PCOS Is a Hormonal Disease That Affects the Ovaries and Can Lead to Acne: 19 – 37% of Females with Moderate-to-Severe Acne May Have This Disorder

The Essential Info
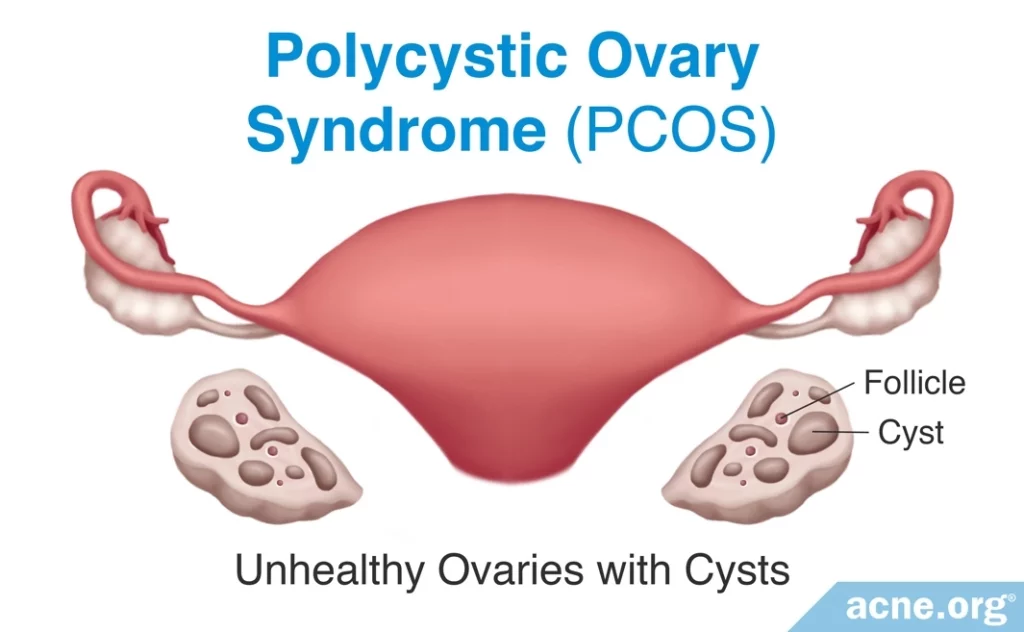
Polycystic ovary syndrome (PCOS) is a common hormonal disorder that affects females. It is characterized by:
- Ovaries with a high number of cysts
- Irregular ovulation
- High male hormone levels
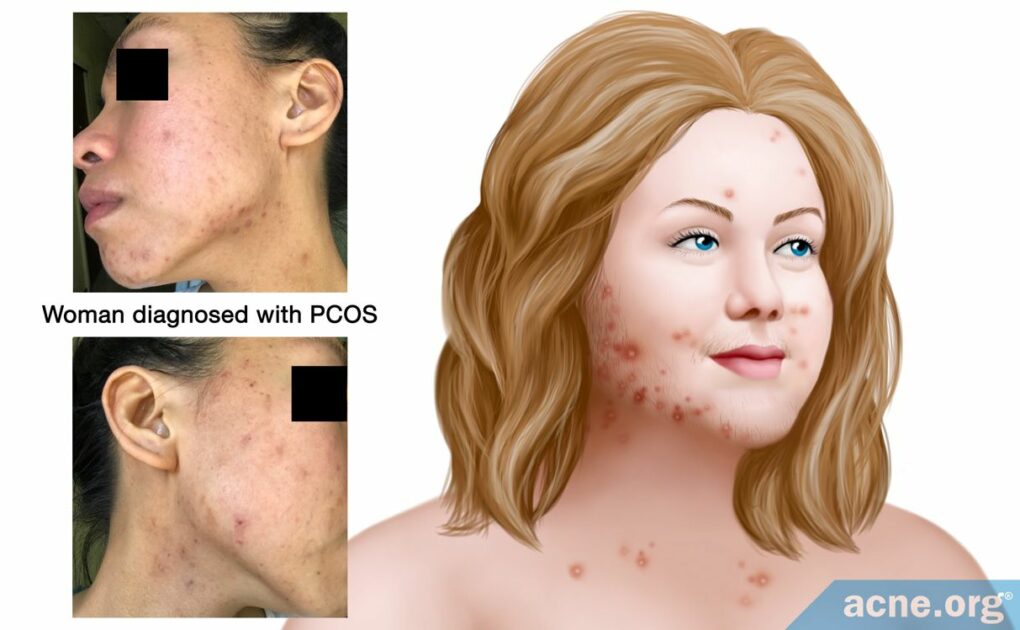
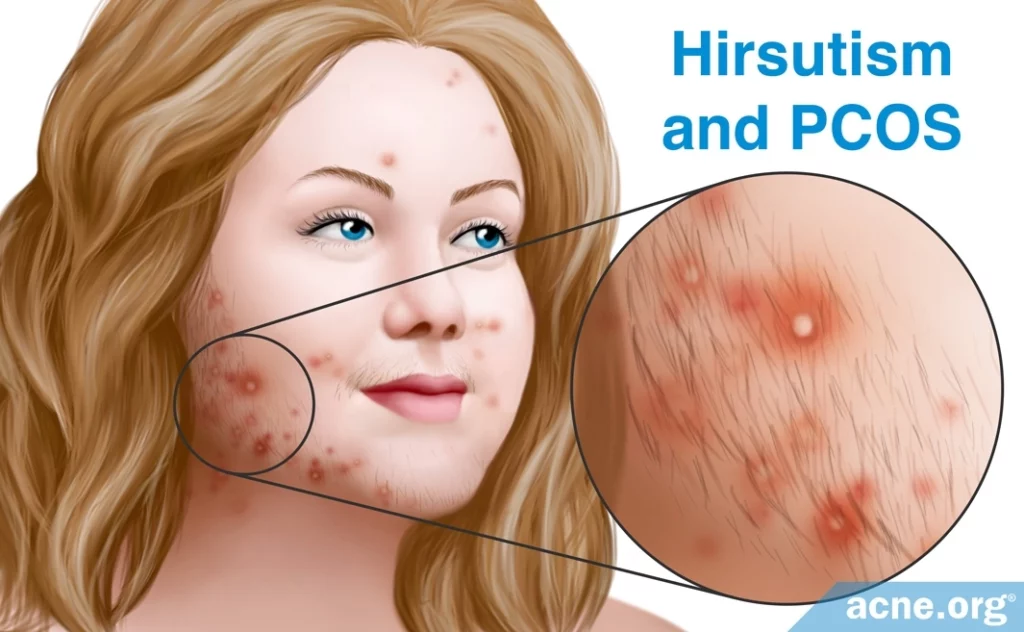
Acne + Excessive Hair Growth: Because high male hormone levels in the body tend to produce acne, females with PCOS very often struggle with acne. Acne associated with PCOS is more inflamed (red and sore) and appears on a larger portion of the body than normal acne that appears during puberty. Another common symptom of elevated male hormone levels is excessive hair growth, and many females with PCOS also experience unwanted hair growth.
When It Appears: Polycystic ovary syndrome often first appears in adolescence, making diagnosis difficult because the symptoms overlap with normal symptoms of puberty, such as acne.
How It Is Treated: The most common treatment for PCOS-associated acne is a combined oral contraceptives (COCs – a.k.a. the birth control pill), which reduce male hormone levels, helping to treat PCOS as well as the acne associated with it. For women whose medical history puts them at increased risk of side effects from COCs, a few non-hormonal treatments are also available.
Important: Polycystic ovary syndrome is common, so don’t discount it as something rare that you probably don’t have. If you are a female with moderate-to-severe acne on the face and/or body, particularly if you notice irregular periods and/or excessive hair growth, or if you are a female with acne that has persisted into adulthood that doesn’t respond to typical acne medications, make sure to see a dermatologist to be evaluated for PCOS. Left untreated, PCOS can impair fertility.

