Pustules Are Slightly Elevated, Red Acne Lesions with a White/Yellow Center and Contain Pus

The Essential Info
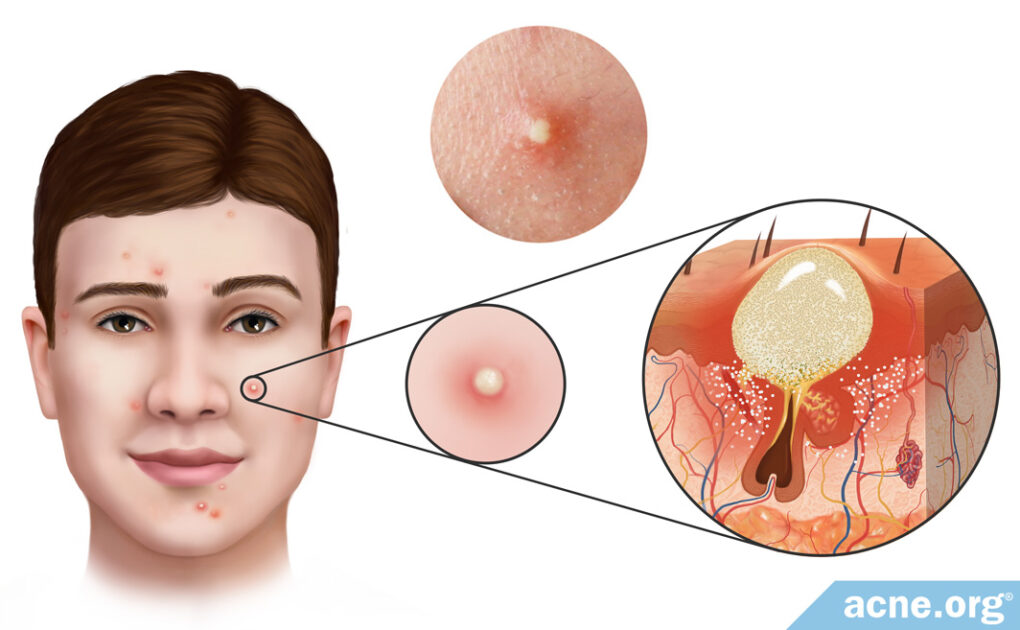
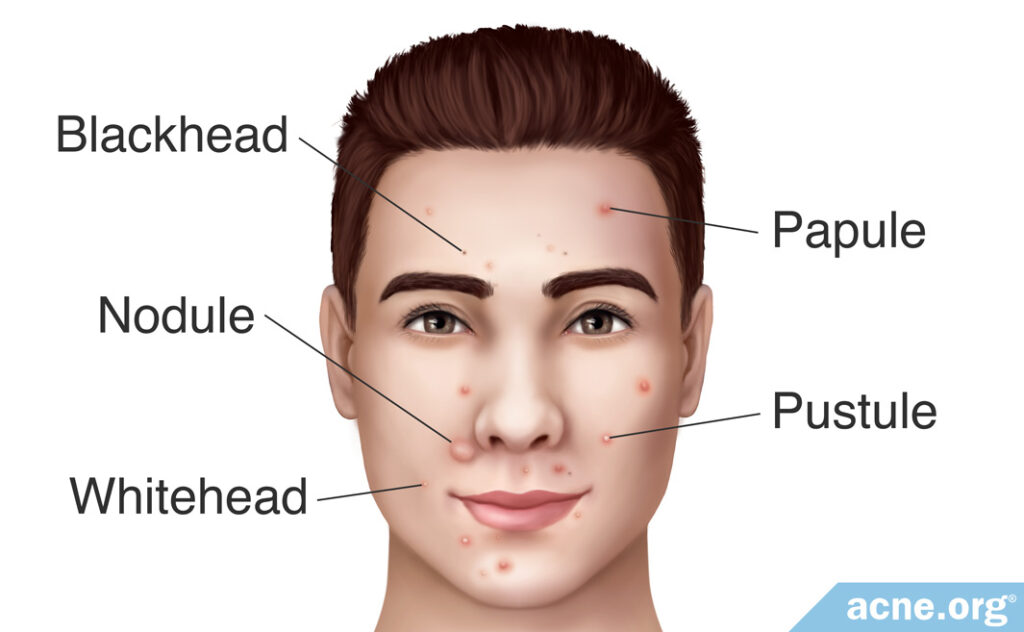
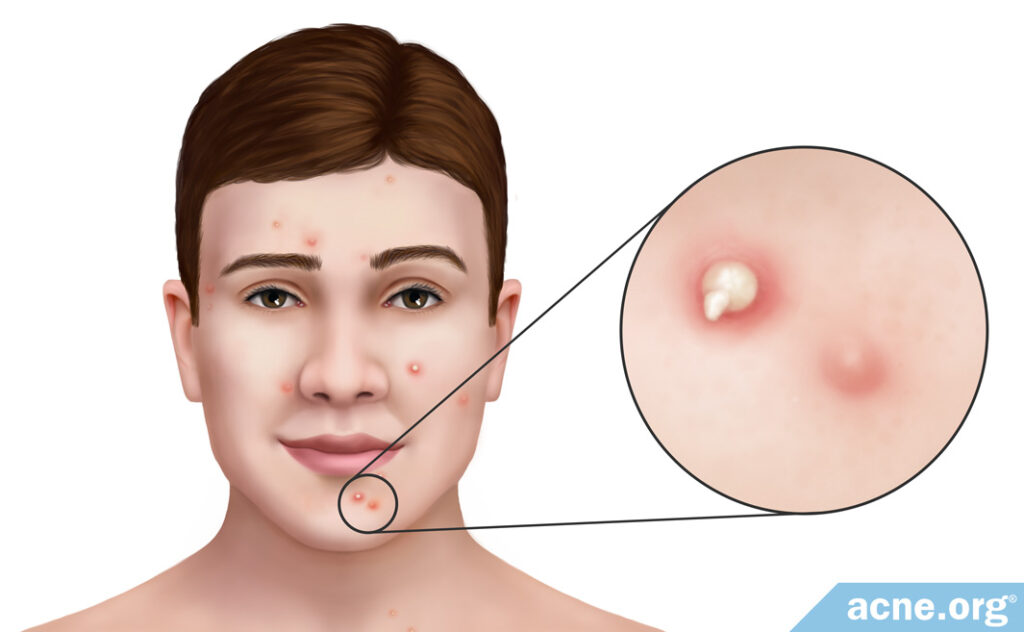
Pustules are what people normally refer to as “zits.” They are relatively small (less than 5 mm across), inflamed (red), elevated acne lesions with a white or yellow center that are located mainly on the face, neck, back, shoulders, and upper arms.
They develop when a pore becomes clogged, and skin oil that normally drains to the surface becomes trapped. Bacteria then grows inside the trapped skin oil, and the lesion becomes a red, sore, raised lesion called a papule. When the papule fills with pus and gets a white or yellow head, it is then called a pustule.
If left untouched, pustules remain on the skin for a few days, after which either the head of the pustule ruptures and releases the pus onto the surface of the skin or the body absorbs the pus.
Popping a Pustule: Pustules can also be popped once they are ready. Just make sure to pop them responsibly.

The Science
Pustules are small, slightly elevated, red, sore bumps with a white or yellow pus-filled center, commonly found on the face, neck, back, chest, shoulders, and upper arms. They are commonly known as “pimples” or “zits.”
After a couple of days on the skin, a pustule will either rupture and release its pus or the body will absorb the pus and the healing process will begin. Depending on genetic predisposition for scarring, pustules may or may not leave scars.1
Pustules are common among teenagers and young adults but can also occur in people over the age of 25.
