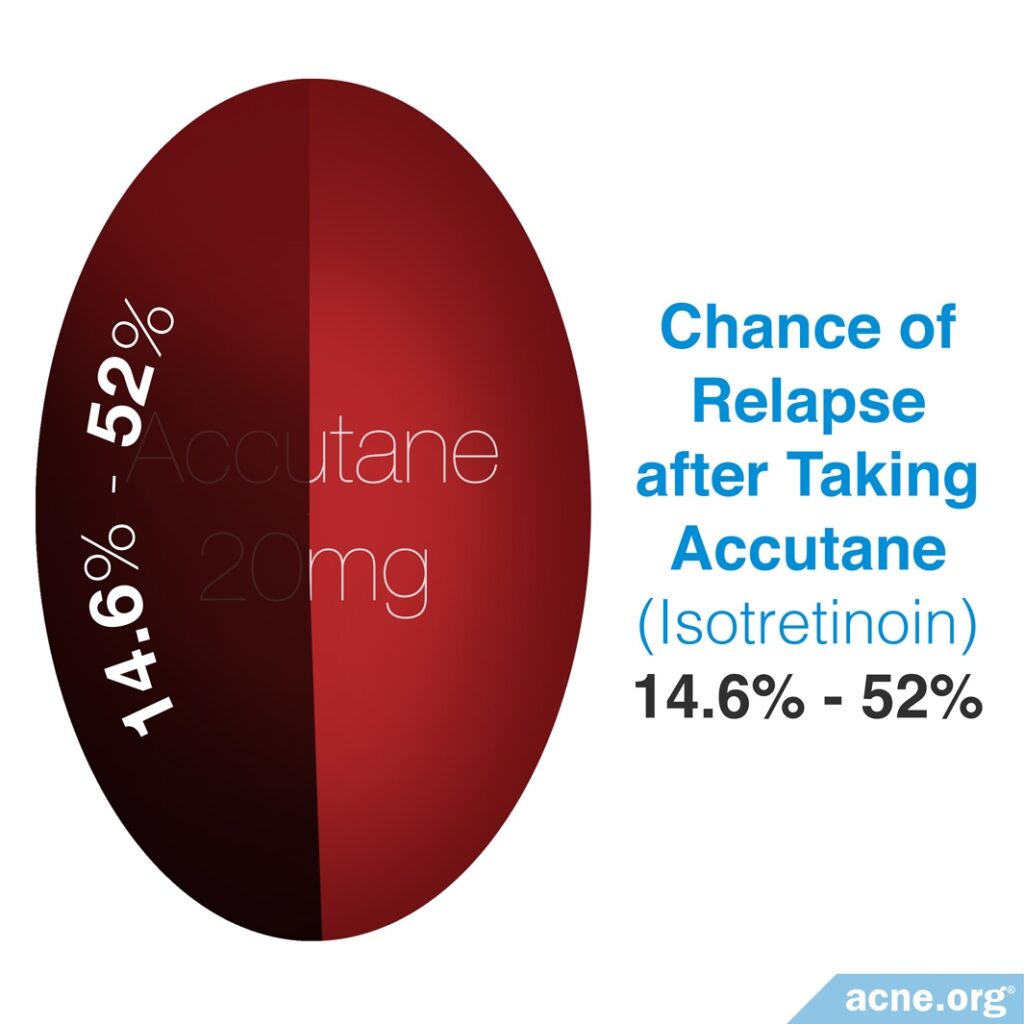
Isotretinoin Does Not Always Achieve a Long-term Result, and 14.6 – 52% of Patients Relapse

The Essential Info
Isotretinoin, often known by its original brand name, Accutane®, is an oral prescription medication that dermatologists sometimes prescribe to people with severe, scarring acne that does not respond to other treatments.
It is effective and can provide for long-term remission in some people. But for other people, it provides only temporary relief. Relapse rates following isotretinoin treatment vary between 14.6% to 52%, which is higher than scientists previously believed. Several factors increase the likelihood of an acne relapse:
- More severe acne
- Younger age
- Hormonal imbalance
- Stopping treatment early
- Male gender
- Not taking isotretinoin pills with fatty food
- Lower treatment dosage
Isotretinoin comes with numerous and sometimes severe and long-term side effects. Before considering it, do your research and be certain it’s the right course of action.
My Experience: I took isotretinoin in college for the usual 15-20 week course (I forget the exact amount of time). I went from having severe acne on my face and body to perfectly clear skin within a month or so. It was glorious. However, immediately following my isotretinoin course, I relapsed and started breaking out again, albeit not quite as badly. I experienced the same side effects as most people: severely dry lips, dry skin, and irritated eyes. I also experienced cumbersome joint pain. To this day I have to use lip balm several times a day and my joints have never quite gone back to normal. Take it from me, only consider isotretinoin if you really need it.

