Red/Dark Spots Left Behind from Acne (Post-inflammatory Hyperpigmentation)

The Essential Info
Post-inflammatory hyperpigmentation, commonly referred to simply as hyperpigmentation, refers to the dark and/or red spots that stay on the skin after acne lesions heal.
Hyperpigmentation is far more common in non-Caucasian skin, and can last for months, and sometimes even years, leading some people to confuse them with scars.
It is not the acne itself that causes hyperpigmentation. Rather it is the skin’s inflammatory response to the acne. This inflammatory response leads to the production of additional skin pigment (melanin), which makes the skin appear darker. Fortunately, hyperpigmentation is not permanent and heals over time.
The 2 Most Important Things to Consider:
- Keep these spots out of the sun, or wear sunscreen when you are in the sun. This will help them fade more quickly.
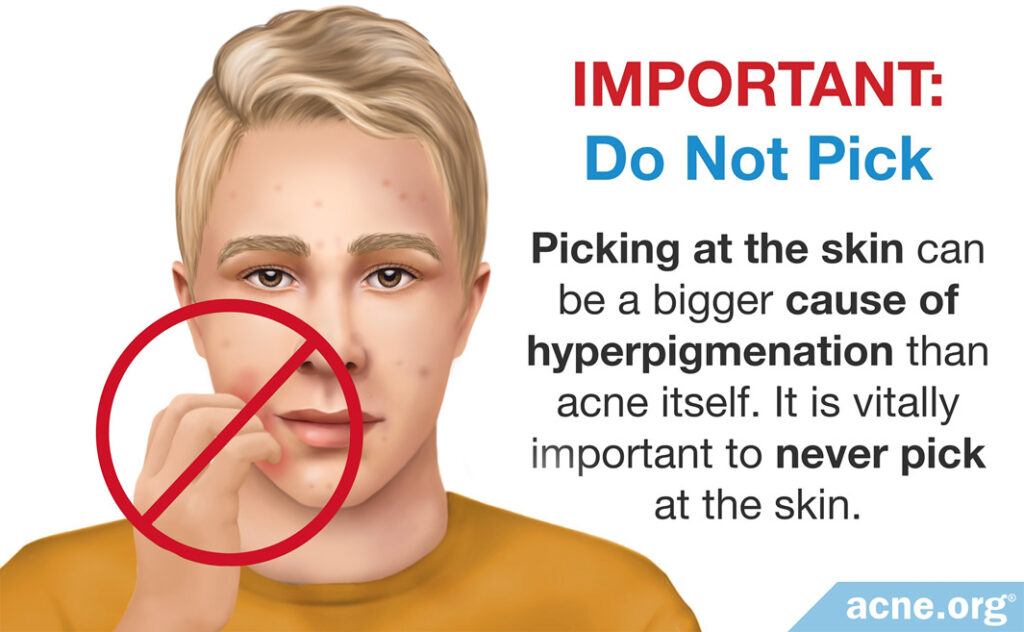
- Don’t pick at acne lesions. Picking can cause more hyperpigmentation than the acne itself.
Popular Topical Treatments:
- Hydroquinone
- Retinoids (tretinoin, adapalene, tazarotene)
- Topical niacinamide (vitamin B3)
- Azelaic acid
- Glycolic acid
Popular Procedure-based Treatments:
- Chemical peels
- Dry ice cryotherapy
- Laser therapy

The Science
- How to Prevent Hyperpigmentation
- How to Treat Hyperpigmentation
- Second-line Treatments of Hyperpigmentation
- The Bottom Line
Post-inflammatory hyperpigmentation (PIH), the red/dark spots that are left behind after acne lesions heal, develops when the inflammation inherent in acne lesions causes skin cells to produce more melanin, which is the pigment that gives skin its color. An increased amount of melanin makes the skin appear darker.
These marks are sometimes referred to as “macules” and can last for months or even years in some cases.
Hyperpigmentation is common among people of African, Asian, and Latino descent, as well as other forms of non-Caucasian skin.1-5 Hyperpigmentation can also occur in Caucasian skin, albeit less frequently.
