Higher Levels of Male Hormones and Growth Hormone Are Mostly to Blame

The Essential Info
Two main hormonal factors are likely most at fault when it comes to why some people have oilier skin than others:
- Androgens (male hormones found in both males and females): Higher levels of androgens and/or higher sensitivity to androgens may lead to oilier skin.
- Growth hormone (IGF-1): Higher growth hormone levels may lead to oilier skin.
And one factor may result in less oiliness:
- Estrogens (female hormones found in both males and females): Higher levels may lead to less oily skin.
And there are two wildcards that may either increase or decrease skin oiliness:
- Neuropeptides: Depending on the body’s response to these small but powerful proteins, we can see an increase or decrease in skin oiliness.
- Diet: Diets high in simple carbohydrates like candy, white bread, and soda may lead to increased skin oil.

The Science
- Skip Down to What Can Be Done About It?
- Higher Androgen and Growth Hormone Levels Lead to Oilier Skin
- Higher Estrogen Levels Lead to Less Oily Skin
- Neuropeptides and Diet
- Other Factors That Might Affect Sebum Production
Oily skin, medically called seborrhea, is a condition that results when the skin over-produces skin oil (sebum), leaving the skin looking shiny and feeling greasy.
Expand to see technical definition of oily skin
Normal skin: In technical terms, on average, a 2 cm x 5 cm (less than 1″ x 2″) area of skin produces about 1 mg of skin oil every three hours.
Oily skin: If your skin makes more than 1.5 mg every three hours, then you have oily skin.
Dry skin: If your skin makes less than 0.5 mg every three hours, you have dry skin.1
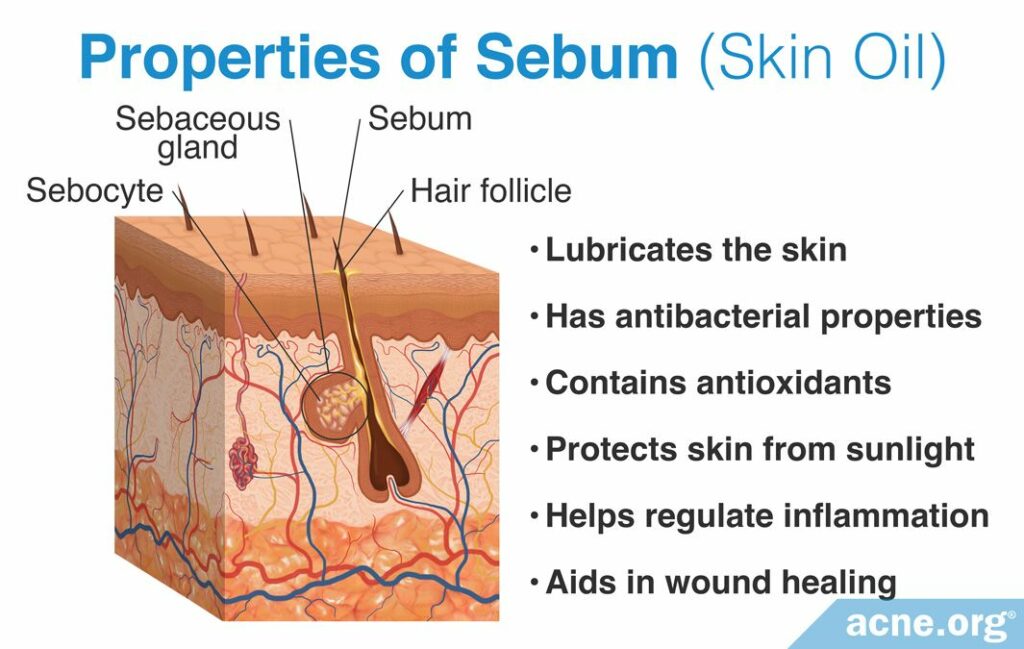
Sebum is produced all over the body in glands called sebaceous glands, that are attached to the sides of skin pores. The face, scalp, and upper torso are most likely to experience excess sebum production.2-4
Even though too much sebum is unwanted, sebum serves several purposes for the skin, as noted in this illustration:
Higher Androgen and Growth Hormone Levels Lead to Oilier Skin
Higher androgen levels: Androgens are male sex hormones that are found in both males and females. Testosterone is the most commonly studied androgen. The majority of testosterone present in the body is produced in the gonads or adrenal glands (found above the kidneys), but it can also be produced in sebaceous glands themselves.

