Cortisol Is a Hormone That Affects the Factors Involved in Acne – Sometimes for the Better, Sometimes for the Worse

The Essential Info
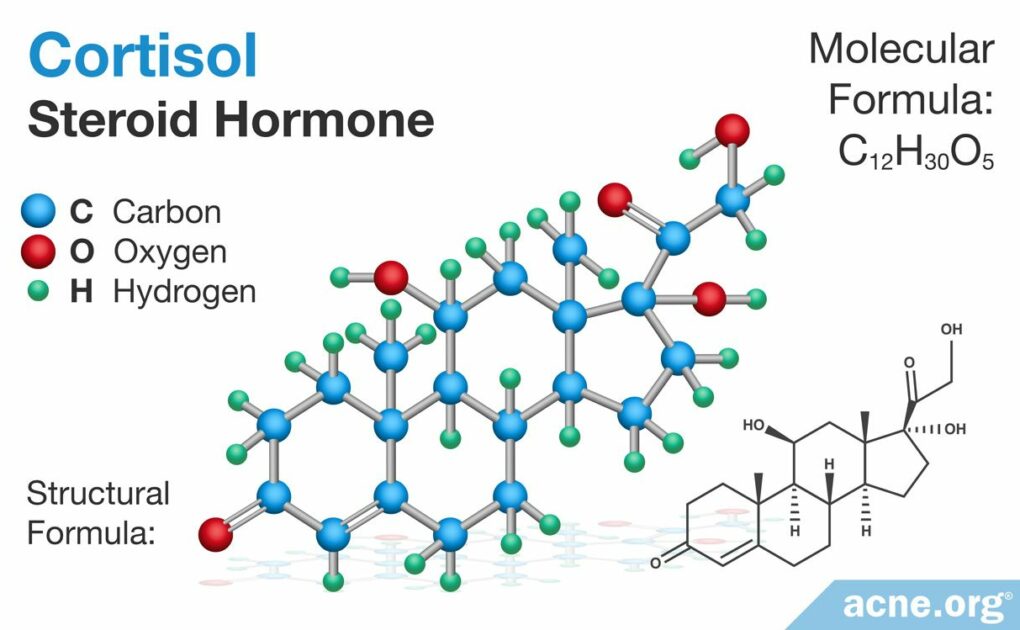
Cortisol is a steroid hormone that is present in almost every human cell and has far-reaching effects on the body. Cortisol is released in response to stress, and chronic, ongoing stress can lead to elevated levels in the body, which may worsen acne. Too little cortisone comes with its own problems in the body, so keeping cortisol balanced is important. When it comes to acne, reducing stress is the best way to balance cortisol levels.

The Science
- Factors That Trigger Acne Development
- Topical Cortisol (Hydrocortisone): It’s Complex Impact on Acne
- Isotretinoin Treatment Decreases Glucocorticoid Levels
- Conclusion
Acne is an inflammatory disease that is, in part, caused by inflammation in the skin. Normally, inflammation is the body’s response to harm. However, inflammation that is improperly controlled can harm the body and diseases such as acne. Therefore, any molecule that regulates and controls the inflammatory process in the skin may impact acne. Cortisol is a glucocorticoid (steroid hormone) that regulates inflammation in the body, including the skin. Generally, the body creates cortisol in response to stress. However, it also acts throughout the body to regulate growth, development, and behavior, such as sleep cycles. Too much or too little cortisol can result in harmful inflammation. In the skin, cortisol regulates inflammation. And because acne is an inflammatory disease, cortisol may positively or negatively impact its development, depending on how it regulates the skin’s inflammatory processes.1,2
Caution: Deep Science Ahead. This is interesting stuff, but just be forewarned that we will be diving pretty deep here.
Factors That Trigger Acne Development
Although acne is primarily an inflammatory disease, there are several other triggers that can worsen acne. Cortisol and inflammation play a role in each of these factors.
- A damaged skin barrier causes skin dehydration and dry, flaky, disease-prone skin. Normally, the skin barrier keeps the skin hydrated and moisturized, but it can be damaged by the use of harsh chemicals and scrubbing. When the skin barrier is damaged, the immune system tries to repair it through inflammation. Cortisol helps regulate inflammation, and misregulation of inflammation can harm the skin and cause diseases such as acne.1
- An overproduction of keratin and sebum (skin oil) can clog skin pores. Acne-prone skin contains low levels of cortisol, and this causes an overproduction of a protein called keratin, which can clog pores.3
- The growth of the bacteria, C. acnes, stimulates the body to produce more inflammation. Because cortisol helps regulate inflammation, low levels of it can result in worsening of acne.
