Yes, Hormones Play an Important Role in the Development of Cystic Acne in Both Males and Females, and Often the Treatment of Cystic Acne in Females

The Essential Info
Androgens (male hormones present in both males and females) increase the production of skin oil, which can lead to an increase in both regular acne and cystic acne. Generally speaking, the more androgens you have in your blood and skin, the more severe your acne may become.
So this topic is relatively cut and dry. Yes, hormones can cause cystic acne.
Treatments that specifically target hormones are available only to females because they can cause feminizing symptoms in males. They include:
- Oral contraceptives: The birth control pill comes with side effects and concerns, but reliably helps clear cystic acne in most females.
- Spironolactone: Spironolactone is an anti-androgen medication, which means it tamps down on how androgens work in the body. This can also help reduce acne.

The Science
- Hormones Contribute to Both Regular Acne and Nodulocystic Acne
- People with Nodulocystic Acne Have Increased Androgens
- Hormonal Treatments for Nodulocystic Acne
Cystic acne, medically referred to as nodulocystic acne, is an especially severe form of acne that includes large (over 5 mm in diameter) lesions that are red and painful. These lesions, called nodules and cysts, develop deep within the skin, and can take weeks, months, or even longer to heal and often cause scarring.
Hormones play a crucial and central role in the development of all types of acne, including cystic acne.
The main hormones associated with the development of acne in both males and females are androgens, which are male hormones that help control the development of sexual characteristics during puberty in both males and, to a lesser extent, females.
Generally speaking, the more androgens someone has, the more skin oil (sebum) their skin produces, and in turn, the more acne they may experience. When androgens reach high levels, sebum production can go into overdrive, and cystic acne can result.1-4
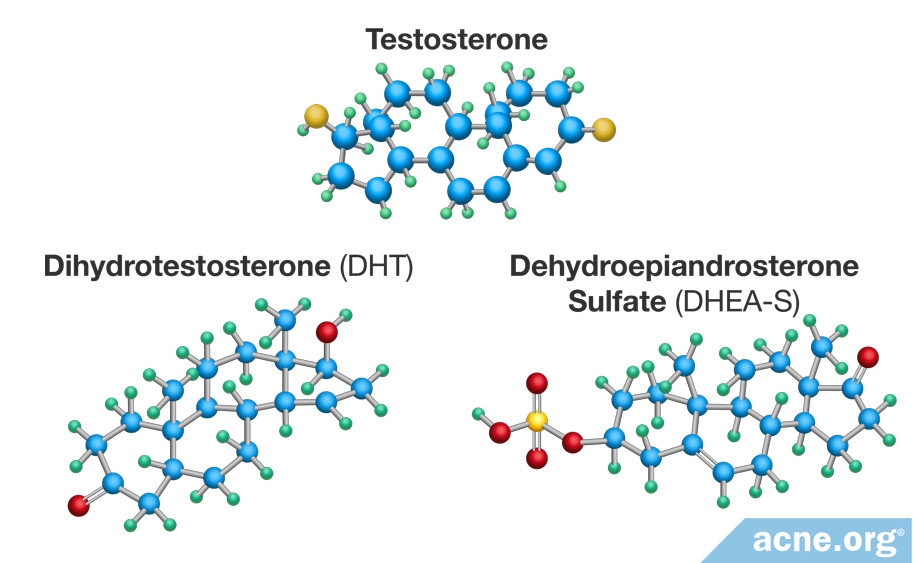
There are three types of androgens that influence acne:
- Dihydrotestosterone (DHT): The most potent androgen
- Testosterone: Another powerful androgen
- Dehydroepiandrosterone sulfate (DHEA-S): A weak androgen that the body can convert into the more powerful testosterone or DHT when needed
In both males and females, beginning at puberty, the sex organs and the adrenal glands (located near the kidneys) begin producing androgens. Once produced, androgens travel in the blood to various areas of the body, including to the skin. When they reach the skin, they enter into skin oil-producing glands, called sebaceous glands, and stimulate the glands to produce more skin oil (sebum).