The Science
- Factors That Increase Relapse after Isotretinoin Treatment
- Do People Need Maintenance Therapy after Isotretinoin?
- The Bottom Line
Accutane (isotretinoin) is a highly effective acne treatment. This effectiveness has led many to believe that isotretinoin acts as a cure for even the most severe acne. Research, however, has shown that 14.6% to 52% of patients experience a relapse of acne after undergoing isotretinoin therapy.
When we look at 17 studies from 1989 through 2020 that look at acne relapse after isotretinoin, we can see this relapse range of 14.6 – 52%. The reason there is such a wide range is because of different study designs and definitions of exactly what “relapse” means. Some people may not report a relapse of their acne because their acne is improved compared to how it was before isotretinoin therapy, and therefore, they do not consider themselves to have “bad acne” like they did before they took isotretinoin, even though their acne did come back to a lesser degree.
Expand to read details of studies on relapse rate of isotretinoin

A 1993 study published in the journal Dermatology investigated 188 patients for acne relapse during 9 years following isotretinoin treatment. They found that 41% of patients relapsed after one treatment, 28% of patients relapsed after 2 or 3 courses of treatment, and 12% relapsed after several courses of treatment. Researchers observed relapse more often in patients with more severe acne and women with hormonal problems.1

A 2013 study published in Actas Dermo-Sifiliográficas examined the relapse rate of 142 patients with cystic acne during a two-year period following isotretinoin treatment. They found that 32% of males and 17% of females experienced a relapse. The authors attributed the gender difference of relapse to some female patients using oral contraceptives or anti-androgens, both of which reduce acne symptoms. The researchers showed that using oral contraceptives or anti-androgens reduced the chance of acne relapse by 3.5 times.2