- An impaired wound-healing process can slow acne healing, leaving scars and skin hyperpigmentation. Upon the formation of an acne lesion, the immune system immediately begins promoting inflammation to repair the skin. Skin cells respond to the stress of inflammation and the acne lesions by producing cortisol. Unfortunately, cortisol slows the production of new skin cells needed to heal an acne lesion.1
Each of these factors, combined with inflammation, contributes to the formation of an acne lesion. However, it is unclear which factor is the first to trigger the inflammatory response and the formation of acne. Despite this, the skin releases cortisol in response to the stress of the inflammation in the clogged pore. Cortisol then impairs the wound-healing process by slowing the production of new skin cells. Therefore, proper levels and regulation of inflammation and cortisol are crucial in all aspects of acne development, from lesion formation to wound healing.3,4
Topical Cortisol (Hydrocortisone): It’s Complex Impact on Acne
You may have heard of hydrocortisone, a topical medication that can help reduce inflammation and itching. Topical hydrocortisone is basically topical cortisol. This begs the question, can topical hydrocortisone help reduce acne? The answer is complex because of the wide-ranging effects of glucocorticoids like cortisol, and shows us that most likely applying topical hydrocortisone is not warranted when it comes to acne.
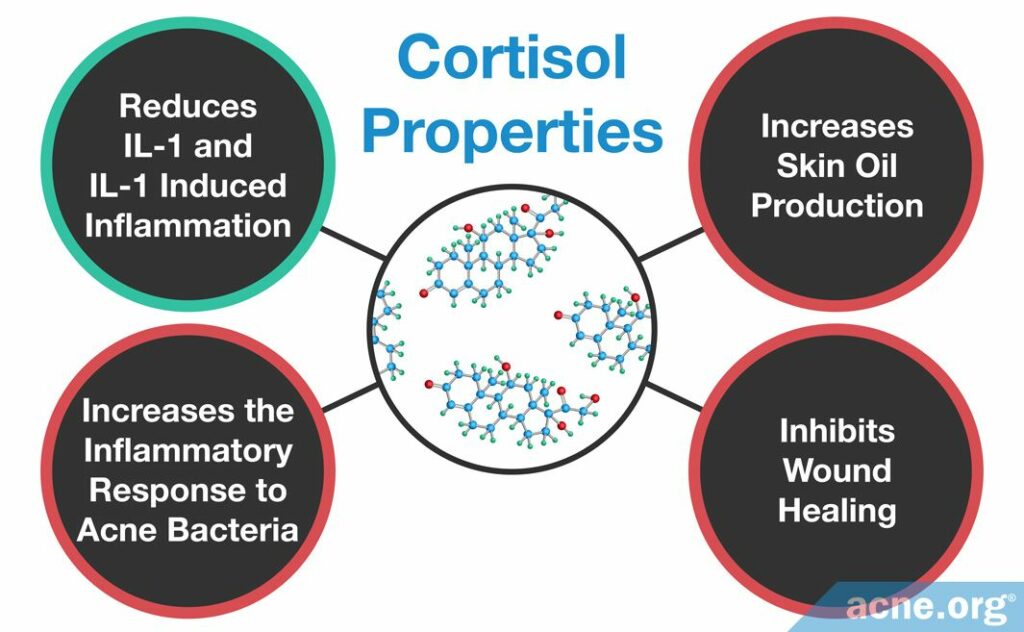
Cortisol is the most important glucocorticoid in the body. Glucocorticoids are able to activate some inflammatory molecules while repressing others. They also come with severe long-term side effects, so this rules them out as long-term treatments. Still, let’s have a look at the research performed on topical glucocorticoids which finds that glucocorticoids can temporarily worsen acne lesions in some people but improve severe acne in others. Why the conflicting results? Let’s examine the 4 ways that glucocorticoids may impact acne development.3,5,6 Note that 3 out of 4 point toward topical glucocorticoids, like cortisol (hydrocortisone) actually worsening acne instead of improving it.
- Glucocorticoids reduce IL-1 and IL-1-induced inflammation and may improve acne
Interleukin-1 (IL-1) is an inflammatory molecule that is highly associated with acne. It is found at higher concentrations in acne-prone skin and also is one of the earliest inflammatory molecules present in a new acne lesion. Some scientists believe that it may be the molecule that triggers the formation of an acne lesion. IL-1 is regulated by glucocorticoids, such as cortisol.