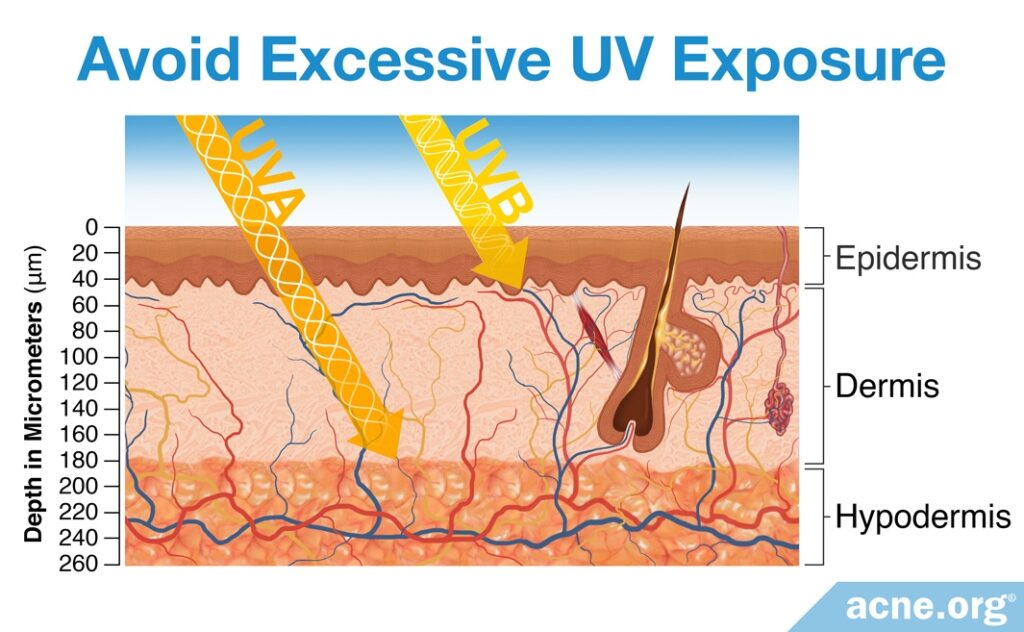
UV light–the light from the rays of the sun–can make hyperpigmentation worse and cause it to remain longer. However, it is not clear whether UV light worsens acne itself, as research studies have reported that UV radiation can both increase6 and decrease7 acne.
Regardless, for all skin types, it is important to take appropriate steps to protect your skin from excessive sun in order to avoid worsening of hyperpigmentation and allow any hyperpigmentation you currently have to heal as fast as possible.
Various forms of acne therapy, such as lasers and chemical peels are often mistakenly blamed for the creation of hyperpigmented marks, but it is the skin’s inflammatory process that creates them.8
Although people often call them scars, they are not permanent and will disappear with time. Nonetheless, they can cause intense distress. Often, people with hyperpigmentation describe this issue as more concerning than the acne itself.
How to Prevent Hyperpigmentation
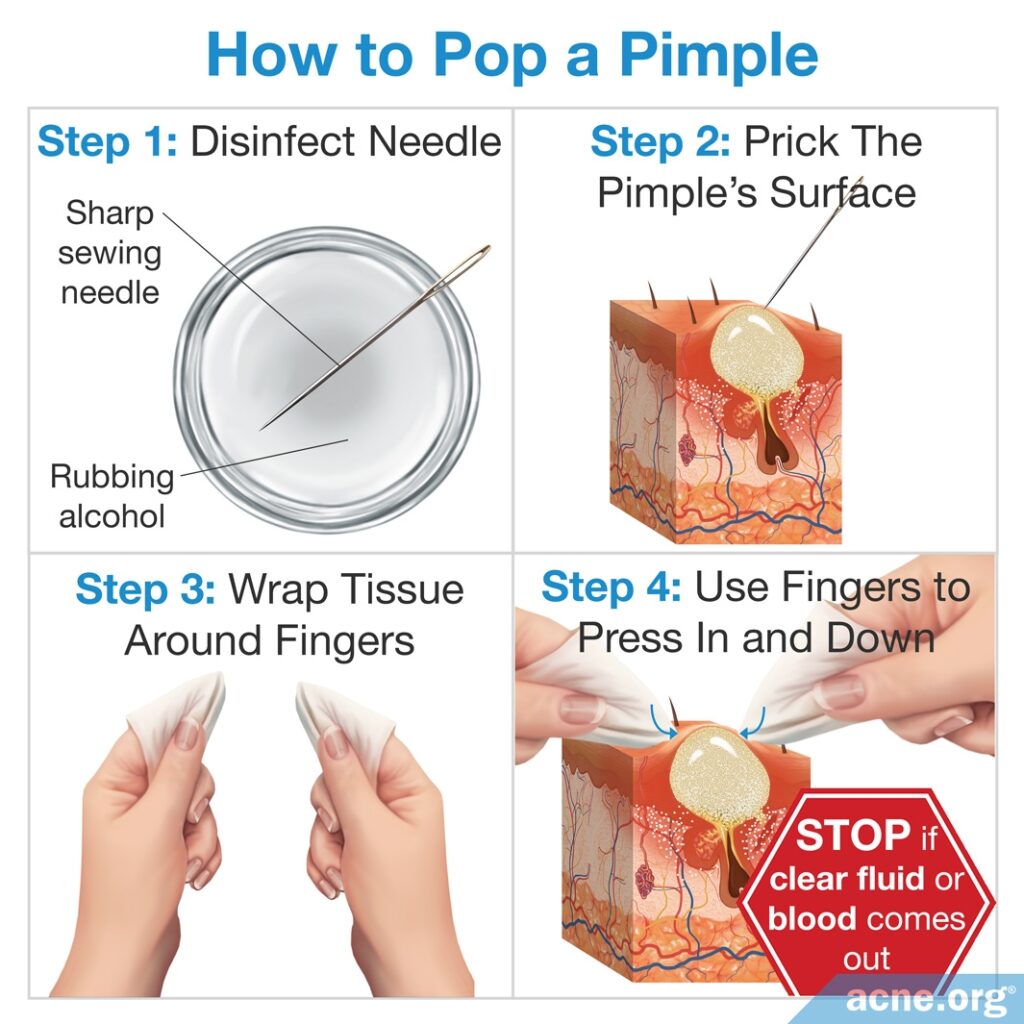
Picking at acne lesions is the worst culprit when it comes to creating hyperpigmentation. Absolutely do not pick at acne lesions. Properly pop a pimple only when it is ready to be popped, and then leave the lesion alone.
Also, while it may seem intuitive to scrub marks away, harsh scrubbing will only prolong their duration and should be avoided. Be sure to wash gently.
Next, as mentioned, keeping hyperpigmented skin out of the sun when possible is a huge help in allowing these marks to fade as quickly as possible. Wearing a sunscreen is important as well.1,5,9
The best way to prevent hyperpigmentation is to treat the acne itself, thus preventing future acne lesions and any hyperpigmentation that they might leave behind.10 Acne is treated the same regardless of skin color and responds extremely well to proper topical treatment with benzoyl peroxide. When acne is severe, widespread, and deeply scarring, Accutane® (isotretinoin) is also an option.
How to Treat Hyperpigmentation

First, get your skin completely clear from active acne. This way you are preventing any future hyperpigmentation.
Once you are clear, you can try a hyperpigmentation treatment to reduce the marks you might have. Topical treatments are the first choice for treating hyperpigmentation. The treatments most commonly prescribed by dermatologists are hydroquinone and retinoids.11
Hydroquinone (Bleach Eze®)
Hydroquinone is often referred to as the “gold standard” for treatment of hyperpigmentation.12
It is normally used at a concentration of 4%. In higher concentrations it can cause “spotted halos,” which appear as lighter colored ring around marks. Hydroquinone treatment results in a marked improvement or complete clearing of PIH in 63% of the patients.4
