Non-prescription Treatments Are Better for Mild and Moderate Cases of Seborrhea since Their Side Effects Are Less Severe

The Essential Info
Oily skin, known by its medical name, seborrhea, is a condition caused by an increase in the production of skin oil (sebum), leaving the skin feeling greasy, looking shiny, and the pores appearing enlarged.
Seborrhea on its own is not a disease, and if it does not accompany a disease such as acne, only non-prescription treatments are recommended.
However, increased sebum production tends to go hand in hand with acne. When oily skin is present and a person also has moderate-to-severe acne, prescription treatments are an option.
Prescription treatments (when moderate-to-severe acne is present): Prescription treatments can help significantly curb skin oil but can come with major side effects, so they are reserved for when oily skin comes with moderate-to-severe acne. They include:
- Isotretinoin – Accutane® (potentially lifelong side effects – approved only for severe, scarring acne)
- Hormonal treatments – antiandrogens and/or oral contraceptives
Non-prescription treatments (when no acne is present): Non-prescription treatments are safer than prescription treatments and come with less side effects. They include:
- Botox® injections (two studies show significant effectiveness)
- Topical green tea (may help a bit)
- Electrothermolysis (one study shows limited effectiveness)

The Science
- What Is Seborrhea (Oily Skin) And What Causes It?
- Prescription Treatments: Severe Cases of Seborrhea
- Nonprescription Treatments: Mild-to-moderate Cases of Seborrhea
- The Bottom Line
What Is Seborrhea (Oily Skin) And What Causes It?
The medical term for skin oil is sebum. When the skin overproduces sebum, the condition is called seborrhea. Seborrhea is characterized by:
- Shiny, greasy skin
- Enlarged skin pores
The primary cause of seborrhea is an increased amount of male hormones, called androgens, that are present in both males and females. However, there is some evidence pointing toward the possibility that lifestyle factors, such as excess sugar intake or high calorie consumption, may also increase skin oil production.1
Seborrhea is not a disease, and mild-to-moderate cases are normally treated only with non-prescription treatments.
Severe cases of seborrhea that are tied to underlying diseases, such as moderate-to-severe acne, are sometimes treated with prescription medications. Let’s start by looking at these prescription treatments for severe cases of seborrhea, and then we will look at non-prescription treatments for mild-to-moderate cases.
Prescription Treatments: Severe Cases of Seborrhea (And When Acne Is Present)
Doctors will normally only prescribe medications to people who suffer from oily skin when it accompanies an underlying disease, such as moderate-to-severe acne.
People with oily skin are also more likely to suffer from acne, so some prescription acne treatments may be useful in the treatment of seborrhea. There are two main prescription treatments for acne that can also be used to treat oily skin:
- Isotretinoin (males & females) – only approved for severe cases of acne – comes with severe side effects
- Hormonal therapies (females only)
Isotretinoin

Isotretinoin, often known by its original brand name, Accutane®, is an oral medication that doctors prescribe for people with severe acne. Isotretinoin is a powerful prescription medication that dramatically suppresses the production of sebum and reduces seborrhea. However, isotretinoin causes severe side effects and is the number one birth defect-causing medication on the market and should never be entered into lightly.
Isotretinoin is extremely effective in reducing seborrhea. Two clinical studies found that even low doses of isotretinoin can significantly reduce facial oiliness.
The first study, published in the Journal der Deutschen Dermatologischen Gesellschaft in 2003, found that even low doses of isotretinoin cut the size of skin oil glands in half.

The researchers performed this study by providing 11 patients with various amounts of isotretinoin daily for six months and then monitoring sebum production during that time period. They concluded that even the lowest dosage of isotretinoin (2.5mg three times per week) resulted in a decrease in sebum production, skin lesions, and size of skin oil glands. In fact, isotretinoin caused the average size of skin oil glands to reduce by approximately 50%. Although this study was performed on a small number of patients, it proved that even low doses of isotretinoin can be effective in the treatment of seborrhea.2,3
The second study, published in the International Journal of Dermatology in 2017, reported that low doses of isotretinoin taken over several months can significantly reduce skin oiliness in patients with moderate-to-severe seborrhea.