A 2000 study published in American Journal of Physiology investigated the sensitivity of IL-1 to hydrocortisone, which is a medication equivalent to cortisol produced in the body. They performed this study by treating blood cells obtained from men and from women with various concentrations of hydrocortisone. They found that the blood cells released less IL-1 in response to higher concentrations of hydrocortisone. This means that cortisol likely can inhibit the production of IL-1, which would cause an anti-inflammatory response that may decrease the inflammation inherent to acne lesions.7
- Glucocorticoids increase skin oil (sebum) production and may worsen acne
Skin oil, called sebum, is required for acne development. Generally speaking, the more sebum that is produced, the more acne we see.

A 2013 study published in British Journal of Dermatology found that sebum production is affected by glucocorticoids. Specifically, this research focused on 11β-HSD1, which is the protein that creates cortisol in the skin. The scientists found that the levels of 11β-HSD1 in the skin were higher in acne patients than in non-acne patients. This suggests that the skin of acne patients produces cortisol in higher amounts when compared to the skin of non-acne patients. This study also found that the when there were high levels of 11β-HSD1, there were high levels of sebum. This suggests that in acne patients the amount of 11β-HSD1 increases the level of cortisol, and this leads to an increase in sebum production. The researchers proposed that treating acne may be possible by creating a drug that blocks the function of 11β-HSD1. However more research is needed in order to prove this hypothesis.6
- Glucocorticoids increase the inflammatory response to acne bacteria (C. acnes) and may worsen acne
Cutibacterium acnes C. acnes) is a type of bacteria often present growing inside a clogged pore. It thrives in the nutrient-rich environment of sebum and keratin, a protein found in skin cells. This results in excessive growth of the bacteria, which further swells the pore. Keratinocytes (the skin cells surrounding the pore) can recognize the bacteria via special proteins called toll-like receptors (TLRs), found on their surface. One TLR, called TLR2, recognizes C. acnes and triggers cells to begin producing inflammatory molecules and recruiting other immune system cells in order to fight the infection.
A 2009 study published in the Journal of Investigative Dermatology found that glucocorticoids can increase the amount of TLR2 produced in skin cells grown in a laboratory. If there is a larger amount of TLR2 on the surface of skin cells, then they are more sensitive to the presence of C. acnes and more likely to trigger an inflammatory response than smaller levels of C. acnes. Therefore, in this way, glucocorticoids may increase the inflammatory response characteristic of an acne lesion.8
- Glucocorticoids inhibit wound healing and may worsen acne
Acne lesions must heal properly in order to avoid leaving scars and hyperpigmentation on the skin. Therefore, the wound healing process is crucial to preventing permanent damage caused by acne lesions.
A 2011 study published in the Journal of Biological Chemistry found that the levels of glucocorticoids are increased due to skin damage but that high levels of glucocorticoids actually decrease and slow the wound-healing process. They also found that when they artificially blocked the enzyme that creates cortisol, the production of IL-1 increased, and wound healing accelerated. In other words, when an acne lesions forms, IL-1 is produced, and this stimulates inflammation and the wound-healing process. But upon the release of cortisol, wound healing slows.9

Another study, published in 2016 in the Archives of General Psychiatry, found that mental stress also increased cortisol, which slowed wound healing. To perform this study, the researchers made wounds in the forearms of 36 women and monitored the levels of glucocorticoids and how fast the forearm wounds healed. Women who healed slowest were those who were most stressed, had the highest levels of cortisol, and had the lowest levels of IL-1.10 Although this study focused on metal stress and wound healing instead of acne lesions and wound healing, it is clear that glucocorticoids slow the wound-healing process and therefore likely would slow the healing of an acne lesion.
Clearly, the effect of glucocorticoids on acne is complex. Some factors, such as IL-1 reduction, may improve acne, while others, such as the effect of sebum production, response to C. acnes, and influence on wound healing, may worsen acne. However, it is clear that improper levels of glucocorticoids, including cortisol, can cause a variety of effects on the skin that may worsen acne.
Isotretinoin Treatment Decreases Glucocorticoid Levels
One common treatment for severe acne is isotretinoin, otherwise known as Accutane®. Isotretinoin, although effective in treating some types of acne, comes with severe side effects, one of which is causing birth defects. It is unclear exactly how isotretinoin treats acne, but we do know that it dramatically and often permanently decreases sebum production.

