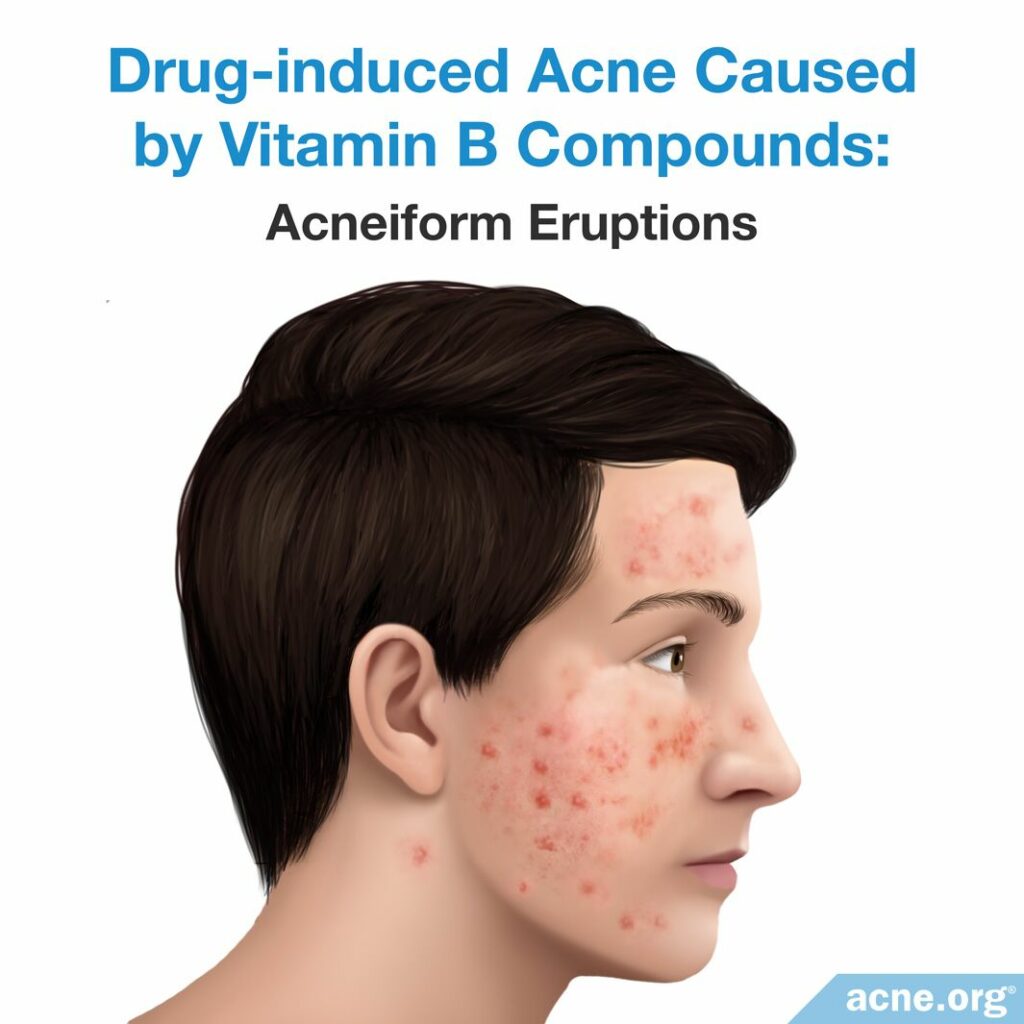
What They Are: Vitamin B compounds are vitamins that are sold as supplements. Vitamins B6 and B12 may cause acne, but almost all known cases of acne that are thought to be due to vitamin B compounds have occurred in women.2
Vitamin B12 may cause acne or worsen existing acne only at high doses, such as 5 – 10 milligrams per week. When it comes to vitamin B6, we do not know what dose may cause acne.2 On average, acne may appear about two weeks after a person begins using vitamin B compounds.1
How They May Cause Acne: We do not know how vitamin B compounds may cause acne. Some scientists have suggested that these vitamins may irritate the skin pores, causing inflammation.2
Treatment of Acne Caused by Vitamin B Compounds: Acne that may be caused by vitamin B compounds usually disappears gradually once supplementation stops.2
Medications That Might Cause Acne