The efficacy of hydroquinone may be increased by the addition of a retinoid and a low potency corticosteroid, such as hydrocortisone.13
Side effects of hydroquinone include burning, redness, and itching in 30% of the patients.12 The addition of ascorbic acid (Vitamin C) to a topical hydroquinone treatment may help minimize side effects.2-3
Hyperpigmentation starts to subside after 4 weeks of hydroquinone treatment, but maximum results usually require 8 to 12 weeks of treatment. Be certain to work closely with your physician or dermatologist if you decide to use hydroquinone to ensure proper dosage and reduction of side effects.
Retinoids: Tretinoin (Retin-A®), Adapalene (Differin®), Tazarotene (Tazorac®), or Trifarotene (Aklief®)
Most people are familiar with retinoids as prescription topical acne treatments. However, they can also be used to treat hyperpigmentation, and are typically used together with hydroquinone.14
According to one study, retinoids can treat hyperpigmentation by increasing the rate at which old skin cells are replaced with new ones.8
Another study found that daily treatment with retinoids resulted in slightly or even significantly lightened marks in the majority of participants.15
Expand to read details of studies

According to the Journal of the American Academy of Dermatology, “Of particular significance to skin of color patients is the ability of retinoids to treat both acne and PIH. By increasing epidermal turnover, these agents facilitate melanin dispersion and removal.”8

A study published in The New England Journal of Medicine on people with skin that was darkened by hyperpigmentation showed that daily retinoid treatment resulted in “much lighter” skin in 53% of participants and in “somewhat lighter” skin in an additional 33% of patients.15
If retinoids are used alone and not in combination with hydroquinone, dermatologists often prescribe a topical corticosteroid in order to reduce the irritation and potential worsening of PIH that retinoids can cause when they are used alone. An expert opinion in Skin Therapy Letters sums it up: “The use of retinoids as monotherapy is not recommended as an irritant reaction may cause inflammation that induces paradoxical hyperpigmentation; a similar concern exists over the use of HQ as monotherapy at very high concentrations (i.e., 8-20%).”12
Retinoids typically take 8 to 12 weeks to produce maximum results. The frequency and concentration of retinoid therapy depends on the severity of hyperpigmentation and should be determined by a dermatologist.