The Science
- What Is PCOS?
- Symptoms
- Hormonal Fluctuations in PCOS
- Diagnosis
- How Is PCOS Related to Acne?
- What PCOS Medications Can Be Used to Treat Acne?
- Non-hormonal Treatment Options for Women with PCOS
- Bottom Line
What Is PCOS?
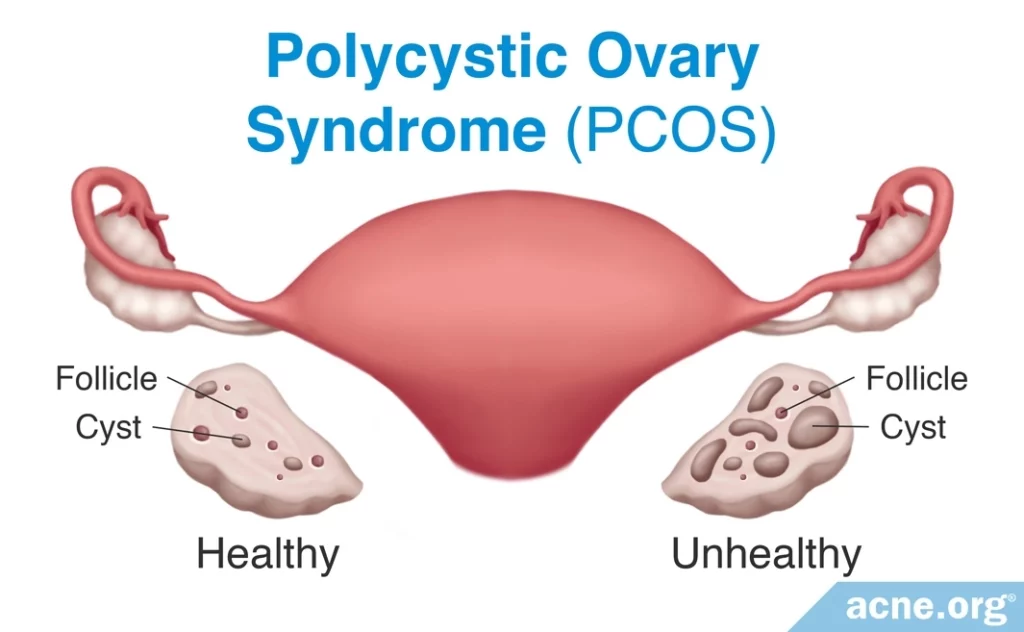
Polycystic ovary syndrome (PCOS) is a common hormonal disorder that affects adolescent girls and adult women. It is characterized by:
- Polycystic ovaries, which means that the ovaries possess an abnormally high number of cysts. Cysts in ovaries are not always problematic, as healthy ovaries sometimes have a few cysts.1
- Dysfunctional ovulation, meaning that the ovaries produce eggs on an irregular schedule
- High levels of androgens (male hormones found in both males and females)
Symptoms
The increase in androgens causes symptoms such as:
- Acne