In this clinical study, 28 patients took 10 mg of isotretinoin every other day for 6 months. During that time period, the researchers kept track of the patients’ sebum production. They saw significant improvement in the patients’ skin oil levels after 3 months of treatment. The researchers reported that sebum production decreased, leaving the skin looking less shiny and feeling less greasy. They wrote, “This finding corroborates the efficacy of isotretinoin in the treatment of seborrhea.”4
Hormonal therapies
Since androgens (male hormones present in both males and females) are the main driver of skin oil production, hormonal treatments that suppress androgen production can reduce sebum production, and thus, seborrhea.
Although hormonal treatments help with seborrhea, they are recommended only to women because hormonal therapies usually cause men to develop feminine characteristics like enlarged breasts.5,6
And like all prescription treatments, hormonal therapies are reserved for people who are experiencing an underlying disease, such as acne. There are two basic types of hormonal therapies:
- Antiandrogens – block androgen function
- Inhibitors of androgen synthesis – block production of androgens
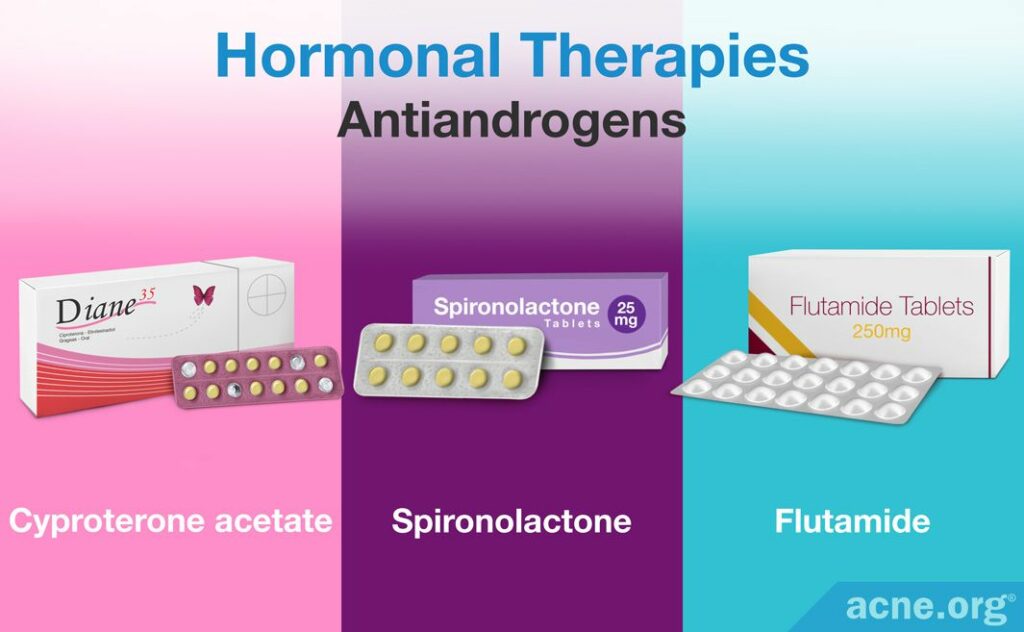
Antiandrogens
Antiandrogens are compounds that block androgens from acting as they normally would in the body, which then causes a reduction in sebum production. There are several approved oral prescription antiandrogens, including:
- Spironolactone: Doctors prescribe spironolactone in dosages of 50 – 100mg, taken twice daily. Side effects of spironolactone include breast tenderness and menstrual irregularities, among others.
- Cyproterone acetate (CPA): Doctors usually prescribe CPA at a 2 – 100mg daily dosage and combine it with an oral contraceptive (a birth control pill), most famously known by the brand names Diane-35® or Dianette®. Side effects of CPA include nausea, vomiting, fluid retention, swelling of the legs, headache, tiredness, liver dysfunction, shortness of breath, and blood clotting disorders, among others.
- Flutamide: Doctors prescribe it at 250mg twice daily. However, flutamide comes with serious side effects, including liver damage, which limits its use.5
Inhibitors of androgen synthesis: Oral contraceptives, glucocorticoids, and gonadotropins