Niacinamide, also known as Nicotinamide
Niacinamide is a B vitamin that can be administered topically, and is currently being investigated as a potential therapy for hyperpigmentation. One recent study tested a topical treatment containing niacinamide on people with hyperpigmentation due to a non-acne skin condition and found that two months of treatment reduced the hyperpigmentation.16
Expand to read details of study

A study published in the journal Cutis in 2015 showed that a topical cream containing 4% niacinamide in combination with the other pigment-lightening and anti-inflammatory compounds arbutin, bisabolol, and retinaldehyde reduced hyperpigmentation due to melasma by 34% over a period of two months. Melasma is a common skin problem where brown marks appear on the face due to pregnancy or sun exposure.16
To date, there exists no published research that has investigated whether niacinamide is also effective in treating PIH, but studies are currently in progress.
Azelaic Acid
Azelaic acid is another topical acne prescription that is sometimes used for PIH that works by slowing down the production of melanin.
It is a gel that doctors normally prescribe in 20% concentration for PIH, applied twice a day.
Azelaic acid is safe and effective for the treatment of both acne and PIH conditions in darker skin types.
Common side effects include mild redness, scaling, and burning.17
Due to the mechanism of action of azelaic acid, results are not seen for the first few months of azelaic acid treatment, but results are eventually seen after six months.
Second-line Treatments of Hyperpigmentation
Chemical Peels
Chemical peels are often employed if topical therapy fails. While this treatment can be effective in treating PIH, it can also worsen hyperpigmentation if used incorrectly. It should therefore be administered by an experienced professional who specializes in PIH.18
Superficial chemical peels, which include salicylic acid, Jessner’s solution, lactic acid, mandelic acid, and glycolic acid cause the fewest side effects and are the preferred choice of chemical peels for hyperpigmentation. For example, one recent study tested three different superficial chemical peels on people of Asian descent with acne and found that each of the three chemical peels significantly reduced PIH.19
Expand to read details of study
A study published in the Journal of Cutaneous and Aesthetic Surgery in 2019 tested three types of superficial chemical peels on 45 Asian patients with acne and post-inflammatory hyperpigmentation. The researchers divided the patients into 3 groups:
- Group A received a 35% glycolic acid chemical peel
- Group B received a 20% salicylic acid – 10% mandelic acid chemical peel
- Group C received a phytic acid chemical peel
The patients in each group were treated with a chemical peel every other week, for a total of 6 sessions in 12 weeks. At the end of this period, the researchers found an improvement in the percentage of the face covered with PIH in all groups:
- In Group A, the percentage of the face covered with PIH decreased from 21.53% to 8.8%
- In Group B, the percentage of the face covered with PIH decreased from 17.16% to 3.1%
- In Group C, the percentage of the face covered with PIH decreased from 16.8% to 7.1%
The scientists concluded that superficial chemical peels are effective at reducing PIH in Asian patients with acne.19
Peels that penetrate more deeply into the skin, such as TCA peel, Jessner’s/TCA combination peel and phenol, result in more serious side effects such as pain and burning sensations as well as the potential to worsen pigmentation, and are therefore not recommended.1-3,12,20
Over-the-counter Peeling
Over-the-counter glycolic acid products are available in strengths up to 10% and can provide gentle exfoliation.
At lower percentages in over-the-counter products, glycolic acid does not cause the skin to visibly peel off in sheets like professionally administered chemical peels do, and instead provides exfoliation of only the surface cells of the skin. This is a slower and safer way to achieve the skin turnover required to reduce hyperpigmentation and can be used on a more frequent basis when compared to chemical peels.
Most people find that they can tolerate over-the-counter 10% glycolic acid products only once every other day, or once a day when mixed ½ and ½ with moisturizer. DO NOT use them more often than this.