Hormones Contribute to Both Regular Acne and Nodulocystic Acne
Whether it’s regular acne or severe, nodulocystic acne, hormones are required for acne to form. If you’d like to see exactly how hormones are involved in each step, expand the drawer below:
Expand drawer to read more
Let’s start with learning the three main steps in acne development and how hormones are involved.
- Human skin is covered in tiny hairs, which people usually call pores. Acne begins when the opening of a pore becomes clogged with skin cells, at which point it is called a microcomedone. This clog causes the sebum, which normally drains to the surface, to become trapped inside the pore. How are hormones involved? It is unclear what triggers this initial clog. Traditionally, scientists thought an increase in hormones caused it, but more recent research has shown us that it is likely inflammation is also at fault. To what degree hormones are involved is still under investigation.
- When sebum is trapped inside the pore, it accumulates. At this stage, the acne lesion is called a comedone, more commonly known as a whitehead or blackhead, depending on the appearance of the lesion. Inside the blocked pore, sebum accumulates. When this occurs, the amount of oxygen inside the pore decreases. A type of bacteria called C. acnes thrives in areas abundant in sebum and with little oxygen. Consequently, when the sebum builds up inside the pore, this bacteria begins to reproduce rapidly. How are hormones involved? Androgens play a major role in this step of acne development because they control the production of sebum. More androgens normally mean more sebum.
- The body reacts to the growth of C. acnes inside the pore and sends inflammatory cells to the area to get rid of the excessive bacteria. The inflammatory cells cause inflammation and can make the area red and sore. The “battle” between the inflammatory cells and bacteria weakens the pore wall. This weakened pore wall, combined with the growing pressure caused by the buildup of sebum, causes the pore to rupture. The rupture releases sebum, skin cells, and bacteria into the surrounding skin, which causes even more inflammation. At this point a sore, inflamed pimple, called a papule or pustule is formed. If the pore completely explodes, nodules and cysts may form. How do hormones relate? Androgens play a role in this step because they directly control the production of sebum. More sebum increases pressure inside the pore, causing the pore to expand and rupture.
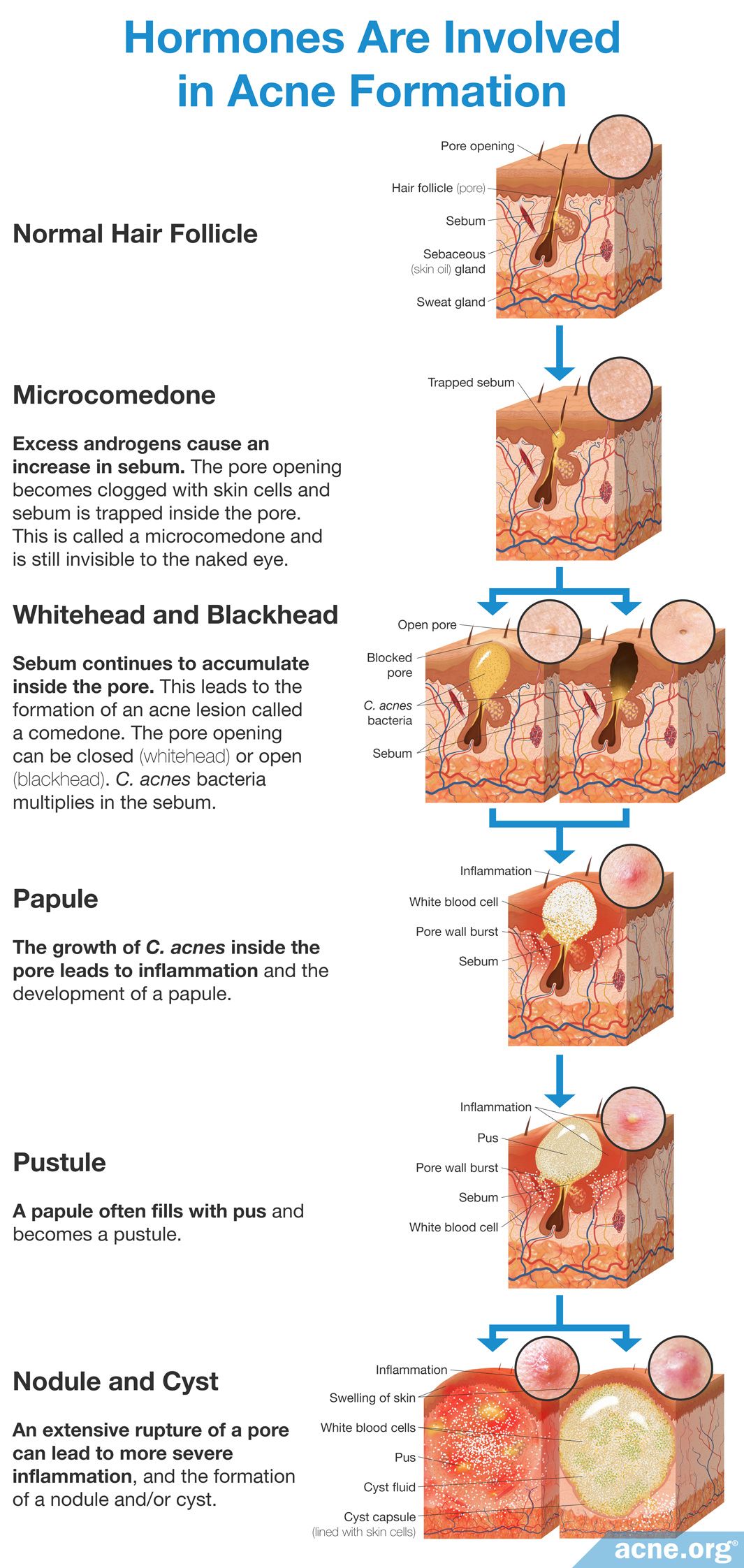
Clearly, many factors influence acne development, but a major one is the production of sebum. Androgens increase sebum production, and therefore can lead to acne lesions, including nodulocystic acne lesions.1-3
People with Nodulocystic Acne Have Increased Androgens
Scientists have performed four studies to look at whether people with nodulocystic acne have elevated androgen levels and have determined that this is in fact the case.5-8