In women, androgens are produced in the ovaries and the adrenal glands (a gland right above the kidneys). Three treatments that can be used to block androgen production in these places, and therefore reduce sebum production, include:6
- Oral contraceptives (OCs): Oral contraceptives, often known as birth control pills, are used to suppress ovulation and to treat moderate acne, and can also reduce sebum production. They contain two types of hormones, (1) estrogen and (2) progestin. Estrogen in particular can inhibit the production of androgen in the ovaries, which then causes a reduction in sebum production. Research shows us that most OCs work equally well when it comes to acne and sebum reduction. However, they come with potentially serious side effects and concerns and the decision to take them should be discussed with a knowledgeable and trusted physician.
- Glucocorticoids: Glucocorticoids are steroid hormones that can suppress androgen synthesis within the adrenal glands. The two most common steroids used for sebum suppression include prednisone at a 2.5 – 5 mg daily dosage and dexamethasone at a 0.25 – 0.75 mg daily dosage. Glucocorticoids can cause adverse side effects like increased bone loss, delayed wound healing, muscle weakness, and increased risks of infection. Because glucocorticoids are steroids, they are inadvisable to take in the long term, and are normally only prescribed for short periods of time in cases of extremely severe acne.
- Gonadotropins: Gonadotropins such as buserelin, nafarelin, and leuprolide, work to block ovulation and prevent androgen production in the ovaries. Although these hormones are effective in the treatment of acne through the reduction of androgens, they also decrease the production of estrogens. As estrogens possess a natural ability to suppress sebum production, gonadotropins may not be the best treatment for oily skin. They also come with side effects that include limiting the ovarian function of patients, which could lead to early menopausal symptoms. Because of these severe side effects, long-term usage of these hormones is not recommended.
Non-prescription Treatments: Mild-to-moderate Cases of Seborrhea

For people who do not have an underlying disease such as acne, but who are bothered by overly oily skin, non-prescription treatments are available, most notably:
- Botulinum toxin (Botox®) injections
- Topical green tea
- Electrothermolysis
Topical green tea
Two studies have shown that daily application of topical green tea may help reduce seborrhea to some degree. Many topical over-the-counter products contain green tea extract (EGCG), but just because a product says it has green tea or EGCG in it doesn’t mean it will work. More often than not, green tea is included in products simply for “label claim,” which means it is added to the product at an extremely small amount just so the manufacturer can list it on the label. Be sure to go with a reputable brand that educates the consumer about what percentage of green tea is in the product. At least one study has shown 3% green tea extract to be effective, so it may be best to look for a product with at least 3% green tea extract.
The following two studies have shown that topical green tea can help decrease sebum to a measurable degree.

A 2010 study published in the Bosnian Journal of Basic Medical Science found that a 3% green tea extract decreased sebum production to a measurable degree. Researchers performed this study by topically applying a three percent green tea extract to the cheeks of 16 healthy volunteers daily for eight weeks. They found that green tea extract decreased sebum production by blocking the formation of DHT.7

A separate 1995 study published in the journal of Biochemical and Biophysical Research Communications also found that green tea extracts suppress sebum production by inhibiting the synthesis of a male hormone called DHT. They found that the green tea compound responsible for blocking DHT synthesis is called epigallocatechin-3 gallate (EGCG).8
Botox injections
Scientific evidence is accumulating to show that Botox® injections can reduce skin oil production and skin pore size.9 It all started with a 2013 study showing that Botox® injections dramatically reduced skin oil production for 3 months or more.

A 2013 study published in the journal Dermatologic Surgery investigated the effect of botulinum toxin, which is used for Botox® injections, on sebum production. Botulinum toxin works by interacting with and blocking nerve impulses from nerve cells. These nerve impulses normally signal the cells within the sebaceous glands to produce sebum, so the researchers wanted to see if blocking these nerve impulses with botulinum toxin would result in decreased sebum production. To perform this study, botulinum toxin was injected 10 times in a linear arrangement across the foreheads of 25 patients with oily skin.
Before and after the injections the researchers measured facial sebum levels. One week following the injections, sebum production had decreased by 75%. One month after the treatment was an 80% decrease in sebum production. Even three months following the injections the production of sebum was 59% lower than before the treatment. Therefore, the researchers concluded that botulinum toxin injections may be a promising new treatment for oily skin.10
More recently, scientists have tested so-called Microbotox injections, which are injections of tiny amounts of botulinum toxin, and found that these were also effective at reducing seborrhea symptoms for several months after treatment.
Another study published in the Journal of Cosmetic Dermatology in 2022 tested Microbotox injections on 20 patients with seborrhea and enlarged skin pores. The researchers examined the patients’ skin 1 month and 4 months after the injections and found both skin oiliness and skin pore size to be reduced. Interestingly, the scientists also tested applying Microbotox to the skin surface by microneedles instead of injecting it into the skin. However, they found that injecting Microbotox into the skin produced better and longer-lasting results.11
Electrothermolysis
Electrothermolysis is a procedure that involves inserting a long, thin needle into the skin pore and zapping a small electric current into the pore repeatedly. It requires hundreds of needle injections and must be repeated multiple times over a series of months. The purpose of electrothermolysis is to damage the skin oil glands and therefore reduce sebum production. One study showed that it produced a 31.5% reduction in sebum after 4 treatments.