A 2013 study published in Dermatology examined 13 previously performed studies that had treated patients with isotretinoin to identify the relapse rate. These studies found that 14.6% to 52% of patients treated with isotretinoin relapsed. The authors attributed the large range of relapse rates to an inconsistency in study design, as each study had a different definition of relapse, number of patients (32 – 17,351) and follow up period (1-5 years). Despite the inconsistencies, none of the studies included a maintenance therapy of other acne medications following isotretinoin therapy. Maintenance therapies can obscure the true relapse rate of Accutane because patients continuing with other acne therapies may prevent relapse. Therefore, the 14.6% to 52% rate that this study reported is the most accurate representation of the relapse rate after isotretinoin treatment.3
A 2020 study published in the Saudi Pharmaceutical Journal surveyed 427 Saudi patients who had taken isotretinoin. The average length of treatment with isotretinoin across all the patients was 7 months. The researchers found that 45.12% of the patients relapsed after taking isotretinoin. Contrary to what some other studies have found, in this study, patients who had been taking higher doses of isotretinoin were more likely to experience a relapse compared to patients who took lower doses. The study authors wrote, “Almost half of the patients showed relapse of acne after using isotretinoin.”4
Factors That Increase Relapse after Isotretinoin Treatment
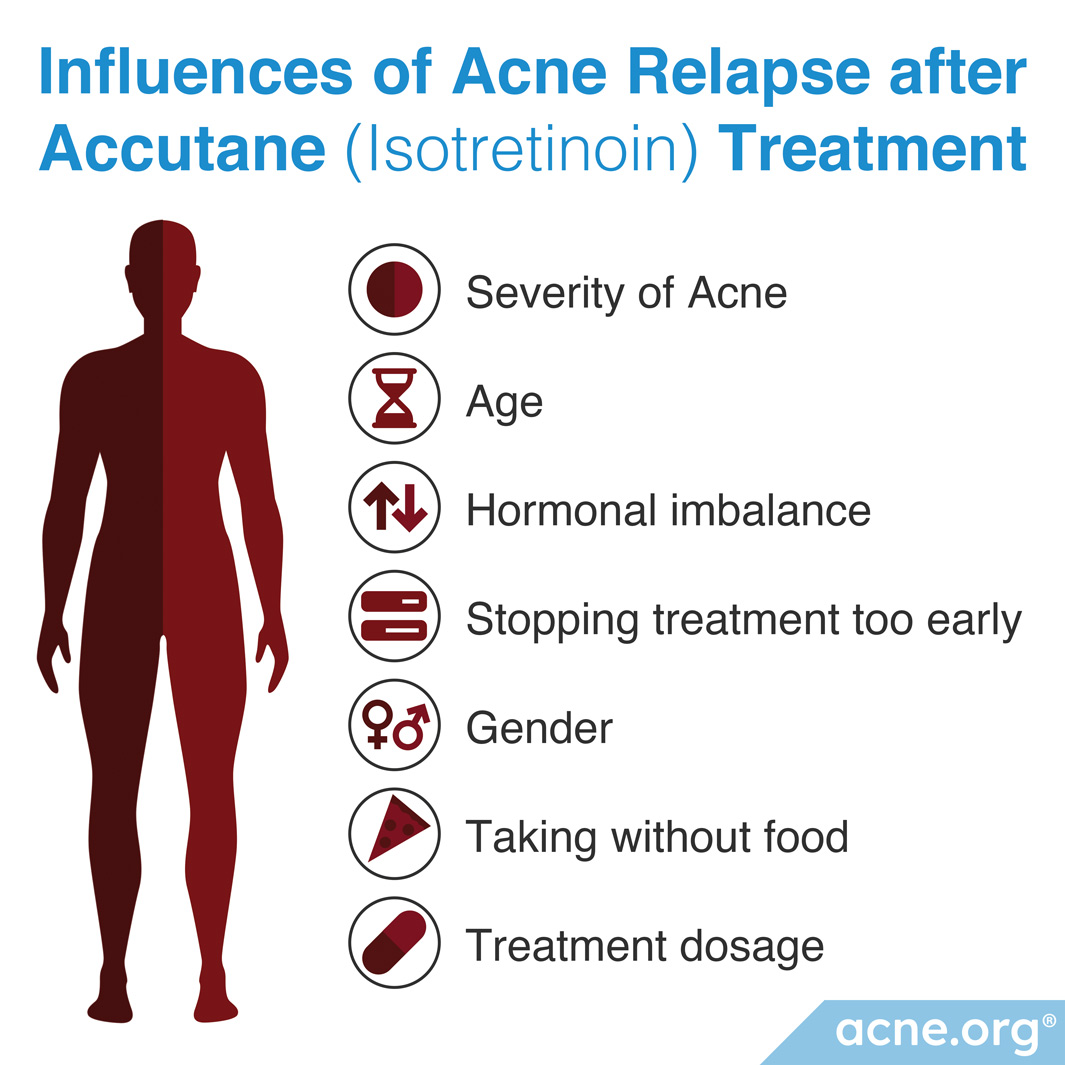
Several factors may increase the rate of relapse in patients treated with isotretinoin. These include:
- Severity of acne: People with more severe acne, and acne on the body, relapse more frequently
- Age: Younger patients experience acne relapse more frequently.
- Hormonal imbalances (especially in women): Women with hormonal imbalances relapse more often.
- Stopping before acne clears completely: People who stop taking isotretinoin before their acne completely clears also relapse more often.
- Gender: Males relapse more often than females.
- Taking isotretinoin without fatty food: Isotretinoin is much better absorbed when taken with an adequate amount of dietary fat. People who take isotretinoin without a meal that contains an adequate amount of fat may not absorb as much medication.
- Treatment dosage: People receiving lower dosages relapse more frequently.
Here are the studies that show us how these factors can increase the chances of relapse after isotretinoin treatment:
Expand to read details of studies on factors that increase chances of relapse

A 1993 study published in the British Journal of Dermatology studied 88 patients for relapse during a nine-year period following isotretinoin treatment. There were 27 patients who relapsed during the 9 years, with 96% of those relapses occurring during the first 3 years. The researchers also reported that patients who had back or chest acne, severe acne, and who took a lower isotretinoin dose relapsed more frequently. However, this study did not find a correlation between gender or age and relapse rates.5

A 2006 review published in Dermatology mentioned 2 studies that researched the relapse rate after isotretinoin therapy. They found that younger age, male gender, more severe acne, and hormonal imbalances (especially in women) were correlated with higher relapse rates. Of all patients studied, 29% to 39% of patients relapsed, with 12% never achieving clear skin even while using isotretinoin.6