- Hirsutism: Excessive hair that grows in a male pattern, such as on the chest and face
- Irregular periods: Periods that occur either more often than usual or less often than usual. Not all women with PCOS experience irregular periods.
- Obesity: Especially abdominal obesity

- Insulin resistance: This is when the body does not respond to the hormone, insulin, normally. In PCOS, insulin resistance causes the body to produce even more insulin, which can result in too much insulin in the bloodstream.1
Hormonal Fluctuations in PCOS
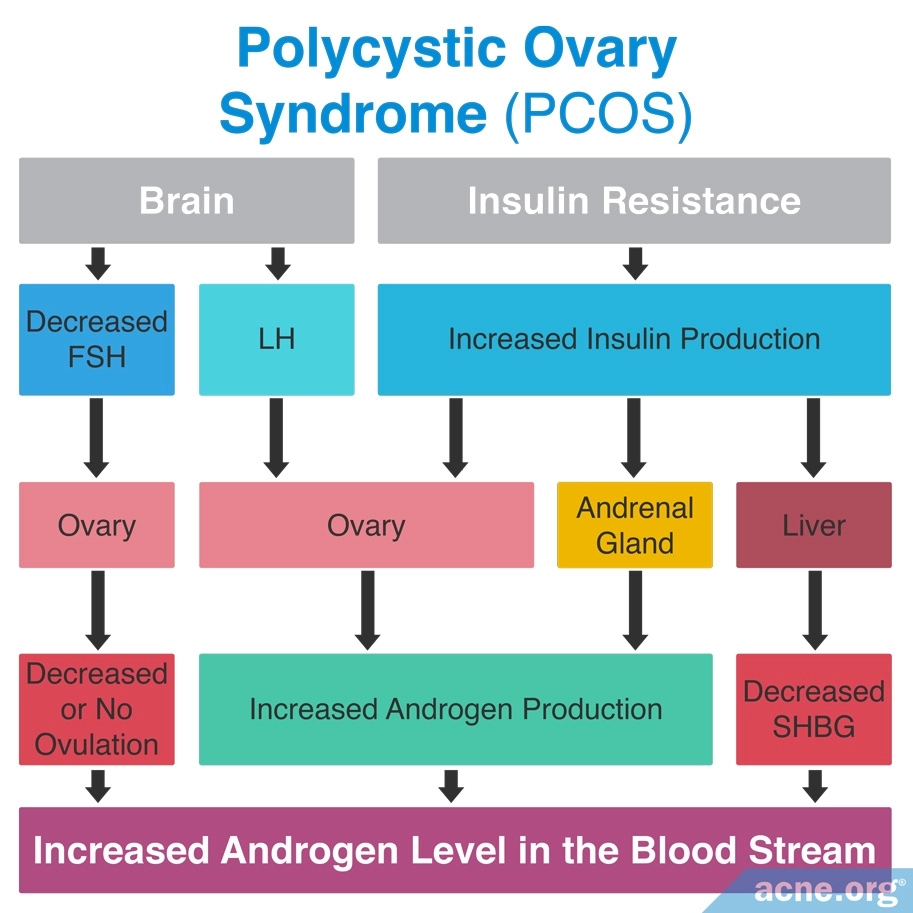
The high level of androgens in PCOS is part of a chain reaction involving several different hormones. The final result is an increase in androgens, and very often, acne.
- The body produces too much of a hormone called luteinizing hormone (LH). Too much LH causes the ovaries to produce excessive amounts of androgens.
- At the same time, too little of a hormone called follicle-stimulating hormone (FSH) causes dysfunctional ovulation.
- Finally, too much insulin in the bloodstream also stimulates the ovaries to produce more androgens. Excess insulin also increases androgens by reducing the levels of another hormone called sex hormone-binding globulin (SHBG), which normally keeps androgen levels from rising too high.1
This graphic illustrates the chain reaction:
Diagnosis
Polycystic ovary syndrome often appears during adolescence. However, diagnosing it in adolescents is difficult because symptoms such as irregular menstruation and acne are often a normal part of puberty. Because of this, PCOS is most frequently diagnosed between the ages of 25 and 35 and is much less frequently diagnosed before age 20. Because there are no tests that can diagnose PCOS, it is a diagnosis of exclusion, meaning that it is diagnosed after ruling out all other possible conditions.1,2
As we have stated, because PCOS symptoms such as irregular menstruation and acne overlap with normal puberty symptoms, they are not reliable indicators of PCOS. During the teen years, the most reliable symptoms that indicate PCOS are:
- The presence of high levels of androgens in the blood
- A persistent pattern of irregular periods that lasts for at least two years after the onset of menstruation
- Ovaries that have at least 25 cysts3
For females of any age, the following symptoms should raise suspicion of PCOS:
- Acne and hirsutism, especially when they accompany irregular periods or polycystic ovaries
- Obesity, especially obesity that is located in the belly. In PCOS, obesity is a result of hormone imbalances that cause weight gain.4
How Is PCOS Related to Acne?
As we have seen, PCOS comes with increased androgen levels. Androgens stimulate the skin to produce more skin oil, called sebum. Excess sebum greatly increases the chance of developing acne.5
Interestingly, PCOS-related acne tends to be different from normal acne that appears during puberty.
- Pubertal acne involves non-inflammatory lesions, such as whiteheads, and inflammatory lesions, such as pustules. In addition, pubertal acne in females appears mostly on the face.
- PCOS-related acne appears mostly as inflammatory lesions on the lower face, but also on the neck, chest, and upper back.5
Moderate-to-severe acne in all women is an indicator of PCOS.