How Pustules Develop
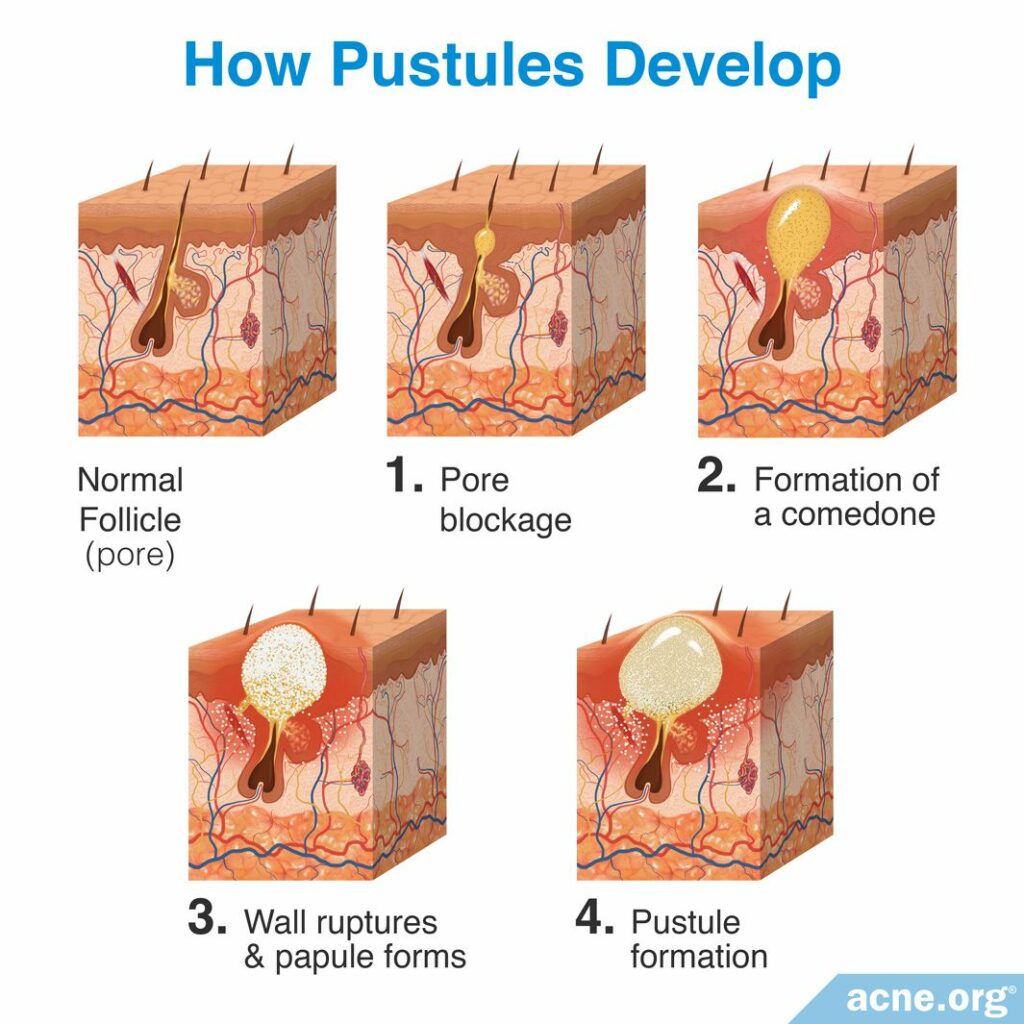
Pustules develop in four steps:
Step 1 – Pore blockage: Acne development begins with microscopic hair follicles (pores) in the skin. Attached to these pores are glands called sebaceous glands, which produce skin oil (sebum). Normally, the sebum flows freely up the pore and is released onto the surface of the skin. Acne develops when the opening of a pore becomes blocked, and this blockage results in sebum buildup inside the pore.