A 2009 article published in Dermato-Endocrinology described the effectiveness of isotretinoin to treat acne. The authors stated that “males with extensive [body] acne, more severe acne, and/or suffering from acne for less than seven years fail to respond as well as and relapse more quickly that female patients with predominately facial acne of a less severe grade.” This means that males with more severe acne are more likely to relapse than females with less severe acne.7
A 2013 study published in the International Journal of Dermatology investigated the relapse of acne following isotretinoin treatment in 96 patients who either had, or did not have, polycystic ovary syndrome (PCOS). PCOS is a disease of the ovaries that leads to excess male hormones in women. The researchers found that out of the 24 patients who relapsed, 18 had PCOS. Therefore, they concluded that hormonal disorders, like PCOS, affect the relapse rate of isotretinoin.8

A 2012 article in the Australasian Journal of Dermatology listed factors that may increase the chances of relapse after taking isotretinoin. These include:
- Having severe acne
- Having macrocomedonal acne (acne characterized by very large whiteheads)
- Stopping isotretinoin before acne has fully cleared
- Smoking
- Having polycystic ovary syndrome (PCOS)
- Being younger than 14 or older than 25 years old9

A 2021 study published in Dermatologic Therapy came to similar conclusions. In this study, the acne relapse rate was 37.3%. The researchers found that the following factors made relapse more likely:
- Having macrocomedonal acne
- Stopping isotretinoin treatment before acne has fully cleared
- Being younger than 20 years old
The researchers wrote, “To prevent relapse in patients with acne using oral isotretinoin, it is of great importance to continue the treatment until complete clinical improvement, and extend the treatment for at least one more month regardless of the cumulative dose.”10

Another study published in the same journal in 2022, found that acne severity was the most important factor that predicted whether an acne relapse would occur after stopping isotretinoin treatment. In this study, 58% of patients with severe acne relapsed, compared to only 5.5% of patients with moderate acne. The researchers also found that patients younger than 20 years old were more likely to relapse.11

Finally, a 2023 study published in the Journal of Multidisciplinary Healthcare found that patients who stopped taking oral isotetinoin too early increased their chances of relapse nearly 4-fold. In this study, the relapse rate was 36%, with relapse occurring 6 to 18 months after stopping isotretinoin treatment.12
Studies that identified the factors of treatment dosage and taking isotretinoin with food with relapse
A collection of seven studies published in various journals between 1983 and 1998 found that increasing the dose of isotretinoin decreased the rate of acne relapse. However, each study compared different daily and cumulative doses of isotretinoin during the treatment. These dosage inconsistencies prevent researchers from comparing the studies to identify which dosage of isotretinoin is optimal to reduce acne relapse rates.13-19 More recent studies have run into a similar problem. However, most studies to date agree that taking a higher dose of isotretinoin and/or making sure to take isotretinoin with a high-fat meal helps to reduce the likelihood of acne relapse.
Expand to read details of recent studies on treatment dosage and relapse rate

A 2011 study published in the Journal of European Academy of Dermatology and Venereology studied 139 patients with mild-to-moderate acne. The researchers concluded that low dose isotretinoin treatments had similar relapse rates to high dose treatments during a two-year follow up period. However, as this study did not include patients with severe acne, these results do not apply to the typical isotretinoin patient.20

A 2013 study published in JAMA Dermatology studied 180 patients for relapse after isotretinoin treatment. They found that patients taking a lower dose of isotretinoin relapsed at nearly twice the rate of patients taking a higher dose. Despite the relapse, however, 97.4% of patients reported that their acne was improved following isotretinoin treatment. Therefore, even though many patients experienced a relapse of their acne, they perceived their returned acne to be less severe than before isotretinoin treatment.21

A 2012 article published in The Journal of Clinical and Aesthetic Dermatology spoke briefly about the importance of patients taking isotretinoin with food. The authors wrote that patients taking isotretinoin on an empty stomach will not properly absorb the full dose. Therefore, a patient who is not properly absorbing isotretinoin will not receive the proper dose, and that could potentially increase the chance of relapse.22