According to a 2014 review in the Journal of the American Academy of Dermatology, “Women with moderate to severe acne should be investigated for PCOS, because 19% to 37% of [female] patients with moderate to severe acne meet the criteria for this disorder.”5 This review also recommends that women with acne that persists into adulthood and does not respond to traditional acne treatment be examined for PCOS.5
What PCOS Medications Can Be Used to Treat Acne?
Different medications are available to treat the various symptoms of PCOS. Since androgens lead to the acne that appears as a symptom of PCOS, treatment of PCOS-related acne aims to reduce androgen levels.
The most commonly used medications for PCOS-associated acne are:
- Combined oral contraceptives (COCs), also known as the birth control pill
- Cyproterone acetate (CPA)
- Spironolactone
- Flutamide
- Finasteride
Let’s take a look at each of these medication options.
Combined Oral Contraceptives
Combined oral contraceptives are birth control pills that contain a combination of ethinyl estradiol (synthetic estrogen, a female hormone that is present in both males and females) and a progestin (synthetic progesterone, another hormone that is present in both males and females).5
Different COCs contain different progestins. While all COCs reduce androgen levels, certain progestins, such as cyproterone acetate (CPA), drospirenone, and chlormadinone acetate (CMA), possess specific anti-androgen properties. Some research suggests that these progestins are somewhat more effective in treating acne than COCs that contain progestins without these properties. However, many studies show that all COCs are effective in reducing androgen levels and clearing acne.3,4
Numerous studies investigated the efficacy of COCs in women with PCOS-associated acne and have all found a significant improvement in acne in the women studied. We can conclude from these studies that all COCs work equally well in treating acne but that COCs that contain an anti-androgen progestin, such as CPA or drospirenone, may be more effective for treating acne accompanied by other androgen-related symptoms, such as hirsutism. Based on these studies, women with PCOS-related acne who use a COC can expect a 50% – 87% improvement in their acne, though some women’s acne may clear completely.6-14
Side effects of COCs include nausea, headache, and breast pain, but COCs can also raise the risk of some more severe health problems, such as heart disease and thromboembolism (blood clot).
Expand to read details of studies on birth control pills
A 1997 study in the Journal of Obstetrics and Gynaecology examined the effectiveness of a COC that contained CPA. This study included 82 women with PCOS and moderate to severe acne. The authors found that after 18 4-week cycles of the COC, acne cleared in 87% of the women, and after 24 cycles, acne cleared in all 82 women.6
A small 2004 pilot study in the Journal of Family Planning and Reproductive Health Care looked at the effectiveness of a COC containing drospirenone in 13 women with PCOS-associated acne. This study found a significant improvement in acne after six months of treatment.7
A 2010 study in the journal Contraception compared the effectiveness of a COC containing drospirenone with a COC containing desogestrel, which does not have specific anti-androgen properties, in 60 women with PCOS. This study found that of the women who had acne, 50% of those who took the COC containing drospirenone experienced improvement in their acne, compared to 30% of those who took the COC containing desogestrel. The authors did not mention the effectiveness of the two medications, but they did state that there was no clinical difference in how the women’s acne responded to them.8
Another 2010 study in Contraception compared the effectiveness of a COC containing CMA in 15 women with PCOS to 15 women who received no COC treatment. The women who received the COC treatment experienced significantly more improvement in their acne after six months than the women who received no COC.9