Botanical and Natural Ingredients
Botanical (plant-based) and natural extracts have been gaining attention as potential alternatives to hydroquinone. These extracts include soy, lignin peroxidase, aloesin, arbutin, ellagic acid, licorice, mulberry, and myrtle. While many of these ingredients show promise in the lab or in short-term trials on people, more long-term, randomized, controlled studies are necessary to determine how effective these ingredients really are at reducing hyperpigmentation.21,22
Dry ice cryotherapy

Doctors will sometimes use application of dry ice to help the mark fade.
Laser Treatment

Laser therapy tends to produce results on par with topical treatment.23,24 However, the use of lasers to treat hyperpigmentation is controversial because research suggests that they can worsen hyperpigmentation in some cases or make the skin more sensitive to the sun.11,12

According to an article in the journal Dermatology Clinics, “Although lasers are reported in many studies to be helpful for the treatment of melasma (and in some instances PIH), in reality, there is a significant limitation to laser-based devices for pigmentation given the risk of rebound pigmentation or worsening, even with conservative treatment.”11 In addition, laser therapy can cause the skin to become more sensitive to the sun, necessitating “an intensive brightening, anti-inflammatory, and sun-protective skin care regimen” following treatment.12
Microdermabrasion
Performed at salons and estheticians’ offices, microdermabrasion helps remove the upper layers of skin cells. However, results are unimpressive and abrading the skin can cause irritation, which perpetuates the acne cycle. Microdermabrasion should be avoided in acne-prone individuals.2-3
The Bottom Line
Whichever treatment option(s) you choose, remember that taking preventative steps to limit hyperpigmentation in the first place can go a long way toward getting a handle on this problem. Always wear sunscreen, limit your time in the sun, and avoid picking at the skin. In time, you will see improvements in the appearance of your skin.
References
- Dunwell, P. & Rose, A. Study of the skin disease spectrum occurring in an Afro-Caribbean population. Int. J. Dermatol. 42, 287 – 289 (2003). https://www.ncbi.nlm.nih.gov/pubmed/12694494
- Alexis, A. F. & Lamb, A. Concomitant therapy for acne in patients with skin of color: a case-based approach. Dermatol. Nurs. 21, 33 – 36 (2009). https://www.ncbi.nlm.nih.gov/pubmed/19283960
- Yahya, H. Acne vulgaris in Nigerian adolescents–prevalence, severity, beliefs, perceptions, and practices. Int. J. Dermatol. 48, 498 – 505 (2009). https://www.ncbi.nlm.nih.gov/pubmed/19416381
- Callender, V. D., St Surin-Lord, S., Davis, E. C. & Maclin, M. Postinflammatory hyperpigmentation: etiologic and therapeutic considerations. Am. J. Clin. Dermatol. 12, 87 – 99 (2011). https://www.ncbi.nlm.nih.gov/pubmed/21348540
- Jacyk, W. K. Adapalene in the treatment of African patients. J. Eur. Acad. Dermatol. Venereol. 15 Suppl 3, 37 – 42 (2001). https://www.ncbi.nlm.nih.gov/pubmed/11843232
- Mills, O. H., Porte, M. & Kligman, A. M. Enhancement of comedogenic substances by ultraviolet radiation. Br. J. Dermatol. 98, 145 – 150 (1978). https://www.ncbi.nlm.nih.gov/pubmed/147099
- Lee, W. J. et al. Inflammatory Cytokine Expression and Sebum Production after Exposure of Cultured Human Sebocytes to Ultraviolet A Radiation and Light at Wavelengths of 650 nm and 830 nm. Ann. Dermatol. 27, 163 – 170 (2015). https://www.ncbi.nlm.nih.gov/pubmed/25834355
- Taylor, S. C., Cook-Bolden, F., Rahman, Z. & Strachan, D. Acne vulgaris in skin of color. J. Am. Acad. Dermatol. 46, S98 – 106 (2002). https://www.ncbi.nlm.nih.gov/pubmed/11807471
- Halder, R. M. & Nootheti, P. K. Ethnic skin disorders overview. J. Am. Acad. Dermatol. 48, S143 – 148 (2003). https://www.ncbi.nlm.nih.gov/pubmed/12789168