Several common medications might cause acne, based on a small number of case reports. Because there is little research evidence linking these medications to acne, we do not know how they potentially cause acne or how the acne should be treated.
Hormonal Contraceptives That Release Progesterone
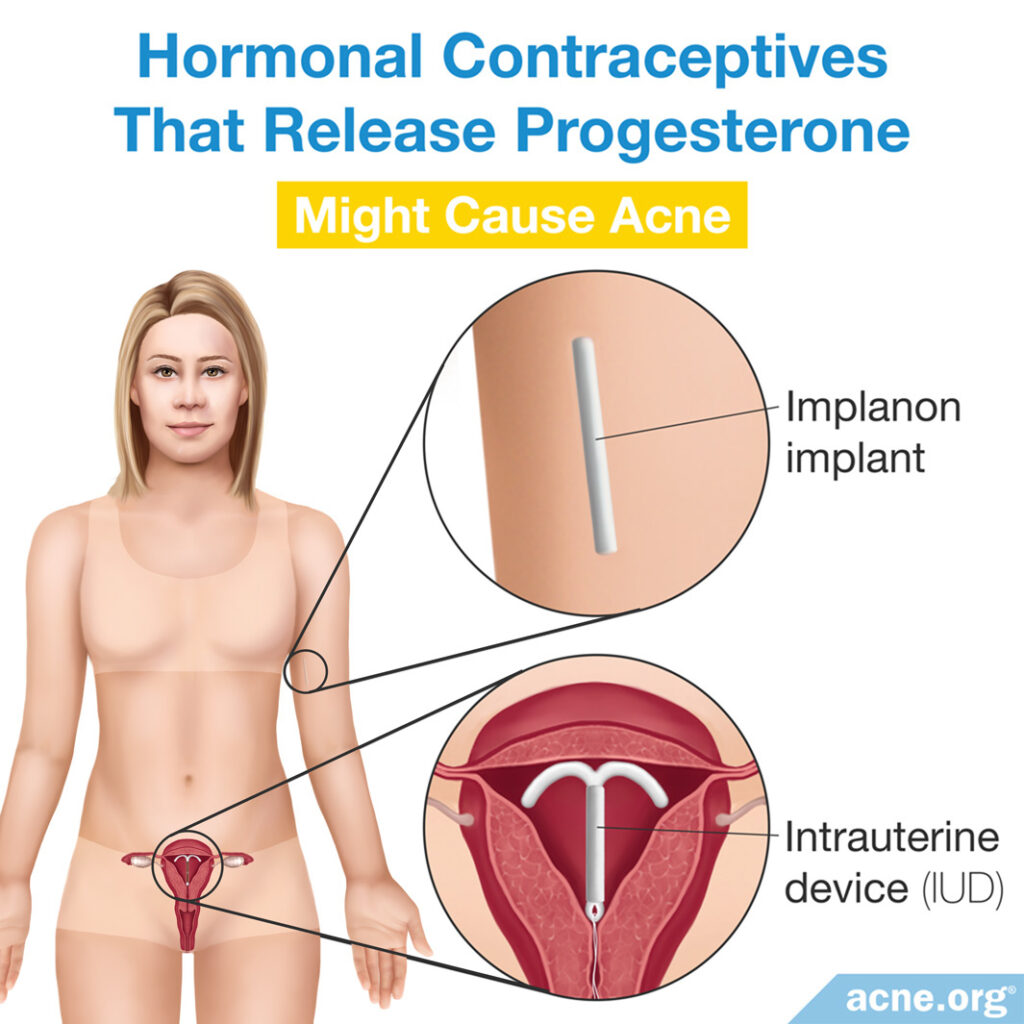
Oral contraceptives (birth control pills) containing female hormones help to clear up acne in females. These pills typically contain both estrogen and progesterone, the two main female sex hormones. However, some birth control devices that only contain progesterone might occasionally cause acne in some females. These devices include:
Intrauterine Devices (IUDs) That Release the Female Sex Hormone Progesterone: Some women develop acne 1 – 3 months after starting to use an IUD that releases hormones. In these cases, the acne might appear on the jaw and back and consists of papules (inflamed “pimples”).4,5
Implants, Such as Implanon®, Which Releases Progesterone: Up to 26.8% of women using Implanon® might develop acne, although not all studies agree on these numbers.5
Rifampicin


