Isotretinoin Is Not Safe for Breastfeeding Infants and Should Be Avoided

The Essential Info
Isotretinoin (Accutane®) is an oral medication sometimes prescribed for severe and scarring acne that does not respond to other treatments. It is a vitamin A derivative that is very well known to cause severe birth defects and miscarriage.
Isotretinoin’s chemical qualities lead biologists to believe it is likely to enter into the breast milk, and therefore isotretinoin is not safe for breastfeeding infants.
The Bottom Line: Both pregnant and breastfeeding women should avoid taking isotretinoin.

The Science
- Drug Transfer into Breast Milk
- Isotretinoin’s Transfer into Breast Milk
- Vitamin A and Beta-Carotene Entrance into Breast Milk
- The Bottom Line
The FDA classifies isotretinoin as a category X drug, meaning that research has proven that isotretinoin can cause fetal abnormalities in pregnant women or laboratory animals. In fact, isotretinoin is the most teratogenic (causes birth defects) medication on the market, and its effects on the fetus are widespread and severe, including death.1,2
For this reason, medical professionals do not prescribe isotretinoin for patients who are pregnant or are planning to become pregnant, and females who do take isotretinoin are required to use two (2) forms of birth control before starting and while taking the medication.
Due to ethical constraints, scientists have been unable to examine the potential dangers of taking isotretinoin while breastfeeding. However, the research into isotretinoin’s chemical qualities has concluded that it is very likely that when taken by a breastfeeding mother, isotretinoin can cross into the breast milk and harm the infant. Therefore, medical professionals do not recommend that breastfeeding mothers use isotretinoin.1
In addition, the medical literature reports on multiple patients who have experienced breast reactions to taking isotretinoin. Such reactions included an increase in breast size in men (gynecomastia) and spontaneous flow of milk from the breast in a man or non-breastfeeding woman (galactorrhea).3 Since isotretinoin impacts the breast, this indirectly strengthens the prediction that it may cross into breast milk.
Drug Transfer into Breast Milk
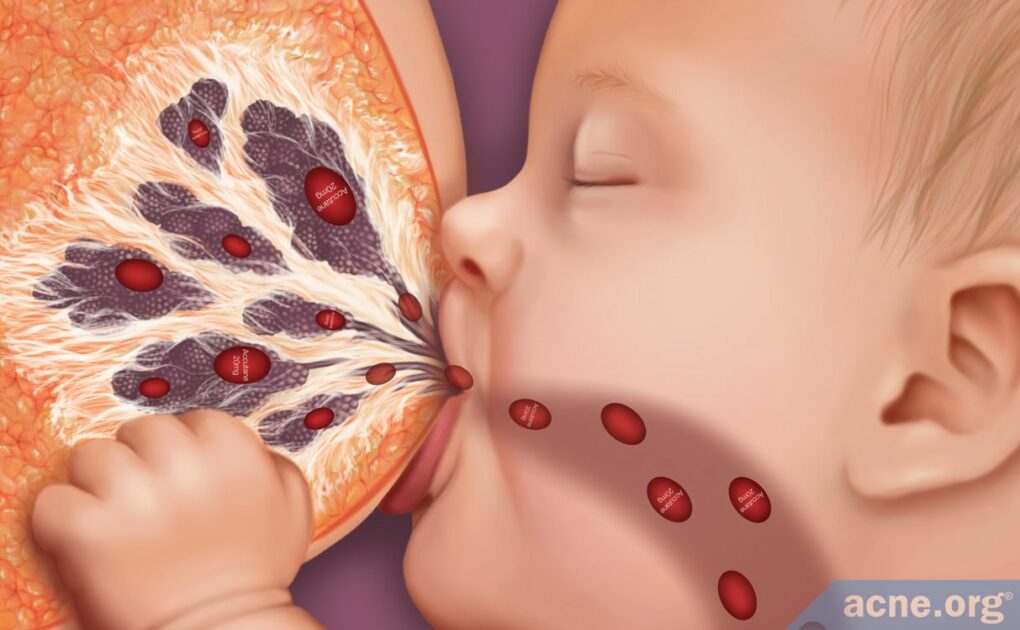
A breastfeeding mother’s body consistently takes proteins, nutrients, and antibodies from the bloodstream and transfers them into breast milk to nourish the feeding infant. When the breastfeeding mother takes oral medication, these drugs also make their way into the bloodstream and can occasionally be transferred into breast milk.