Acne research can often be convoluted and confusing with so many factors at play. However, when it comes to hormones, it is accepted fact that more androgens create more acne and more severe cases of acne.
Expand to read details of studies

A 1983 study published in The New England Journal of Medicine measured the levels of two hormones in 59 female and 32 male nodulocystic acne patients. All 91 patients were resistant to conventional acne treatments. The two hormones tested were DHEA-S and 17-hydroxyprogesterone. DHEA-S is an androgen that is known to increase sebum levels directly. 17-hydroxyprogesterone is a different hormone also produced by the adrenal glands that the body converts into either DHEA-S or testosterone when it needs more androgens. The researchers found that 80% of females and 81% of males had elevated DHEA-S levels, while 14% of females and 34% of males showed elevated 17-hydroxyprogesterone levels. The researchers concluded, “[M]ost patients with therapeutically resistant cystic acne have androgen excess and that lowering elevated [DHEA-S] results in improvement or remission of acne in most instances.”5
A 1985 study published in Clinical and Experimental Dermatology measured the levels of testosterone and other androgens in 42 female and 17 male acne patients. The researchers divided the participants into three groups, based on acne severity. Although the researchers did not explicitly say how they classified acne severity, it is likely that the group labeled as “severe acne group” consisted of patients with nodulocystic acne. There were 19 females and 5 males in the severe acne group. To perform this study, the researchers obtained blood samples from all patients to measure the level of testosterone and other androgens in the blood. They found that testosterone was on average 22.4% higher in the people with acne. However, this number was calculated using all patients with acne, including those who had mild acne. Unfortunately, the authors of the study did not report whether the levels of testosterone were even higher in people with nodulocystic acne. They did report that DHT was elevated in all severe acne patients. However, from this study, it appears that DHT is increased in nodulocystic acne patients.6

A 2014 study published in the Indian Dermatology Online Journal compared hormone levels in 60 females with acne and 60 females without acne. The researchers found significantly higher testosterone levels in females with acne compared to females without acne. They also noted that females with the highest testosterone levels tended to have severe acne. The researchers wrote, “Higher values of [testosterone]…levels were significantly in favor of severe acne.”7

A 2019 study published in the Pakistan Journal of Medical Sciences compared hormone levels in participants with and without acne. The study included 155 women and 115 men with acne as well as 54 women and 26 men without acne. Among the people with acne, 36% had mild acne, 40% had moderate acne, and 24% had severe acne, which likely means nodulocystic acne. We should note that the researchers did not look at how hormone levels differed by gender.