A 2019 study published in The Journal of Clinical and Aesthetic Dermatology looked at relapse rates in patients who took lidose-isotretinoin (Absorica®), a form of isotretinoin that may be taken without a high-fat meal. The researchers found that out of 166 patients who took lidose-isotretinoin without food daily for up to 20 weeks, only 17.5% relapsed and required follow-up acne treatment. The study authors wrote, “Long-term relapse rates for lidose-isotretinoin taken without food for 20 weeks were at the low end of those published for traditional isotretinoin taken with a high-fat/high-calorie meal.” However, it should be noted that even lidose-isotretinoin may not be absorbed well enough unless eaten with a high-fat meal.23
Do People Need Maintenance Therapy after Isotretinoin?
Often, dermatologists prescribe other acne medications as a maintenance therapy following isotretinoin treatment. Patients using a maintenance therapy may topically apply adapalene, benzoyl peroxide, retinoids, or combinations of these medications to keep acne at bay. However, this points to the reality that to stay clear of acne after isotretinoin, ongoing medication may be required.

A 2012 study published in Dermatology Research and Practice observed 20 male patients for acne relapse following isotretinoin treatment. The researchers found that men using a maintenance therapy had, on average, 38.7 less acne lesions than men who did not use a maintenance therapy.24

A 2013 study published in Dermatology studied 70 patients with moderate acne to determine if a maintenance therapy prevented relapse after isotretinoin treatment. This study found that only 2.94% of patients experienced an acne relapse if they used adapalene and benzoyl peroxide daily for one year following isotretinoin treatment. Although this study did not look past one year, it still reported much lower rates of relapse than previous studies lacking a maintenance therapy.3
The Bottom Line
Relapse after isotretinoin may be higher than people expect. While in many cases acne is permanently reduced, in 14.6 to 52% of people, acne will return to some degree, necessitating ongoing maintenance therapy with other treatments.
Since isotretinoin is such a serious medication that changes the skin and the rest of the body forever, and can come with lifelong side effects, it is vitally important that people with acne take all of these things into consideration before embarking on isotretinoin therapy.
References
- Lehucher-Ceyrac, D. & Weber-Buisset, M. J. Isotretinoin and acne in practice: a prospective analysis of 188 cases over 9 years. Dermatology. 186, 123-128 (1993). https://www.karger.com/Article/Abstract/247322
- Morales-Cardona, C. & Sánchez-Vanegas, G. Acne relapse rate and predictors of relapse following treatment with oral isotretinoin. Actas Dermosifiliograf. 104, 61-66 (2013). https://www.ncbi.nlm.nih.gov/pubmed/22795452
- Bettoli, V. et al. Maintenance therapy for acne vulgaris: efficacy of a 12-month treatment with adapalene-benzoyl peroxide after oral isotretinoin and a review of the literature. Dermatology. 227, 97-102 (2013). https://www.ncbi.nlm.nih.gov/pubmed/24029411
- Alshammari, Sa, Alamri, Y., Alanazi, Am., Almuhanna, Sa., Pinjabi, L. & Alsnaidi, Na. Prevalence and associated risk factors of acne relapse among Saudi acne vulgaris patients using isotretinoin. Saudi. Pharm. J. 28, 374‐379 (2020). https://www.ncbi.nlm.nih.gov/pubmed/32194340
- Layton, A. M., Knaggs, H., taylor, J. & Cunliffe, W. J. Isotretinoin for acne vulgaris-10 years later: a safe and successful treatment. Br. J. Dermatol. 129, 292-296 (1993). https://www.ncbi.nlm.nih.gov/pubmed/8286227
- Zouboulis, C. C. The truth behind this undeniable efficacy–recurrence rates and relapse risk factors of acne treatment with oral isotretinoin. Dermatology. 212, 99-100 (2006). https://www.ncbi.nlm.nih.gov/pubmed/16484812
- Layton, A. The use of isotretinoin in acne. Dermatoendocrinol. 1, 162-169 (2009). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2835909/