Step 2 – Formation of a comedone: After the pore is blocked and sebum begins to build up inside the pore, it becomes a visible lesion called a comedone, better known as a whitehead or blackhead.2,3
Step 3 – Wall ruptures & papule forms: Inside of a comedone, there is a buildup of sebum. This is the ideal environment for acne bacteria, called Cutibacterium acnes (C. acnes). This bacteria feeds on the trapped sebum and begins to reproduce rapidly. As the quantity of bacteria grows, the body views it as an infection and responds by sending in inflammatory cells to fight the infection. These inflammatory cells can weaken the wall of the pore, and eventually cause the pore to rupture. When the pore ruptures, the pore’s contents (sebum, C. acnes, inflammatory cells, and dead skin cells) are released into the surrounding skin. The body views these contents as “invaders” and responds with a larger inflammatory response that creates an inflamed, red, firm, slightly raised and sore acne lesion called a papule.4-6
Step 4 – Pustule formation: Normally, a papule fills with pus. At that point it becomes a pustule, which is softer to the touch than a papule. The pus that eventually fills the lesion is the result of the “battle” between C. acnes and inflammatory cells, both of which are killed during the battle, and the result of this death is pus. Pus is a white or yellow liquid that is made of dead inflammatory cells (white blood cells), along with serum (protein-rich liquid). The white blood cells give pus its characteristic white/yellow color.6,7
How Long Do Pustules Remain on the Skin?
Once a pustule has formed, it can remain on the skin for several days. Researchers have found that how a pustule develops can determine how long it will last.

A 1974 study published in the Journal of Investigative Dermatology found that pustules developing from blackheads remained on the skin for an average of 5.2 days, while pustules developing from whiteheads remained on the skin for an average of 8.2 days. After this time, the head of the pustule with either break spontaneously, or it will break through picking or popping the lesion. Once the head of the pustule breaks, the lesion releases the pus and other contents of the pore onto the surface of the skin. The lesion then heals, usually with minimal scarring.8,9
Treating Pustules
Once a pustule has formed, there’s not much you can do to reverse its course. Prevention is preferred. Pustules can be prevented with proven topical treatments, such as proper application of benzoyl peroxide. A variety of other remedies are also available. Some of these are sold over-the-counter, while others require a prescription from a doctor.10,11
Popping Pustules
If you wish to pop a pustule, wait until it has an obvious white or yellow center. Then, make sure you follow these instructions to make sure you do is safely.
References
- Bhate, K. & Williams C. Epidemiology of acne vulgaris. Br. J. Dermatol 168, 474 – 485 (2013). https://www.ncbi.nlm.nih.gov/pubmed/23210645
- Brogden, R. & Goa, K. Adapalene. Drugs 53, 511 – 519 (1997). https://www.ncbi.nlm.nih.gov/pubmed/9074847
- Do, T. et al. Computer-assisted alignment and tracking of acne lesions indicate that most inflammatory lesions. arise from comedones and de novo. J. Am. Acad. Dermatol. 58, 603 – 608 (2008). https://www.ncbi.nlm.nih.gov/pubmed/18249468
- Degitz, K., Placzek, M., Borelli, C. & Plewig, G. Pathophysiology of acne. JDDG 5, 316 – 323 (2007). https://www.ncbi.nlm.nih.gov/pubmed/17376098
- Toyoda, M. & Morohashi, M. Pathogenesis of acne. Med. Electron. Microsc. 34, 29 – 40 (2001). https://www.ncbi.nlm.nih.gov/pubmed/11479771
- Marks, R. Facial skin disorders (Informa Healthcare, 2007).
- Plewig, G. & Kligman, A. Acne and Rosacea (Springer International PU, 2000). https://www.springer.com/gp/book/9783642640964
- Buxton, P. ABC of Dermatology (4th ed). 49 (Blackwell Publishing, 2003). http://famona.sezampro.rs/medifiles/abc/abc of dermatology.pdf
- Orentreich, N. & Durr, N. The natural evolution of comedones into inflammatory papules and pustules. J. Investig. Dermatol. 62, 316 – 320 (1974). https://core.ac.uk/download/pdf/82174419.pdf
- Fox, L., Csongradi, C., Aucamp, M., du Plessis, J. & Gerber, M. Treatment modalities for acne. Molecules 21, 1063 (2016). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6273829/
- Oon, H. H., Wong, S. N., Aw, D. C. W., Cheong, W. K., Goh, C. L. & Tan, H. H. Acne management guidelines by the Dermatological Society of Singapore. J. Clin. Aesthet. Dermatol. 12, 34‐50 (2019). https://www.ncbi.nlm.nih.gov/pubmed/31531161
 Acne.org Products
Acne.org Products