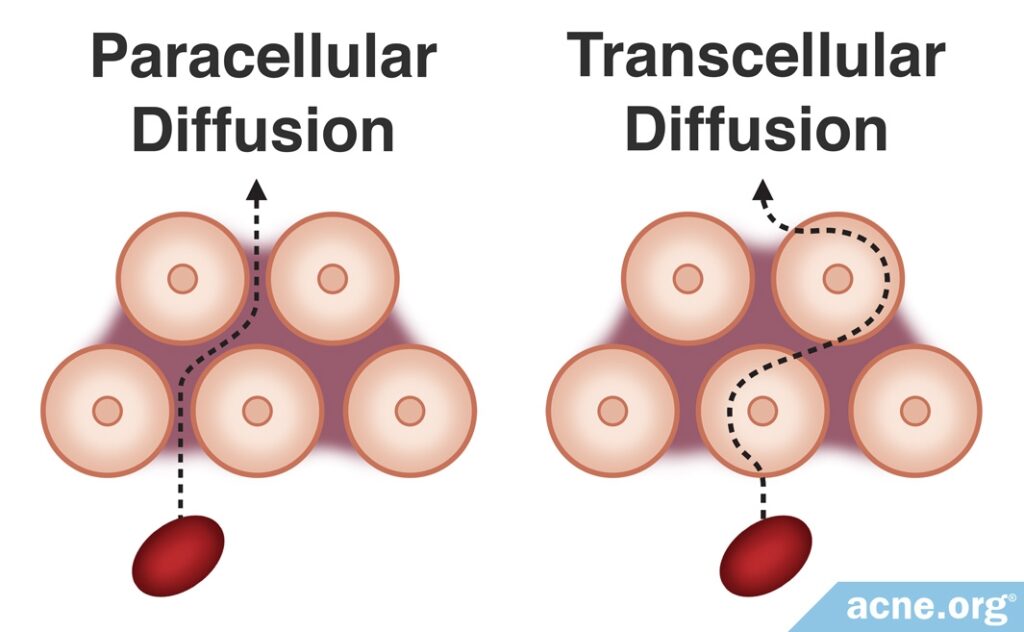
There are two methods of drug transfer into breast milk, and isotretinoin is likely to be able to transfer through either method:
- Paracellular diffusion occurs within the first three days after birth, when the drug moves from the blood stream into the breast milk through gaps between breast cells. Paracellular diffusion is a less restrictive drug transfer process than transcellular diffusion, allowing drugs to more easily pass through.
- Transcellular diffusion kicks in three days after birth, when the gaps between breast cells close and the drug must move through the breast cells themselves to reach the breast milk.
Regardless of whether it is the first three days after birth or after these three days have elapsed, medical professionals are extremely careful when it comes to prescribing drugs, like isotretinoin, that can be transferred from the bloodstream and into the breast milk through either paracellular or transcellular diffusion.4
Isotretinoin’s Transfer into Breast Milk
After paracellular diffusion ends and the body closes the gaps between breast cells that appear shortly after birth, the body then must use transcellular diffusion to move nutrients from the bloodstream into the breast milk. This process is highly selective, requiring nutrients to meet a variety of chemical qualities in order to pass through the breast cells and into the breast milk.
Unfortunately, drugs that have any of these chemical qualities may also be able to pass into the breast milk. When it comes to isotretinoin, it displays three of the six chemical characteristics that increase the risk that it will pass through breast cells, leading scientists to believe that it will, in fact, pass into breast milk.

Three Characteristics of Isotretinoin That Increase Risk of Entering Breast Milk
- Fat solubility: Nutrients and drugs that are chemically similar to fat can more easily cross into the breast cell and into the breast milk. Vitamin A is a fat-soluble molecule, and isotretinoin, being a vitamin A derivative, retains this quality. Therefore, it can likely easily cross into the breast milk.5
- Ability to enter the blood circulation (oral bioavailability): When creating oral medication, scientists must consider the ability of the drug to be absorbed by the bloodstream. This quality, called oral bioavailability, determines how much of the drug is present in the bloodstream, and therefore able to move into other bodily fluids like breast milk. Isotretinoin’s bioavailability is 83% when taken with a high fat meal. Therefore, this high bioavailability means that a large percentage of isotretinoin is present in the bloodstream and can move into breast milk.5,6
- Half-life: A drug’s half-life measures the amount of time it takes for the blood concentration to fall to half of the initial concentration. If a drug has a short half life (1-3 hours), and a mother waits a few hours after taking the drug to breastfeed, that means there will be less of the drug in the bloodstream by feeding time. The half-life of isotretinoin is 17-50 hours, therefore potentially exposing the infant to a high concentration of isotretinoin in the breast milk.7
Three Characteristics of Isotretinoin That Decrease Risk of Entering Breast Milk
- Molecular size: There are proteins on the surface of breast cells called pores that allow small molecules to easily pass into the cell. For a molecule to pass through these pores, it must be less than 200 kilodaltons. The size of isotretinoin is 300 kilodaltons. Therefore, isotretinoin cannot pass through breast cell pores. This does not mean it cannot pass into the breast cell in other ways, but it cannot pass through the pores.5
- Protein binding ability: Blood contains proteins which bind to drugs. The more proteins bind to a drug, the less that drug is able to transfer into breast milk. Nearly 100% of isotretinoin in the blood is bound to other blood proteins, therefore potentially limiting its transfer into breast milk.5
- Measure of drug acidity (pKa): Some drugs are more acidic, and some are less acidic. The acidity of a drug is measured through calculation of pKa. Highly acidic drugs (lower pKa) are less likely to enter into and remain in breast milk, while lower-acidity drugs (higher pKa) are more likely to enter into and remain in breast milk. Isotretinoin is a highly acidic drug with a low pKa of 5. Therefore, the pKa of isotretinoin suggests it is more likely to remain in the bloodstream than cross into the breast milk.8
A drug does not have to display all six characteristics for it to pass through the breast cell and into the breast milk. Isotretinoin meets only three of the six qualities, but scientists believe that isotretinoin’s fat solubility, oral bioavailability, and half-life likely gives it the ability to cross into breast milk.