Rifampicin is a drug for treating tuberculosis, and doctors usually prescribe it in combination with isoniazid. Only one report, published in 1974, links rifampicin to acne:

The report describes a number of African patients who received rifampicin with another drug to treat tuberculosis, and developed acne on the face, shoulders, and back after five weeks. The authors found that the acne resolved after the patients stopped taking rifampicin, even though they continued to take the other medication.5
Ethosuximide

Ethosuximide is a medication for treating epilepsy (seizure disorder). Only one case report, published in the European Journal of Dermatology in 2017, links the drug to acne:

The report describes a 20-year-old Italian girl who had never had acne, but who developed acne after treatment with ethosuximide. The girl experienced papules and pustules on the chest, back, forehead, and neck that were intensely itchy.6
To treat the acne, the girl’s doctors reduced her ethosuximide dose and also prescribed an antihistamine (antiallergy) medication for the itching and a topical antibiotic. This treatment was effective, and the acne gradually disappeared.6
Interferon


Interferons are proteins the human body naturally produces as a defense against viruses. Doctors also sometimes prescribe interferons to help treat viral infections such as hepatitis or immune-system-related disorders like multiple sclerosis. There are at least 20 different types of interferons.
One case report, published in the Indian Dermatology Online Journal in 2016, links a type of interferon called interferon-alpha-2a to acne:

The report describes an 18-year-old girl with a history of occasional acne who developed a very severe form of acne called acne fulminans after treatment with interferon-alpha-2a for hepatitis B. The girl’s symptoms improved after she stopped interferon treatment and began to take a low dose of isotretinoin (Accutane®).9
Another case report, published in the Brazilian journal Anais Brasileiros de Dermatologia in 2011, links a different type called interferon-beta-1b to acne:

The report describes a 32-year-old Caucasian female with no previous history of acne who developed acne-like lesions due to treatment with interferon beta-1b for her multiple sclerosis. The acne-like lesions appeared on her face, neck, and arms. The lesions disappeared after she stopped treatment with interferon and completed a 4-week course of antibiotic treatment prescribed by her doctor.10
Olanzapine

Olanzapine is an antipsychotic drug used to treat conditions like schizophrenia. One case report, published in the Indian Journal of Psychological Medicine in 2019, links olanzapine to acne:

The report describes a 25-year-old woman who developed acne-like lesions on the face after starting treatment with olanzapine for her schizophrenia. The authors wrote, “There is no previous case report describing…acneiform [eruptions] with olanzapine exposure in schizophrenia.”11
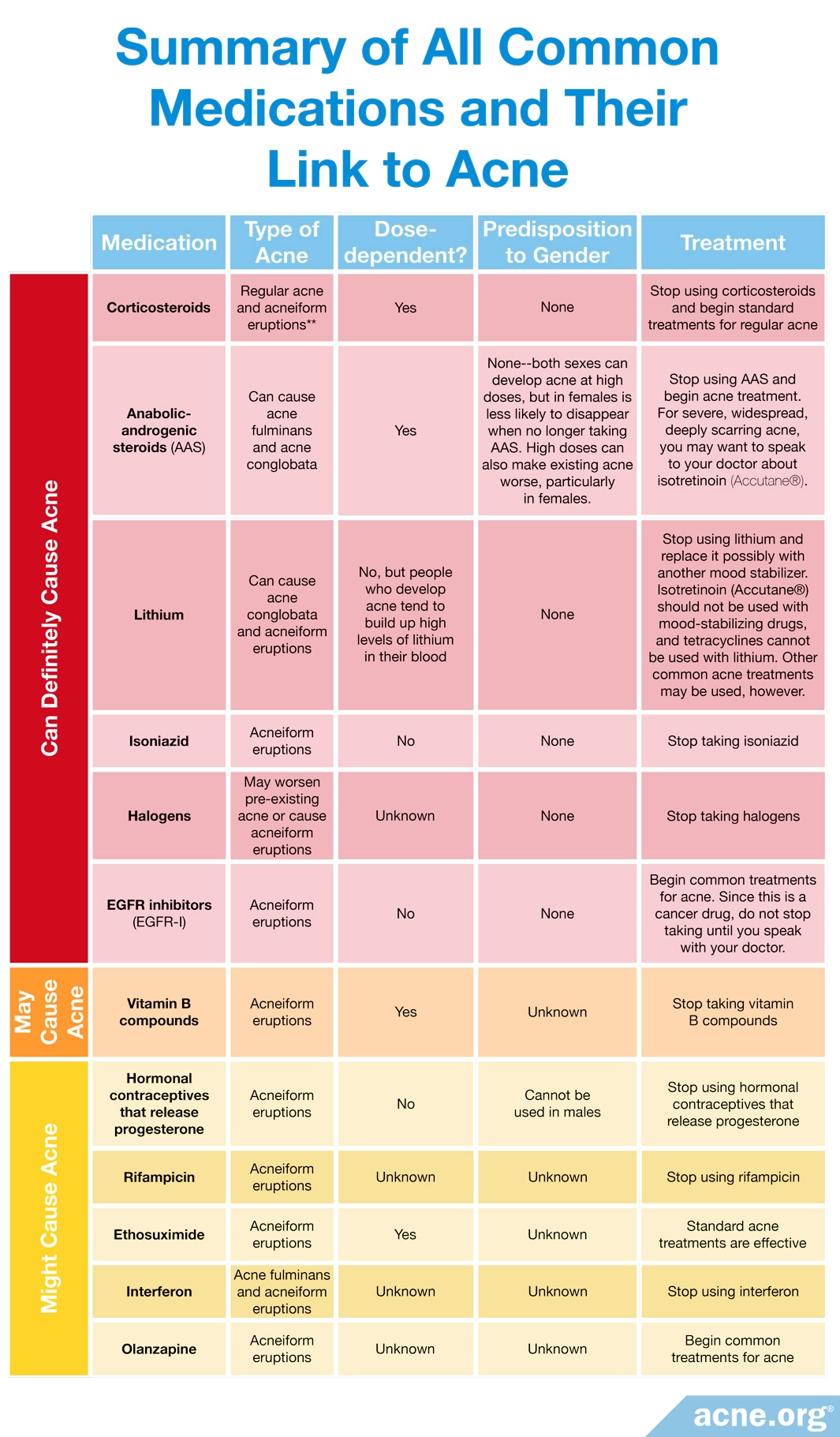
Summary
The table below summarizes all the common medications we have looked at and their link with acne:
Expand to read a full list of any other drugs mentioned in scientific literature

According to a 2020 article in StatPearls, an online educational publication for doctors, “Drug-induced acne…can occur due to…anticonvulsants like phenytoin, antidepressants, the antipsychotic olanzapine…antituberculosis drugs like INH, thiourea, thiouracil, disulfiram, corticotropin, antifungals like nystatin and itraconazole, hydroxychloroquine, naproxen, mercury, amineptine, chemotherapy drugs…Antibiotics like penicillins and macrolides…co-trimoxazole, doxycycline, ofloxacin, and chloramphenicol.”12

According to a 2013 article in the Brazilian journal Anais Brasileiros de Dermatologia, “Drug-induced acne, or drug-induced acneiform eruption, is an adverse effect of…thyroid hormones…antibiotics (tetracycline and streptomycin)…antiepileptic drugs (phenobarbital and hydantoin derivatives), cyclosporin A, antimycotics, gold salts, isotretinoin, clofazimine.”13

A 2009 article in the journal Archives of Dermatology stated, “Nodulocystic acne may be induced by the use of cyclosporine in children as well as adults.”14

A 2019 article in the journal Acta Biomedica stated, “Acneiform eruptions…occur with iodides, bromides, adrenocorticotropic hormone…actinomycin D, and phenytoin.”15

According to a 2022 case report in the Journal of Cutaneous Medicine and Surgery, isotretinoin, an oral medication prescribed to treat severe acne, actually caused a worsening of acne in one patient, leading the patient to develop a very rare and serious type of acne called acne fulminans. This type of acne comes with large, painful lesions that turn into blood-filled wounds. While acne fulminans typically includes full-body (systemic) symptoms like joint pain and fever, in this case, the patient had no systemic symptoms. The patient was a 16-year-old male, and acne fulminans developed 2 months after he started taking isotretinoin to treat his severe acne.16