Many studies show us that people with higher levels of androgens tend to have oilier skin. However, higher levels of androgens may not always be required to develop oily skin. Some people may simply be more sensitive to androgens, and this sensitivity may lead to the development oilier skin.3,5
Expand to read details of studies

A 1969 study published in the Journal of Investigative Dermatology studied the effect of testosterone on the sebaceous glands in men. To perform this study, the researchers injected testosterone into 27 adult males on a weekly basis and then measured changes in sebum production and sebaceous gland size over the course of 11 weeks. The researchers found that the testosterone injections increased both the amount of sebum produced and the size of the sebaceous gland, so they concluded that increases in testosterone can increase sebum production and likely also increase oily skin.6

Two 1983 studies published in the New England Journal of Medicine and the Journal of Investigative Dermatology studied the levels of androgens in women with acne. Both studies found that women with acne have higher androgen levels than women without acne. Therefore, the researchers concluded that acne was correlated with an excess of androgens. The researchers involved with this study did not report on whether the elevated androgen levels also caused oily skin. However, as acne is often correlated with oily skin, it is likely that women with acne and excess androgens also had oilier skin.7,8

A 1993 study published in the Journal of Endocrinology and Metabolism studied sebum production in men without androgens in order to determine if androgens likely controlled the production of sebum. The men without androgens in this study were pseudohermaphrodites, who are unable to produce proper sex hormones. The researchers found that the pseudohermaphrodites studied lacked androgens and that because of this, they also did not produce sebum. Therefore, the researchers concluded that there was “absolute androgen control of sebum production.”9

A 1994 study published in the Archives of Dermatology examined the hormones of young girls with acne who had not yet undergone puberty. Prepubescent girls often do not have the same levels of androgens as girls who have gone through puberty, so the point of this study was to understand if the girls’ prepubescent acne was due to abnormal androgen levels. This study examined the hormone levels of 623 acne-prone young girls with an average age of 10 years. They found that one androgen called dehydroepiandrosterone (DHEA) was present at abnormally high levels in the prepubescent girls with acne. DHEA is a hormone that is required for testosterone synthesis. Therefore, the researchers concluded that the prepubescent girls’ acne was likely caused by an elevated level of the androgen DHEA in their blood since androgens, including testosterone, stimulate sebum production. The researchers involved in this study did not report on whether the increase in DHEA also caused oilier skin. However, as acne is often correlated with oily skin, it is likely that the prepubescent girls with acne and elevated DHEA levels also had oilier skin.3,10

A 1983 study published in The Journal of Investigative Dermatology investigated the levels of androgens in adult females with and without acne. The researchers found that 52% of adult acne patients showed “at least one abnormal hormone level” compared to patients without acne. They also found that androgens like testosterone and DHEA were elevated.11 Therefore, it is likely that women with elevated levels of androgens also have oilier skin.

A 1999 study published in the Archives of Dermatology investigated the levels of androgens and IGF-1 in both adult male and female patients with and without acne. The researchers found that androgen levels were increased in both male and female acne patients, while IGF-1 levels were similar in acne and non-acne patients. This study also examined the activities of androgen-producing proteins called 17β-hydroxysteroid dehydrogenase and 5α-reductase. These two proteins are enzymes and metabolize (work to break down) testosterone into DHT, which is a more potent, active form. However, no differences in enzyme activities were found between individuals with and without acne. Therefore, the scientists concluded that the main difference between individuals with and without acne was the levels of androgens, and that acne patients were more likely to have higher levels of androgens. Although oily skin was not a focus of this study, elevated androgen levels will likely also cause increases in sebum production and oilier skin.12,13

A 2014 study published in the Journal of Endocrinology focused on how androgens impact sebum production and secretion in human skin oil glands. The researchers first noticed that skin oil glands contain high levels of proteins that produce androgens and convert them into other forms. These proteins include 5α-reductase, 17β-hydroxysteroid dehydrogenase, 3β-hydroxysteroid dehydrogenase, and steroidogenic acute regulatory protein. They also found that in males, skin oil glands with more 5α-reductase tended to have more androgen receptors as well. As we have seen, 5α-reductase converts testosterone into a more powerful androgen. This means that males with more of this protein in their skin oil glands get a double whammy: their skin oil glands contain a more powerful androgen as well as more androgen receptors, making them more sensitive to androgens. Logically, this likely leads to increased skin oil production. The study concluded that the amount of skin oil is closely tied to how androgens are produced and processed at the level of individual skin oil glands, especially in males.14