A 2012 study in the Journal of the European Academy of Dermatology and Venereology compared the effectiveness of two COCs that each contained an anti-androgen progestin: one with drospirenone and one with CMA. This study included 59 women with mild to severe acne and PCOS, who randomly were assigned to one of the two COCs for six months. Both groups experienced a significant reduction in acne: the drospirenone group experienced a 71% reduction, and the CMA group experienced a 65% reduction.10
Another 2012 study, published in the Journal of Obstetrics and Gynaecology Research, investigated the effectiveness of a COC containing desogestrel in 42 women with PCOS. After 12 months of treatment, the percentage of women with acne decreased from 54% to 18%.11
A 2014 study in Archives of Gynecology and Obstetrics randomly assigned 52 women with PCOS to take a COC containing either CPA or drospirenone for 12 months. Acne improved by 50% in the CPA group and by 66% in the drospirenone group, though the difference between the two was not statistically significant.12
Another 2014 study, in Fertility and Sterility, compared three different COCs: one containing desogestrel, one containing CPA, and one containing drospirenone. This study included 171 women with PCOS. Acne decreased in all three groups after 12 months of treatment, with no significant difference between the three COCs. However, the authors concluded that when they considered androgen-specific symptoms, such as hirsutism, in addition to acne, CPA showed the strongest anti-androgen activity.13

A 2016 study in Gynecological Endocrinology evaluated the effectiveness of a COC containing CPA in 41 women with PCOS. This study found that acne improved by 87% in only three months.14
Cyproterone Acetate (CPA)
While doctors almost always prescribe cyproterone acetate (CPA) with a combined oral contraceptive (COC), in rare cases it is sometimes prescribed on its own. Because CPA is anti-androgen, it can cause birth defects in a male fetus. This means that women taking CPA alone must also use some form of birth control.
The recommended dose of CPA when used alone is 50 – 100 mg/day for a 10-day cycle.
In contrast, most COCs containing CPA have about only 2 mg of CPA.
Side effects include headache, weight gain, breast tenderness, loss of libido (sex drive), and mood changes. In high doses, CPA also can cause liver damage.4
Because CPA rarely is used alone, there is not much research concerning its efficacy for PCOS-related acne. One small 1987 study found that acne improved significantly after two months of solo CPA therapy. However, when the treatment was stopped, acne returned quickly. In addition, the women using CPA experienced either irregular menstruation or a complete cessation of their periods.15
Spironolactone

Spironolactone is an anti-androgen that is usually prescribed as an additional medication along with a COC. Because spironolactone is an anti-androgen, it can cause birth defects in a male fetus, so using birth control while taking it is required.1
The typical dosage of spironolactone is between 50 – 200 mg per day, with the most common (“preferred”) dose being 100 mg/day. Side effects, especially in higher doses, include breast tenderness, irregular periods, and headache, among others.4
The preponderance of the evidence seems to be pointing to spironolactone on its own being somewhat helpful for PCOS-related acne, although not as helpful as COCs. At the same time, spironolactone appears to cause less side effects than COCs, potentially making it a safer choice for certain patients, such as females at risk of cardiovascular complications.16-18
Expand to read details of research on spironolactone

A recent systematic review (a rigorous literature review that provides the highest level of evidence) published in the journal Cureus in 2022 compared how well spironolactone and COCs treated various PCOS symptoms, including acne. The review authors examined 9 studies and concluded that spironolactone was less effective than COCs at reducing acne and other PCOS symptoms. On the plus side, they found that spironolactone caused less side effects than COCs and was a safer alternative for patients with cardiovascular disease.18
Flutamide
Flutamide is another anti-androgen that can be prescribed on its own or with a COC. Again, because it can cause birth defects in a male fetus, women taking it must also use birth control.3
Sometimes doctors incorporate flutamide if a COC alone is not enough to resolve PCOS symptoms. Low doses of flutamide (less than or equal to 250 mg/day) are generally better tolerated, with less side effects. Since low doses are as effective as higher doses, and high doses can damage the liver, researchers recommend staying with a low dose.3
There is only one small study evaluating the effectiveness of flutamide on its own in women with acne, and results showed that it did in fact work to clear acne. One study evaluating the effectiveness of flutamide with a COC also found a dramatic clearing of acne.19-21
Expand to read details of studies on flutamide

Researchers in a small 1993 study in Clinical Endocrinology gave 10 women with hirsutism 250mg of flutamide twice per day for one year. Five of these women also had acne, and 5 did not. This study found that the 5 women with acne experienced a dramatic reduction in their acne within the first month of treatment. After 2 months, their acne cleared. None of the women experienced any significant side effects. It is important to keep in mind, though, that the study was small, so we shouldn’t conclude anything.19
A 2007 study in the Journal of Clinical Endocrinology and Metabolism examined the effectiveness of 3 doses of flutamide (125mg, 250mg, and 375mg) combined with a COC and compared it to a placebo. This study included 131 women with hirsutism and acne. After 12 months of treatment, the women using flutamide with a COC experienced a reduction of more than 80% in their acne. The women in the placebo group experienced only a 46.4% reduction. The authors found that while all doses of flutamide worked better than placebo, higher doses were not more effective than lower ones.20