Similarly, in 2020, the Dermatology Online Journal reported the case of a 13-year-old male who developed acne fulminans without systemic symptoms after taking isotretinoin for 30 days.17
A 2022 article published in the Journal of Cystic Fibrosis reported that 19 patients developed acne or experienced a worsening of acne after receiving their first dose of elexacaftor/tezacaftor/ivacaftor, a drug that helps patients with cystic fibrosis manage their symptoms.18
References
- Kazandjieva, J. & Tsankov, N. Drug-induced acne. Clin Dermatol 35, 156 – 162 (2017). https://www.ncbi.nlm.nih.gov/pubmed/28274352
- Zouboulis, C. Pathogenesis and Treatment of Acne and Rosacea. (Springer Berlin Heidelberg, 2014). https://www.springer.com/gp/book/9783540693741
- Cutaneous drug eruptions. 157 – 165 (Springer, 2015). https://link.springer.com/book/10.1007/978-1-4471-6729-7
- Zeichner, J. Acneiform eruptions in dermatology. (Springer Science+Business Media, 2014). https://www.springer.com/gp/book/9781461483434
- Du-Thanh, A., Kluger, N., Bensalleh, H. & Guillot, B. Drug-Induced Acneiform Eruption. Am J Clin Dermatol 12, 233 – 245 (2011). https://www.ncbi.nlm.nih.gov/pubmed/21668032
- Ricci, F., Paradisi, A. & Masini, F. Acneiform eruption induced by ethosuximide. EJD 24, 97 – 98 (2017). https://www.ncbi.nlm.nih.gov/pubmed/24334200
- Anabolic steroid, https://en.wikipedia.org/wiki/Anabolic_steroid
- DeWitt, C., Siroy, A. & Stone, S. Acneiform eruptions associated with epidermal growth factor receptor – targeted chemotherapy. J Am Acad Dermatol 56, 500 – 505 (2007). https://www.ncbi.nlm.nih.gov/pubmed/17166623
- Arora, S., Malik, A., Kumar, D. & Sodhi, N. Hepatitis B, interferon, and acne fulminans in a young girl. Indian Dermatol Online J 7, 93‐95 (2016). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4804601/
- Rosa, D. J., Matias Fde, A., Cedrim, S. D., Machado, R. F., Sá, A. A. & Silva, V. C. Acute acneiform eruption induced by interferon beta-1b during treatment for multiple sclerosis. An Bras Dermatol 86, 336‐338 (2011). https://www.scielo.br/scielo.php?script=sci_arttext&pid=S0365-05962011000200018
- Sutar, R. & Ganjekar, S. Dysmorphic delusion and olanzapine-induced postpartum dermatosis in a case of schizophrenia. Indian J Psychol Med 41, 393‐395 (2019). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6657489/
- Nair, P. A. & Salazar, F. J. Acneiform Eruptions. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2020. https://www.ncbi.nlm.nih.gov/books/NBK459207/
- Pontello, R. Jr & Kondo, R. N. Drug-induced acne and rose pearl: similarities. An Bras Dermatol 88, 1039‐1040 (2013). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3900370/
- Strahan, J. E. & Burch, J. M. Cyclosporine-induced infantile nodulocystic acne. Arch Dermatol 145, 797‐799 (2009). https://www.ncbi.nlm.nih.gov/pubmed/19620562
- Crisafulli, G., Franceschini, F., Caimmi, S., et al. Mild cutaneous reactions to drugs. Acta Biomed 90, 36‐43. (2019). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6502176/
- Yorulmaz, A. & Hayran, Y. Isotretinoin-induced acne fulminans. J Cutan Med Surg 26, 435-437 (2022). https://pubmed.ncbi.nlm.nih.gov/34498501/
- Fakih, A., Goens, J., Grozdev, I., Dangoisse, C. & Richert, B. Acne fulminans induced by a low dose isotretinoin: case report and review of the literature. Dermatol Online J 26, 1-8 (2020). https://pubmed.ncbi.nlm.nih.gov/33423422/
- Hudson, B. N., Jacobs, H. R., Philbrick, A., Zhou, X. A., Simonsen, M. M., Safirstein, J. A. & Rotolo, S. M. Drug-induced acne with elexacaftor/tezacaftor/ivacaftor in people with cystic fibrosis. J Cyst Fibros 21, 1066-1069 (2022). https://pubmed.ncbi.nlm.nih.gov/36088208/
 Acne.org Products
Acne.org Products