- Cakir, G. A., Erdogan, F. G. & Gurler, A. Isotretinoin treatment in nodulocystic acne with and without polycystic ovary syndrome: efficacy and determinants of relapse. Int. J. Dermatol. 52, 371-376 (2013). https://www.ncbi.nlm.nih.gov/pubmed/22998438
- Rademaker, M. Isotretinoin: dose, duration and relapse. What does 30 years of usage tell us? Australas. J. Dermatol. 54, 157‐162 (2013). https://pubmed.ncbi.nlm.nih.gov/23013115/
- Demirci Saadet, E. Investigation of relapse rate and factors affecting relapse after oral isotretinoin treatment in patients with acne vulgaris. Dermatol. Ther. 34, e15109 (2021). https://pubmed.ncbi.nlm.nih.gov/34431590/
- Kassem, B., Ismail, M. & Hassan, F. Evaluation of the efficacy and relapse rates of treatment protocols for moderate acne using isotretinoin based on the global acne grading system: Randomized, controlled, comparative study. Dermatol. Ther. 35, e15974 (2022). https://pubmed.ncbi.nlm.nih.gov/36346039/
- Ibrahim, S., Osman, B., Awaad, R. M. & Abdoon, I. Acne vulgaris relapse in Sudanese patients treated with oral isotretinoin: Rate and predictive factors. J. Multidiscip. Healthc. 16, 839-849 (2023). https://pubmed.ncbi.nlm.nih.gov/37020969/
- Jones, D. H., King, K., Miller, A. J. & Cunliffe, W. J. A dose-response study of I3-cis-retinoic acid in acne vulgaris. Br. J. Dermatol. 108, 333-343 (1983). https://www.ncbi.nlm.nih.gov/pubmed/6219690
- Strauss, J. S. et al. Isotretinoin therapy for acne: Results of a multicenter dose-response study. J. Am. Acad. Dermatol. 10, 490-496 (1984). https://www.ncbi.nlm.nih.gov/pubmed/6233335
- Wokalek, H., Hennes, R., Schell, Vogt H. J. A Review of Clinical and Laboratory Research. MTP Press Limited. 231-239 (1984).
- Cunliffe, W. J. & Norris, J. F. Isotretinoin–an explanation for its long-term benefit. Dermatologica. 175, 133-137 (1987). https://www.ncbi.nlm.nih.gov/pubmed/2446935
- Layton, A. M., Knaggs, H., Taylor, J. & Cunliffe, W. J. Isotretinoin for acne vulgaris–10 years later: a safe and successful treatment. Br. J. Dermatol. 129, 292-296 (1993). https://www.ncbi.nlm.nih.gov/pubmed/8286227
- Stainforth, J. M., layton, A. M., Taylor, J. & Cunliffe, W. J. Isotretinoin for the treatment of acne vulgaris: which factors may predict the need for more than one course? Br. J. Dermatol. 129, 297-301 (1993). https://www.ncbi.nlm.nih.gov/pubmed/8286228
- White, G. M., Chen, W., Yao, J., & Wolde-Tsadik, G. Recurrence rates after the first course of isotretinoin. Arch. Dermatology. 134, 376-378 (1998). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3970835/
- Borghi, A. et al. Low-cumulative dose isotretinoin treatment in mild-to-moderate acne: efficacy in achieving stable remission. J. Eur. Acad. Dermatol. Venereol. 25, 1094-1098 (2011). https://www.ncbi.nlm.nih.gov/pubmed/21198947
- Blasiak, R. C., Stamey, C. R. & Burkhart, C. N. High-dose isotretinoin treatment and the rate of retrial, relapse, and adverse effects in patients with acne vulgaris. JAMA Dermatol. 149, 1392-1398 (2013). https://pubmed.ncbi.nlm.nih.gov/24173086/
- Del Rosso, J. Q. Face to face with oral isotretinoin: a closer look at the spectrum of therapeutic outcomes and why some patients need repeated courses. J. Clin. Aesthet. Dermatol. 5, 17-24 (2012). https://www.ncbi.nlm.nih.gov/pubmed/23198008
- Del Rosso, J. Q., Stein Gold, L., Segal, J. & Zaenglein, A. L. An open-label, Phase IV study evaluating lidose-isotretinoin administered without food in patients with severe recalcitrant nodular acne: Low relapse rates observed over the 104-week post-treatment period. J. Clin. Aesthet. Dermatol. 12, 13‐18 (2019). https://www.ncbi.nlm.nih.gov/pubmed/32038751
- Vender, R. & Vender, R. Double-blinded, vehicle-controlled proof of concept study to investigate the recurrence of inflammatory and noninflammatory acne lesions using tretinoin gel (microsphere) 0.04% in male patients after oral isotretinoin use. Dermatol. Res. Pract. 2012, 736532 (2012). https://www.ncbi.nlm.nih.gov/pubmed/22577372
 Acne.org Products
Acne.org Products