A 2010 study in Gynecological Endocrinology investigated the long-term effects of flutamide in women with acne who had not been diagnosed with PCOS and did not have hirsutism. This study found that low doses of flutamide (between 62.5 and 125 mg/day) did not affect liver function. This study looked only at side effects of flutamide and did not indicate what effect it had on acne.21
Finasteride

Finasteride is not an anti-androgen, but it prevents testosterone (an androgen) from being converted to its more active form. It is commonly known by its brand name Propecia®, used to treat hair loss in men. Its effectiveness at the recommended dose of 5 mg/day is similar to that of anti-androgens.4
Recently, a team of researchers combed through 65 studies on finasteride, and found only 2 studies looking at finasteride as a treatment for PCOS-related acne. Based on these studies, the researchers concluded that finasteride can improve acne in women, but less effectively than flutamide or a CPA-containing oral contraceptive.22 However, when it comes to PCOS-related hirsutism, finasteride is about as effective as flutamide, spironolactone, and CPA-containing oral contraceptives.22-24
Side effects in women include increased hair growth, sweating, and hot flashes. Finasteride also carries a high risk of causing birth defects in a male fetus, so women who are pregnant or may become pregnant should not take this medication.
Expand to read details of research on finasteride
This systematic review was published in the International Journal of Dermatology in 2019. The researchers looked at 65 studies that included a total of 2,683 female patients treated with finasteride. Most of the studies tested finasteride as a treatment for women with hirsutism or female pattern hair loss, and only 2 studies tested finasteride on women with acne. After reviewing the research, the review authors came to the following conclusions:
- For PCOS-related acne: Finasteride is less effective than flutamide or a CPA-ethinyl estradiol combination.
- For PCOS-related hirsutism: Finasteride is as effective as flutamide, spironolactone, and a CPA-ethinyl estradiol combination.22
Non-hormonal Treatment Options for Women with PCOS
Some women with PCOS are poor candidates for hormonal treatments like COCs. Because of the increased risk of side effects, doctors are reluctant to prescribe COCs to women who are:
- At risk for forming blood clots (thrombophilia)
- Prone to migraines
- Heavy smokers25
For these women, non-hormonal prescription treatments such as isotretinoin and metformin may be a useful alternative. In addition, researchers are looking into potential new over-the-counter treatments like myo-inositol.
Isotretinoin
For women with PCOS and severe, deeply scarring acne, isotretinoin (Accutane®) may be an option. One study looked at forty women with PCOS and severe acne who were unable to take COCs. The researchers found that a six-month course of treatment with isotretinoin improved not only acne, but other PCOS symptoms, such as hirsutism and androgen levels in the blood.25
However, any time we mention isotretinoin, we must also mention its side effects, some of which may be lifelong. And particularly, we must strongly mention its propensity to cause severe birth defects and miscarriage. Isotretinoin is the #1 most birth defect-causing medication on the market. It must be considered carefully alongside a trusted physician, and must be administered only when two (2) forms of birth control are in place.
Expand to read details of study

A study published in the journal BioMed Research International in 2019 looked at the efficacy of isotretinoin treatment in women with PCOS and severe cystic acne. Forty women between the ages of 18 and 40 participated in the study. The women were unable to take COCs due to heavy smoking, a history of blood clots or migraines, and/or a fear of taking hormonal pills. The researchers treated the women with oral isotretinoin taken daily for 6 months.
Before starting the treatment and at the end of the treatment, the scientists evaluated the women’s acne and hirsutism and measured the amounts of testosterone and insulin in their blood. They found that 6 months of oral isotretinoin significantly improved acne and hirsutism and decreased the amounts of testosterone and insulin in the blood. These results indicate an improvement in PCOS symptoms. The researchers wrote, “Solely isotretinoin administration may supply adequate healing in PCOS patients’ symptoms complicated with severe cystic acne who [are] not eligible candidates for [oral contraceptive pill] use.”25
Metformin
Metformin is a medication used to treat diabetes by lowering sugar levels and insulin levels in the blood. This in turn can help reduce androgen levels.
In 2021, a group of researchers reviewed 51 studies on metformin as a treatment for PCOS-related acne. The researchers found metformin to be effective at improving acne in patients with PCOS, either as a stand-alone treatment or in combination with other treatments like oral contraceptives.26
Expand to read details of research

A systematic review published in in the American Journal of Clinical Dermatology in 2021 explored the evidence on metformin for treating acne in patients with PCOS. After reviewing 51 studies, the researchers concluded that taking metformin for 3 months or more can significantly improve PCOS-related acne. They also found that metformin works better in combination with oral contraceptives than on its own.26 However, because the patients in different studies took different doses of metformin over different lengths of time, more tightly controlled studies are needed to determine what dosage and length of treatment works best for PCOS-related acne.