A 2014 study published in Experimental Dermatology evaluated the levels of androgen receptors in the T- and U-zones of the face. The T-zone refers to the forehead and nose, while the U-zone includes the cheeks and chin. The authors found that even though these receptors are present in all skin oil glands on the face, the skin oil glands in some areas have more of these receptors and are therefore more sensitive to androgens. For example, skin oil glands in the T-zone have more androgen receptors, which likely explains why people often have more oily skin in this area.5
Higher growth hormone (IGF-1) levels: Growth hormones are hormones secreted by the pituitary gland (found at the base of the skull) that stimulate the body to produce insulin-like growth factor 1 (IGF-1).
Scientists believe that IGF-1 is involved in sebum production and acne development because people show the highest levels of IGF-1 during adolescence, which is also when people are most likely to experience acne.
One study found that acne patients had increased levels of IGF-1 and increased sebum secretion. Another study found that IGF-1 can promote the synthesis of fats in sebaceous glands. These studies, combined with other evidence showing that growth hormone disorders are associated with higher than normal sebum levels and acne, have led researchers to believe that IGF-1 levels are directly correlated with sebum production.2,14
Expand to read details of studies

A 2008 study published in the British Journal of Dermatology investigated the amount of sebum and IGF-1 levels in 11 male and 5 female acne patients. The researchers found that higher sebum levels were correlated with increased IGF-1 levels in men and women. However, an increase in IGF-1 levels was associated with higher acne lesion counts in women, but not men.15 Therefore, the researchers concluded that IGF-1 played an important role in sebum production, but not necessarily acne, in both men and women.
A 2006 study published in the Journal of Investigative Dermatology found that IGF-1 promotes the synthesis of fats (lipids) in sebaceous glands. In this research, scientists stimulated oil-producing glands with IGF-1 and measured the total production of lipids. They found that IGF-1 activates two different molecular pathways, resulting in increased lipid synthesis.16
Higher Estrogen Levels Lead to Less Oily Skin
Higher estrogen levels: Estrogens are female sex hormones that are found in both males and females. Estrogen works to suppress sebum production, leading to less oily skin. However, only females can be treated with estrogen.
Researchers have proposed four hypotheses to explain how estrogens might reduce sebum production:
- Directly counteracting the effects of androgens already in the body.
- Inhibiting the production of testosterone so less testosterone is produced to begin with.
- Decreasing the level of free testosterone in the blood.
- Controlling the activation of genes responsible for synthesizing fats. Since sebum is made of fats, this can decrease sebum production.
Regardless, estrogens work to reduce sebum production, and therefore different levels of estrogen may partly explain why some people’s skin is oilier than others’.10,17
Two Wildcards: Neuropeptides and Diet
Neuropeptides: Neuropeptides are small proteins found within nerve cells that help to regulate a variety of bodily functions, including sebum production.
Researchers have found that sebaceous gland cells can respond to different neuropeptides. Depending on the neuropeptide the sebaceous gland cell encounters, it may activate or suppress sebum production.4 Therefore, differences in how someone’s body responds to neuropeptides may also partly explain why some people have oilier skin than others.
Diet: Studies have found that three specific diets may decrease sebum production in the skin, but it’s important to keep in mind that the science that looks at diet and sebum production is still coming in.
The first diet is a low glycemic load diet, which is a diet that restricts the consumption of simple carbohydrates found in foods like candy, white bread, and soda. Research has found that a low-glycemic diet may cause a reduction in the amount of sebum produced. A typical Western diet contains many foods high in simple carbohydrates, which may cause increases in IGF-1 levels.4
The second diet is an extreme caloric restriction diet, also known as fasting. Two studies have found that fasting can reduce sebum production by up to 20% in the short term. The decrease in sebum production caused by fasting is reversed when the individual returns to a normal diet.4
The third diet is the Mediterranean diet. The Mediterranean diet is a healthy diet rich in omega-3 fatty acids (from fish), as well as being high in vegetables, fruits, and nuts. This type of diet may lower the blood levels of IGF-1 and in turn make our skin less oily.18