A 2007 study published in the journal of Dermatologic Surgery examined the effect of electrothermolysis on sebum production in 15 women over the course of six months. After the women received four treatment sessions of electrothermolysis at one- or two-month intervals, the researchers found that sebum production had decreased by 31.5%.12
The Bottom Line
If you have oily, shiny skin but no acne, you can try non-prescription treatments to cut down on the excess skin oil. Non-prescription treatments tend to cause fewer side effects but may have limited effectiveness.
However, if your oily skin also comes with moderate-to-severe acne, prescription treatments might be worth considering. While generally more effective, prescription treatments can cause potentially serious side effects and may only be warranted in cases of severe seborrhea with acne. This is especially true of isotretinoin (Accutane).
Going forward we may see new treatments emerge. Researchers are currently investigating new potential treatments for oily skin that show promise in lab experiments.13,14 If these treatments prove effective in clinical trials and pass safety tests, they may become available to people with seborrhea in the future.
References
- Makrantonaki, E., Ganceviciene, R. & Zouboulis, C. C. An update on the role of the sebaceous gland in the pathogenesis of acne. Dermatoendocrinol 3, 41 – 49 (2011). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3051853/
- Geissler, S. E., Michelsen, S. & Plewig, G. Very low dose of isotretinoin is effective in controlling seborrhea. J Dtsch Dermatol Ges 19, 952 – 958 (2003). https://www.ncbi.nlm.nih.gov/pubmed/16285647
- Zouboulis, C. C. Retinoids – Which Dermatological Indications Will Benefit in the Near Future? Skin Pharmacol Appl Skin Physiol 14, 303 – 315 (2001). https://www.karger.com/Article/Abstract/56361
- de Souza Leão Kamamoto, C., et al. Low-dose oral isotretinoin for moderate to severe seborrhea and seborrheic dermatitis: a randomized comparative trial. International Journal of Dermatology 56, 80 – 85 (2017). https://pubmed.ncbi.nlm.nih.gov/27778328/
- Thiboutot, D. & Chen, W. C. Update and Future of Hormonal Therapy in Acne. Dermatology 206, 57 – 67 (2003). https://www.ncbi.nlm.nih.gov/pubmed/12566806
- Katsambas, A. D. & Dessinioti, C. Hormonal therapy for acne: why not as first line therapy? Facts and controversies. Clin Dermatol 28, 17 – 23 (2010). https://www.ncbi.nlm.nih.gov/pubmed/20082945
- Mahmood, T., Akhtar, N., Khan, B. A., Khan, H. M. & Saeed, T. Outcomes of 3% green tea emulsion on skin sebum production in male volunteers. Bosn J Basic Med Sci 10, 260 – 264 (2010). https://www.ncbi.nlm.nih.gov/pubmed/20846135
- Liao, S. & Hiipakka, R. A. Selective inhibition of steroid 5α-reductase isozymes by tea epicathecin-3-gallate and epigallocatechin-3-gallate. Biochem Biophys Res Commun 214, 833 – 838 (1995). https://www.ncbi.nlm.nih.gov/pubmed/7575552
- Rho, N.-K. & Gil, Y.-C. Botulinum Neurotoxin Type A in the treatment of facial seborrhea and acne: Evidence and a proposed mechanism. Toxins 13, 1 – 12 (2021). https://pubmed.ncbi.nlm.nih.gov/34822601/
- Rose, A. E. & Goldberg, D. J. Safety and Efficacy of Intradermal Injection of Botulinum Toxin for the Treatment of Oily Skin. Dermatol Surg 39, 443 – 448 (2013). https://www.ncbi.nlm.nih.gov/pubmed/23293895
- Salem, R. M., et al. Microbotox injection versus its topical application following microneedling in the treatment of wide facial pores: A split face comparative study. Journal of Cosmetic Dermatology 22,1249-1255 (2022). https://pubmed.ncbi.nlm.nih.gov/36606384/
- Kobayashi, T. & Tamada, S. Selective electrothermolysis of the sebaceous glands: Treatment of facial seborrhea. Dermatol Surg 33, 169 – 177 (2007). https://synapse.koreamed.org/Synapse/Data/PDFData/0140AD/ad-31-75.pdf
- Esler, W. P., et al. Human sebum requires de novo lipogenesis, which is increased in acne vulgaris and suppressed by acetyl-CoA carboxylase inhibition. Sci Transl Med 11(492) (2019). https://www.ncbi.nlm.nih.gov/pubmed/31092695
- Crunkhorn, S. Inhibiting sebum production to treat acne. Nat Rev Drug Discov 18, 498 (2019). https://www.ncbi.nlm.nih.gov/pubmed/31267070
 Acne.org Products
Acne.org Products