The researchers found that as a group, the people with acne had higher testosterone levels than people without acne. In addition, testosterone levels rose with acne severity; in other words, the people with severe acne had the most testosterone in their blood. However, the scientists found the relationship between testosterone and acne was complex. For example, if one person with acne had twice as much testosterone in their blood as another person with acne, that didn’t necessarily mean they would have twice as many acne lesions.8
To further support the idea that elevated androgen levels tend to go hand-in-hand with severe acne, scientists have also observed that people with rare forms of severe acne also have raised androgens. These rare forms of severe acne include:
- Acne conglobata (a rare, severe form of acne that typically affects males)
- Acne fulminans (a rare, severe form of acne that also includes whole-body symptoms and typically affects young white males)
- SAPHO syndrome (a rare chronic inflammatory syndrome that often includes severe acne)9,10
Hormonal Treatments for Nodulocystic Acne

One option for nodulocystic acne treatment is hormonal therapy. There are three main types of hormonal therapies: cortisone shots, which both males and females can use to treat an occasional nodule or cyst, as well as oral contraceptives and spironolactone, which only females can take.
- Cortisone shots are steroid hormones that are injected directly into a nodule or cyst and can quickly reduce inflammation and initiate healing, helping to prevent scarring. If you have a nodule or cyst, don’t hesitate to make an appointment with your dermatologist for a cortisone shot.
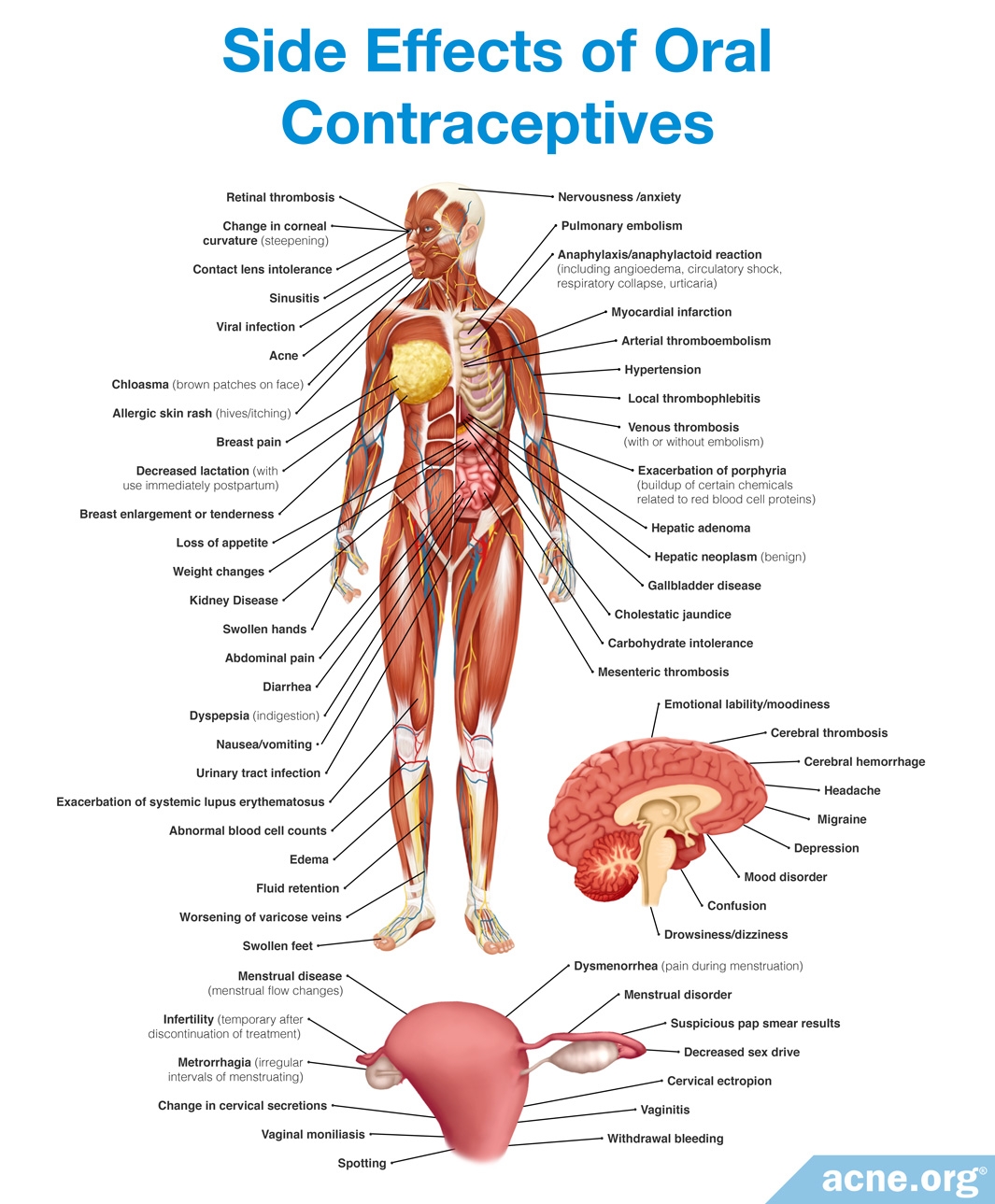
- Oral contraceptives, otherwise known as the birth control pill, are an effective hormonal treatment that females can use, but can come with side effects. In addition to preventing pregnancy, oral contraceptives can calm the effects of androgens and treat acne, reducing it on average by about 60%. They can only be used by females, because in males they can cause feminization symptoms, including breast growth and sexual dysfunction. These also are not appropriate for pregnant women since they can feminize a male fetus.