For instance, one study published in The Journal of Clinical and Aesthetic Dermatology in 2019 tested metformin taken at a dose of 500 mg 3 times a day for 8 weeks on 40 women with PCOS. The researchers found that this treatment regimen improved acne by 47% after 3 weeks, by 64% after 6 weeks, and by 86% after 8 weeks.27
Myo-inositol: An experimental treatment that shows some promise
Myo-inositol is a compound related to vitamin B that is naturally found in the body. One study found that a pill called Tracnil™, which contains myo-inositol combined with folic acid and vitamin D3, improved acne in women with PCOS symptoms.28 However, this is just one preliminary study, so more research into this potential treatment is necessary.
Expand to read details of study

The study was published in the journal Dermatology Research and Practice in 2020. Thirty-three women with symptoms of PCOS, such as acne, hirsutism, and irregular menstrual periods, participated in the study. The researchers noted that the women, despite experiencing symptoms of PCOS, had normal hormone levels. The women took Tracnil™, a pill containing myo-inositol, folic acid, and vitamin D3, twice a day for 6 months.28
The researchers found that 3 months of treatment with the myo-inositol pill reduced acne lesions by almost 50%. Other PCOS symptoms, such as hirsutism and irregular periods, also began to improve significantly after 8 weeks of treatment. However, the scientists noted the limitations of the study, including its small size and the lack of a control group.28 In other words, a larger study comparing the efficacy of Tracnil™ against a placebo pill (a similar-looking pill without medicinal ingredients) is necessary. Also, since Tracnil™ contains folic acid and vitamin D in addition to myo-inositol, it is impossible to say how much of the medicinal effect is due to myo-inositol itself. For example, vitamin D may have been responsible for some of the drug’s anti-acne effect.
Bottom Line
If you are a female who is struggling with acne, particularly acne on both your face and body, and you are also experiencing excessive hair growth, weight gain, or menstrual irregularities, be sure to ask your doctor about the possibility of PCOS. It is very common and treatable.
References
- McCartney, C. R. & Marshall, J. C. Polycystic ovary syndrome. N. Engl. J. Med. 375, 54 – 64 (2016). https://www.ncbi.nlm.nih.gov/pubmed/27705264
- Lo, J. C. et al. Epidemiology and adverse cardiovascular risk profile of diagnosed polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 91, 1357 – 1363 (2006). https://www.ncbi.nlm.nih.gov/pubmed/16434451
- Spritzer, P. M. & Motta, A. B. Adolescence and polycystic ovary syndrome: current concepts on diagnosis and treatment. Int. J. Clin. Pract. 69, 1236 – 1246 (2015). https://www.ncbi.nlm.nih.gov/pubmed/26289303
- Conway, G. et al. The polycystic ovary syndrome: a position statement from the European Society of Endocrinology. Eur. J. Endocrinol. 171, P1 – 19 (2014). https://www.ncbi.nlm.nih.gov/pubmed/24849517
- Housman, E. & Reynolds, R. V. Polycystic ovary syndrome: a review for dermatologists. J. Am. Acad. Dermatol. 71, e1 – 10 (2014). https://www.ncbi.nlm.nih.gov/pubmed/25437977
- Falsetti, L., Ramazzottto, F. & Rosina, B. Efficacy of combined ethinyl estradiol (0.035mg) and cyproterone acetate (2 mg) in acne and hirsutism in women with polycystic ovary syndrome. J. Obstet. Gynaecol. 17, 565 – 568 (1997). https://www.ncbi.nlm.nih.gov/pubmed/15511960
- Palep-Singh, M., Mook, K., Barth, J. & Balen, A. An observational study of Yasmin in the management of women with polycystic ovary syndrome. J. Fam. Plann. Reprod. Health Care 30, 163 – 165 (2004). https://www.ncbi.nlm.nih.gov/pubmed/15222920
- Kriplani, A. et al. Effect of oral contraceptive containing ethinyl estradiol combined with drospirenone vs. desogestrel on clinical and biochemical parameters in patients with polycystic ovary syndrome. Contraception 82, 139 – 146 (2010). https://www.ncbi.nlm.nih.gov/pubmed/20654754
- Uras, R. et al. Endocrinological, metabolic and clinical features of treatment with oral contraceptive formulation containing ethinylestradiol plus chlormadinone acetate in nonobese women with polycystic ovary syndrome. Contraception 82, 131 – 138 (2010). https://www.ncbi.nlm.nih.gov/pubmed/20654753
- Colonna, L. et al. Skin improvement with two different oestroprogestins in patients affects by acne and polycystic ovary syndrome: clinical and instrumental evaluation. J. Eur. Acad. Dermatol. Venereol. 26, 1364 – 1371 (2012). https://www.ncbi.nlm.nih.gov/pubmed/22011217