Vitamin A and Beta-Carotene Entrance into Breast Milk
Since isotretinoin is a vitamin A derivative, we can look at research looking into vitamin A and beta-carotene supplementation in breastfeeding mothers to find some more clues.
Results of this research shows us that when breastfeeding mothers consume vitamin A or beta-carotene in an oral tablet, it results in an increase in the amount of vitamin A and beta-carotene present in the breast milk. Therefore, like the chemically similar vitamin A and beta-carotene, isotretinoin may also cross into breast milk and potentially cause harm to the breastfeeding infant.4,6,9-14
The Bottom Line
Doctors recommend that breastfeeding mothers do not take isotretinoin.15
Click here for more info on how to treat acne during pregnancy.
And click here for alternative treatments for acne during pregnancy.
References
- Briggs, G., Freeman, R. & Yaffe S. Drugs in Pregnancy and Lactation. Philadelphia: Lippincott Williams & Wilkins (2002). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4989726/
- Rawashdeh, N. Drugs Contraindicated in Pregnancy (2013). Retrieved May 14, 2016, from Drug Information Center. http://www.just.edu.jo/DIC/Manuals/Drugs contrandicated in pregnancy.pdf
- U.S. National Library of Medicine (2018). Drugs and Lactation Database. Retrieved November 11, 2020, from the National Center for Biology Information (NCBI). https://www.ncbi.nlm.nih.gov/books/NBK501634/
- Hale, T. & Illet, K. Drug Therapy and Breastfeeding. New York: The Parthenon Publishing Group (2002). https://www.cabdirect.org/cabdirect/abstract/20023063782
- Hale, T. Medications and Mother’s Milk. Amarillo, Texas: Pharmasoft Publishing (2000). https://www.springerpub.com/hale-s-medications-mothers-milktm-2019-9780826135582.html
- U.S. National Library of Medicine (2016). Drugs and Lactation Database. Retrieved 05 14, 2016, from Toxicology Data Network (TOXNET). http://toxnet.nlm.nih.gov/newtoxnet/lactmed.htm
- Hale, T. Drug Entry Into Human Milk (2016). Retrieved May 12, 2016, from Infant Risk Center (Texas Tech University Health Sciences Center). http://www.infantrisk.com/content/drug-entry-human-milk
- Drug Bank. (2005, June 13). Isotretinoin. Retrieved May 14, 2016, from Drug Bank. http://www.drugbank.ca/drugs/DB00982
- Bennett, P. Drugs and Human Lactation. New York: Elsevier (1996). https://www.elsevier.com/books/drugs-and-human-lactation/bennett/978-0-444-81981-9
- Canfield, L. et al. Beta-carotene in breast milk and serum is Increased after a single beta-carotene dose. Am. J. Clin. Nutr. 66, 52-61 (1997). https://www.ncbi.nlm.nih.gov/pubmed/9209169
- Johnson E, Qin J, Krinsky N, & Russell R. Beta-carotene isomers in human isomer in human serum, breast milk, and buccal mucosa cells after continuous oral doses of all-trans and 9-cis-beta-carotene. J. Nutr. 127, 1993-1999 (1997). https://www.ncbi.nlm.nih.gov/pubmed/9311956
- Lawrence, R. A. & Lawrence R. M. Breastfeeding: A Guide for Medical Profession, 7th ed. Mosby: Maryland Heights (2011). http://iums.ac.ir/files/vch/files/laranc.pdf
- Ostrea, E., Balun, J., Winkler, R. & Porter, T. Influence of breast-feeding on the restoration of the low serum concentration of vitamin E and beta-carotene in the newborn infant. Am. J. Obst. Gynecol. 154, 1014-1017 (1986). https://www.sciencedirect.com/science/article/abs/pii/0002937886907404
- Thompson, M. Carotinaemia in a suckling. Arch. Dis. Child. 18, 112 (1943). https://www.ncbi.nlm.nih.gov/pubmed/21032250
- Ly, S., Kamal, K., Manjaly, P., Barbieri, J. S. & Mostaghimi, A. Treatment of acne vulgaris during pregnancy and lactation: A narrative review. Dermatol. Ther. (Heidelb). 13, 115-130 (2023). https://pubmed.ncbi.nlm.nih.gov/36447117/
 Acne.org Products
Acne.org Products