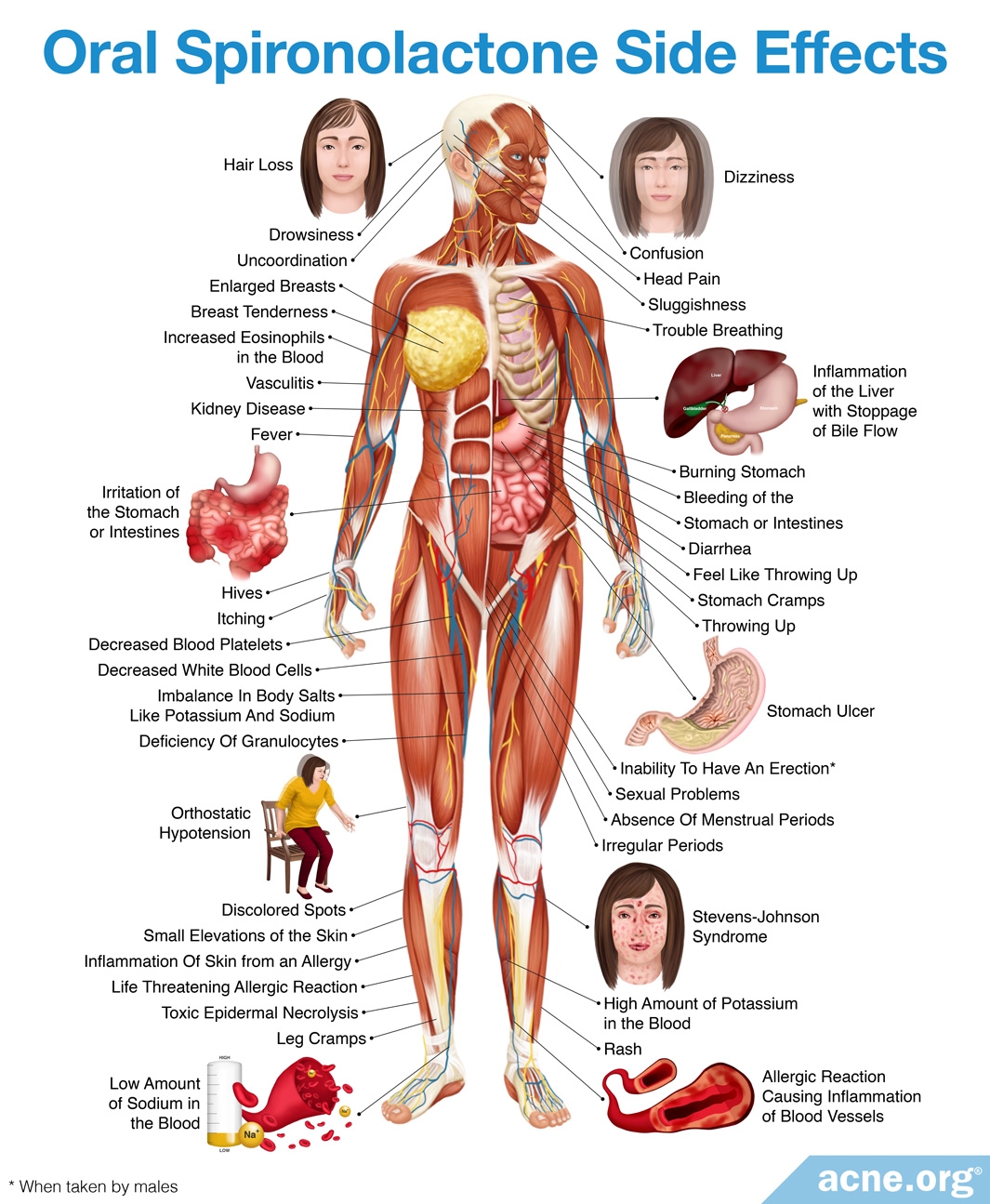
- Spironolactone is a drug called an anti-androgen, which prevents androgens from working. It can be prescribed on its own or alongside an oral contraceptive. Doctors usually only prescribe spironolactone to women because it can also cause feminization and sexual dysfunction symptoms in men.11 It is also not appropriate for pregnant women. Like oral contraceptives, spironolactone is somewhat effective in clearing cystic acne, but can come with side effects.
There are two studies demonstrating the effectiveness of hormonal medications to treat nodulocystic acne, both of which showed that hormonal treatment significantly reduced nodulocystic acne symptoms.5,12
So, if you are a female experiencing cystic acne it may be prudent to get your hormone levels checked and see if this is a treatment route that might be right for you.