- Bhattacharya, S. M., Ghosh, M. & Basu, R. Effects of ethinyl estradiol and desogestrel on clinical and metabolic parameters in Indian patients with polycystic ovary syndrome. J. Obstet. Gynaecol. Res. 38, 285 – 290 (2012). https://www.ncbi.nlm.nih.gov/pubmed/22070369
- Kahraman, K. et al. Comparison of two oral contraceptive forms containing cyproterone acetate and drospirenone in the treatment of patients with polycystic ovary syndrome: a randomized clinical trial. Arch. Gynecol. Obstet. 290, 321 – 328 (2014). https://www.ncbi.nlm.nih.gov/pubmed/24676694
- Bhattacharya, S. M. & Jha, A. Comparative study of the therapeutic effects of oral contraceptive pills containing desogestrel, cyproterone acetate, and drospirenone in patients with polycystic ovary syndrome. Fertil. Steril. 98, 1053 – 1059 (2012). https://www.ncbi.nlm.nih.gov/pubmed/22795636
- Feng, W., Jia, Y. Y., Zhang, D. Y. & Shi, H. R. Management of polycystic ovarian syndrome with Diane-35 or Diane-35 plus metformin. Gynecol. Endocrinol. 32, 147 – 150 (2016). https://www.ncbi.nlm.nih.gov/pubmed/26507097
- Couzinet, B., Le Strat, N., Brailly, S. & Schaison, G. Comparative effects of cyproterone acetate or a long-lasting gonadotrophin-releasing hormone agonist in polycystic ovarian disease. J. Clin. Endocrinol. Metab. 63, 1031 – 1035 (1986). https://www.ncbi.nlm.nih.gov/pubmed/2943752
- Zulian, E. et al. Spironolactone in the treatment of polycystic ovary syndrome: efficacy on clinical features, insulin sensitivity and lipid profile. J. Endocrinol. Invest. 28, 49 – 53 (2005). https://www.ncbi.nlm.nih.gov/pubmed/15816371
- Brown, J., Farguhar, C., Lee, O., Toomath, R. & Jepson, R. G. Spironolactone versus placebo or in combination with steroids for hirsutism and/ or acne. Cochrane Database Syst. Rev. 15, CD00194 (2009). https://www.ncbi.nlm.nih.gov/pubmed/19370553
- Rajashekar, S., Giri Ravindran, S., Kakarla, M., et al. Spironolactone versus oral contraceptive pills in the treatment of adolescent polycystic ovarian syndrome: A systematic review. Cureus 14, e25340 (2022). https://pubmed.ncbi.nlm.nih.gov/35774693/
- Couzinet, B., Pholsena, M., Young, J. & Schaison, G. The impact of a pure anti-androgen (flutamide) on LH, FSH, androgens and clinical status in idiopathic hirsutism. Clin. Endocrol. (Oxd) 39, 157 – 162 (1993). https://www.ncbi.nlm.nih.gov/pubmed/8370128
- Calaf, J. et al. Long-term efficacy an tolerability of flutamide combined with oral contraception in moderate to severe hirsutism: a 12-month, double-blind, parallel clinical trial. J. Clin. Endocrinol. Metab. 92, 3446 – 3452 (2007). https://academic.oup.com/jcem/article/92/9/3446/2597495
- Paradisi, R. et al. Retrospective, observational study on the effects and tolerability of flutamide in a large population of patients with acne and seborrhea over a 15-year period. Gynecol. Endocrinol. 27, 823 – 829 (2011). https://www.tandfonline.com/doi/abs/10.3109/09513590.2010.526664?src=recsys&journalCode=igye20
- Hu, A. C., Chapman, L. W. & Mesinkovska, N. A. The efficacy and use of finasteride in women: a systematic review. Int. J. Dermatol. 58, 759-776 (2019). https://pubmed.ncbi.nlm.nih.gov/30604525/
- Moghetti, P. et al. Comparison of spironolactone, flutamide, and finasteride efficacy in the treatment of hirsutism: a randomized, double blind, placebo-controlled trial. J. Clin. Endocrinol. Metab. 85, 89 – 94 (2000). https://www.ncbi.nlm.nih.gov/pubmed/10634370
- Beigi, A., Sobhi, A. & Zarrinkoub, F. Finasteride versus cyproterone acetate-estrogen regimens in the treatment of hirsutism. Int. J. Gynaecol. Obstet. 87, 29 – 33 (2004). https://www.ncbi.nlm.nih.gov/pubmed/15464773
- Acmaz, G., Cınar, L., Acmaz, B., et al. The effects of oral isotretinoin in women with acne and polycystic ovary syndrome. Biomed. Res. Int. 2019, 2513067 (2019). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6475563/
- Yen, H., Chang, Y. T., Yee, F. J. & Huang, Y. C. Metformin therapy for acne in patients with polycystic ovary syndrome: A systematic review and meta-analysis. Am. J. Clin. Dermatol. 22, 11-23 (2021). https://pubmed.ncbi.nlm.nih.gov/33048332/
- Sharma, S., Mathur, D. K., Paliwal, V. & Bhargava, P. Efficacy of metformin in the treatment of acne in women with polycystic ovarian syndrome: A newer approach to acne therapy. J. Clin. Aesthet. Dermatol. 12, 34‐38 (2019). https://www.ncbi.nlm.nih.gov/pubmed/31320975
- Ramanan, E. A., Ravi, S., Anbu, K. R. R. & Michael, M. Efficacy and safety of Tracnil™ administration in patients with dermatological manifestations of PCOS: An open-label single-arm study. Dermatol. Res. Pract. 2020, 7019126 (2020). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7128037/
 Acne.org Products
Acne.org Products