A 2011 study published in Acta Dermato-Venereologica sought to understand how isotretinoin affects the production of hormones, including cortisol. After three months of isotretinoin treatment, the researchers observed an average decrease in cortisol levels from 13.1 to 11 in the 47 acne patients participating in the study.11

A second study, published in 2015 in Dermatology, found that after three months of isotretinoin treatment, the levels of cortisol decreased on average from 15.0 to 11.8 in the 105 acne patients participating in the study.12 The researchers proposed that isotretinoin decreases glucocorticoid levels, which may improve acne.
Conclusion
In the skin, cortisol regulates inflammation. Acne is an inflammatory disease, so cortisol is important in the formation and healing of acne lesions. Research has found that glucocorticoids, including cortisol, affect the factors involved in acne development, sometimes for the better and sometimes for the worse. These include regulating IL-1-induced inflammation, sebum (skin oil) production, C. acnes growth and inflammation, and wound healing. Because of cortisol’s skin function complexity, scientists are unable to determine how improper cortisol levels worsen or improve acne. However, it is clear that abnormally high or low cortisol levels can result in inflammation, which is harmful if misregulated. Overall, more research is needed in order to identify how cortisol and other glucocorticoids affect acne and potential treatments, which would target improper glucocorticoids levels.
References
- Terao, M. & Katayama, I. Local cortisol/corticosterone activation in skin physiology and pathology. J Dermatol Sci 84, 11 – 16 (2016). https://www.ncbi.nlm.nih.gov/pubmed/27431412
- Hardy, R. S., Raza, K. & Cooper, M. S. Endogenous glucocorticoids in inflammation: contributions of systemic and local responses. Swiss Med Wkly 142, 1 – 10 (2012). https://www.ncbi.nlm.nih.gov/pubmed/22869348
- Nikolakis, G. & Zouboulis, C. C. Skin and glucocorticoids: effects of local skin glucocorticoid impairment on skin homeostasis. Exp Dermatol 23, 807 – 808 (2014). https://www.ncbi.nlm.nih.gov/pubmed/25056134
- Slominski, A. et al. Steroidogenesis in the skin: implications for local immune functions. J Steroid Biochem Mol Biol 137, 107 – 123 (2013). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3674137/
- Franchimont, D. Overview of the actions of glucocorticoids on the immune response: A good model to characterize new pathways of immunosuppression for new treatment strategies. Ann N Y Acad Sci 1024, 124 – 137 (2004). https://www.ncbi.nlm.nih.gov/pubmed/15265777
- Lee, S. E., Kim, J. M., Jeong, M. K., Zouboulis, C. C. & Lee, S. H. 11β-hydroxysteroid dehydrogenase type 1 is expressed in human sebaceous glands and regulates glucocorticoid-induced lipid synthesis and toll-like receptor 2 expression in SZ95 sebocytes. Br J Dermatol 168, 47 – 55 (2013). https://www.ncbi.nlm.nih.gov/pubmed/22897663
- Daun, J. M. et al. Glucocorticoid sensitivity of interleukin-1 agonist and antagonist secretion : the effects of age and gender. Am J Physiol – Regul Integr Comp Physiol 278, 855 – 862 (2000). https://www.ncbi.nlm.nih.gov/pubmed/10749772
- Shibata, M., Katsuyama, M., Onodera, T., Ehama, R. & Hosoi, J. Glucocorticoids enhance toll-like receptor 2 expression in human keratinocytes stimulated with Propionibacterium acnes or proinflammatory cytokines. J Invest Dermatol 129, 375 – 382 (2009). https://www.ncbi.nlm.nih.gov/pubmed/18704103
- Vukelic, S. et al. Cortisol synthesis in epidermis is Induced by IL-1 and tissue injury. J Biol Chem 286, 10265 – 10275 (2011). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3060481/
- Glaser, R. et al. Stress-related changes in proinflammatory cytokine production in wounds. Arch Gen Psychiatry 56, 450 – 456 (2016). https://www.ncbi.nlm.nih.gov/pubmed/10232300
- Karadag, S. A., Ertugrul, D. T., Tutal, E. & Akin, K. O. Isotretinoin influences pituitary hormone levels in acne patients. Acta Derm Venereol 91, 31 – 34 (2011). https://www.ncbi.nlm.nih.gov/pubmed/21103844
- Karadag, A. S. et al. The Effect of Different Doses of Isotretinoin on Pituitary Hormones. Dermatology 230, 354 – 359 (2015). https://www.ncbi.nlm.nih.gov/pubmed/25721216
 Acne.org Products
Acne.org Products