- Shah, S. K. & Alexis, A. F. Acne in skin of color: practical approaches to treatment. J. Dermatolog. Treat. 21, 206 – 211 (2010). https://www.ncbi.nlm.nih.gov/pubmed/20132053
- Molinar, V. E., Taylor, S. C. & Pandya, A. G. What’s new in objective assessment and treatment of facial hyperpigmentation? Dermatol. Clin. 32, 123 – 135 (2014). https://www.ncbi.nlm.nih.gov/pubmed/24679999
- Sofen, B., Prado, G. & Emer, J. Melasma and Post Inflammatory Hyperpigmentation: Management Update and Expert Opinion. Skin Therapy Lett. 21, 1 – 7 (2016). https://www.ncbi.nlm.nih.gov/pubmed/27224897
- Chandra, M., Levitt, J. & Pensabene, C. A. Hydroquinone therapy for post-inflammatory hyperpigmentation secondary to acne: not just prescribable by dermatologists. Acta Derm. Venereol. 92, 232 – 235 (2012). https://www.ncbi.nlm.nih.gov/pubmed/22002814
- Callender, V. D., Baldwin, H., Cook-Bolden, F. E., Alexis, A. F., Stein Gold, L. & Guenin, E. Effects of topical retinoids on acne and post-inflammatory hyperpigmentation in patients with skin of color: A clinical review and implications for practice. Am. J. Clin. Dermatol. 23, 69-81 (2022). https://pubmed.ncbi.nlm.nih.gov/34751927/
- Bulengo-Ransby, S. M. et al. Topical tretinoin (retinoic acid) therapy for hyperpigmented lesions caused by inflammation of the skin in black patients. N. Engl. J. Med. 328, 1438 – 1443 (1993). https://www.nejm.org/doi/full/10.1056/NEJM199305203282002
- Crocco, E. I., Veasey, J. V., Boin, M. F., Lellis, R. F. & Alves, R. O. A novel cream formulation containing nicotinamide 4%, arbutin 3%, bisabolol 1%, and retinaldehyde 0.05% for treatment of epidermal melasma. Cutis 96, 337 – 342 (2015). https://www.ncbi.nlm.nih.gov/pubmed/26682557
- Rossi, A. M. & Perez, M. I. Treatment of hyperpigmentation. Facial Plast. Surg. Clin. North Am. 19, 313 – 324 (2011). https://www.ncbi.nlm.nih.gov/pubmed/21763992
- Eimpunth, S., Wanitphadeedecha, R. & Manuskiatti, W. A focused review on acne-induced and aesthetic procedure-related postinflammatory hyperpigmentation in Asians. J. Eur. Acad. Dermatol. Venereol. 27 Suppl 1, 7 – 18 (2013). https://www.ncbi.nlm.nih.gov/pubmed/23205540
- Sarkar, R., Ghunawat, S. & Garg, V. 1. Comparative study of 35% glycolic acid, 20% salicylic-10% mandelic acid, and phytic acid combination peels in the treatment of active acne and postacne pigmentation. J. Cutan. Aesthet. Surg. 12, 158-163 (2019). https://www.ncbi.nlm.nih.gov/pubmed/31619887
- Davis, E. C. & Callender, V. D. A review of acne in ethnic skin: pathogenesis, clinical manifestations, and management strategies. J. Clin. Aesthet. Dermatol. 3, 24 – 38 (2010). https://www.ncbi.nlm.nih.gov/pubmed/20725545
- Hollinger, J. C., Angra, K. & Halder, R. M. Are natural ingredients effective in the management of hyperpigmentation? A systematic review. J. Clin. Aesthet. Dermatol. 11, 28 – 37 (2018). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5843359/
- Bagatin, E., Thouvenin, M. D., Bacquey, A., Baradat, S., Lauze, C., Mengeaud, V., Soares, J. L. M., Andrade, L. S. M., Miot, H. A. & Rocha, M. A. The usefulness of a dermocosmetic containing Myrtus communis extract and azelaic acid for maintenance phase of adult female acne: Results from a randomized exploratory investigator-blinded comparative study. J. Eur. Acad. Dermatol. Venereol. 2, 26-30 (2023). https://pubmed.ncbi.nlm.nih.gov/36729399/
- Kane, A., Niang, S. O., Diagne, A. C., Ly, F. & Ndiaye, B. Epidemiologic, clinical, and therapeutic features of acne in Dakar, Senegal. Int. J. Dermatol. 46 Suppl 1, 36 – 38 (2007). https://www.ncbi.nlm.nih.gov/pubmed/17919205
- Poli, F. Acne on pigmented skin. Int. J. Dermatol. 46 Suppl 1, 39 – 41 (2007). https://www.ncbi.nlm.nih.gov/pubmed/17919206
 Acne.org Products
Acne.org Products