And what about dairy? While it remains a subject of debate, reducing the amount of milk and dairy we eat might reduce the amount of sebum we produce. Researchers hypothesize that milk and dairy products may increase IGF-1 levels18 and thus stimulate increased sebum production.
Other Factors That Might Affect Sebum Production
Two other potential factors might influence skin oiliness:
- Ethnicity: Generally, people who have larger skin pores tend to produce more skin oil. Studies have found that the size of skin pores may differ across ethnicities. For example, women of Chinese background may have smaller pores while people of African background may have larger pores.
- Humidity: Humid climates might lead to oilier skin. Similarly, people’s skin might produce more skin oil at humid times of year, although not all studies agree on whether this occurs.1
So What Can Be Done About It?
Males & females: There are several treatments that can help, including non-prescription treatments (e.g. topical green tea) as well as prescription treatments (e.g. Botox®).
Females only: Hormonal treatments (e.g. oral contraceptives and/or anti-androgen medications like spironolactone) are an option, but are usually not recommended to simply correct oily skin.
References
- Endly, D. C. & Miller, R. A. Oily skin: A review of treatment options. J Clin Aesthet Dermatol 10, 49‐55 (2017). https://pubmed.ncbi.nlm.nih.gov/28979664/
- Smith, K. R. & Thiboutot, D. M. Sebaceous gland lipids: friend or foe? J Lipid Res 49, 271 – 281 (2008). https://www.ncbi.nlm.nih.gov/pubmed/17975220
- Thibutout, D. Regulation of human sebaceous glands. J Invest Dermatol 123, 1 – 12 (2004). https://www.ncbi.nlm.nih.gov/pubmed/15191536
- Makrantonaki, E., Ganceviciene, R. & Zouboulis, C. C. An update on the role of the sebaceous gland in the pathogenesis of acne. Dermatoendocrinol 3, 41 – 49 (2011). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3051853/
- Seo, Y. J. et al. Regional difference in sebum production by androgen susceptibility in human facial skin. Experimental Dermatology 23, 70-72 (2014). https://pubmed.ncbi.nlm.nih.gov/24289322/
- Pochi, P. E. & Stauss, J. S. Sebaceous gland response in man to the administration of testosterone, ∆4-androstenedione, and dehydroisoandrosterone. J Investig Dermatol 52, 32 – 36 (1969). https://www.ncbi.nlm.nih.gov/pubmed/4236132
- Marynick, S. P., Chakmakjian, Z. H., McCaffree, D. L. & Herndon, J. H. Androgen excess in cystic acne. New Engl J Med 308, 981 – 986 (1983). https://www.ncbi.nlm.nih.gov/pubmed/6220224
- Lucky, A. W., McGuire, J., Rosenfield, R. L., Lucky, P. A. & Rich, B. H. Plasma androgens in women with acne vulgaris. 81, 70 – 74 (1983). https://www.ncbi.nlm.nih.gov/pubmed/6223099
- Imperato-McGinley, J. et al. The androgen control of sebum production. Studies of subjects with dihydrotestosterone deficiency and complete androgen insensitivity. J Clin Endocrinol Metab 76, 524 – 528 (1993). https://www.ncbi.nlm.nih.gov/pubmed/8381804
- Lucky, A. W. et al. Acne vulgaris in premenarchal girls. An early sign of puberty associated with rising levels of dehydroepiandrosterone. Arch Dermatol 130, 308 – 314 (1994). https://www.ncbi.nlm.nih.gov/pubmed/8129408
- Lucky, A. W., McGuire, J., Rosenfield, R. L., Lucky, P. A. & Rich, B. H. Plasma androgens in women with acne vulgaris. J Investig Dermatol 81, 70 – 74 (1983). https://www.ncbi.nlm.nih.gov/pubmed/6223099
- Thiboutot, D., Gilliland, K. & Lookingbill, D. Androgen metabolism in sebaceous glands from subjects with and without acne. Arch Dermatol 135, 1041 – 1045 (1999). https://www.ncbi.nlm.nih.gov/pubmed/10490108
- Cappel, M., Mauger, D. & Thiboutot, D. Correlation between serum levels of insulin-like growth factor 1, dehydroepiandrosterone sulfate, and dihydrotestosterone and acne lesion counts in adult women. Arch Dermatol 141, 333 – 338 (2005). https://www.ncbi.nlm.nih.gov/pubmed/15781674
- Inoue, T. et al. Expression of steroidogenic enzymes in human sebaceous glands. The Journal of Endocrinology 222, 301-12 (2014). https://pubmed.ncbi.nlm.nih.gov/24938708/
- Vora, S., Ovhal, A., Jerajani, H., Nair, N., and Chakrabortty, A. Correlation of facial sebum to serum insulin‐like growth factor‐1 in patients with acne. British Journal of Dermatology 159, 990–991 (2008) https://pubmed.ncbi.nlm.nih.gov/18652583/
- Smith, T. M. et al. Insulin-like growth factor-1 induces lipid production in human SEB-1 sebocytes via sterol response element-binding protein-1. The Journal of Investigative Dermatology 126, 1226-1232 (2006). https://pubmed.ncbi.nlm.nih.gov/16575389/
- Elsaie, M. L. Hormonal treatment of acne vulgaris: an update. Clinical, Cosmetic and Investigational Dermatology 9, 241-248 (2016). https://pubmed.ncbi.nlm.nih.gov/27621661/
- Baldwin, H. & Tan, J. Effects of diet on acne and its response to treatment. American Journal of Clinical Dermatology 22,55-65 (2021). https://pubmed.ncbi.nlm.nih.gov/32748305/
 Acne.org Products
Acne.org Products