Expand to read details of studies

A 1983 study published in The New England Journal of Medicine examined the effect of dexamethasone (corticosteroid) and Demulen (oral contraceptive) to decrease the levels of DHEA-S in males and females. To perform this study, the researchers provided dexamethasone to 32 men with nodulocystic acne, and either dexamethasone, Demulen, or both to 59 female nodulocystic acne patients daily for six months. After the six-month treatment period, the hormonal treatments cleared the nodulocystic acne in 97% of females and 81% of males. More specifically, of the 32 male patients taking dexamethasone, 8 were cleared of their acne; 18 saw a reduction in acne, and 6 noticed no change. Of the 43 female patients taking only dexamethasone, 26 cleared their acne; 15 experienced a reduction in acne, and 2 saw no change. Of the 4 women taking only Demulen, 3 eradicated their acne, and 1 saw a reduction in acne. Of the 12 women taking a combination of dexamethasone and Demulen, 8 cleared their acne, and 4 saw at least a 50% reduction. The researchers concluded, “[M]ost patients with therapeutically resistant acne have androgen excess and lowering [DHEA-S] results in improvement or remission of acne in most instances.”5

A 1984 study published in the British Journal of Dermatology examined the effect of spironolactone on 26 acne patients, of which at least 3 experienced nodulocystic acne. To perform it the patients were given either 100 milligrams (mg) or 200mg of spironolactone per day for three months. The researchers found that of the patients taking 100mg per day, 67% of females and 83% of males demonstrated marked improvement of their acne. The patients who took 200mg daily had the strongest response to the treatment, and 3 patients with nodulocystic acne who had not responded to other treatments significantly improved on a daily 200mg dosage. The researchers concluded that spironolactone may be a useful treatment for general and nodulocystic acne.12
References
- Androgen, https://en.wikipedia.org/wiki/Androgen
- Toyoda, M. & Morohashi, M. Pathogenesis of acne. Med. Electron Microsc. 34, 29 – 40 (2001). https://www.ncbi.nlm.nih.gov/pubmed/11479771
- Degitz, K. et al. Pathophysiology of acne. JDDG 5, 316 – 323 (2007). https://www.ncbi.nlm.nih.gov/pubmed/17376098
- Reingold, S. The relationship of mild hirsutism or acne in women to androgens. Arch. Dermatol. 123, 209 – 212 (1987). https://www.ncbi.nlm.nih.gov/pubmed/2949707
- Marynick, S. et al. Androgen Excess in Cystic Acne. N. Engl. J. Med. 308, 981 – 986 (1983). https://www.nejm.org/doi/10.1056/NEJM198304283081701
- Lawrence, D. et al. Elevated free testosterone concentration in men and women with acne vulgaris. Clin. Exp. Dermatol. 11, 263 – 273 (1986). https://www.ncbi.nlm.nih.gov/pubmed/2943538
- Bakry, O. A., El Shazly, R. M., El Farargy, S. M. & Kotb, D. Role of hormones and blood lipids in the pathogenesis of acne vulgaris in non-obese, non-hirsute females. Indian Dermatol. Online J. 5 (Suppl 1), S9-S16 (2014). https://pubmed.ncbi.nlm.nih.gov/25506579/
- Iftikhar, U. & Choudhry, N. Serum levels of androgens in acne & their role in acne severity. Pak. J. Med. Sci. 35, 146-150 (2019). https://pubmed.ncbi.nlm.nih.gov/30881413/
- Lakshmi, C. Hormone therapy in acne. Indian J. Dermatol. Venereol. Leprol. 79, 322-337 (2013). https://pubmed.ncbi.nlm.nih.gov/23619437/
- Zito, P. M. & Badri, T. Acne Fulminans. [Updated 2020 Apr 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459326/
- Tobechi, L.et al. Hormonal treatment of acne in women. J. Clin. Aesthet. Dermatol. 2, 16 – 22 (2009). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2923944/
- Goodfellow, A. et al. Oral spironolactone improves acne vulgaris and reduces sebum excretion. Br. J. Dermatol. 111, 209 – 214 (1984). https://www.ncbi.nlm.nih.gov/pubmed/6235834
