Papules Are Red, Slightly Elevated Acne Lesions Less than 5mm in Size and Do Not Contain Pus

The Essential Info
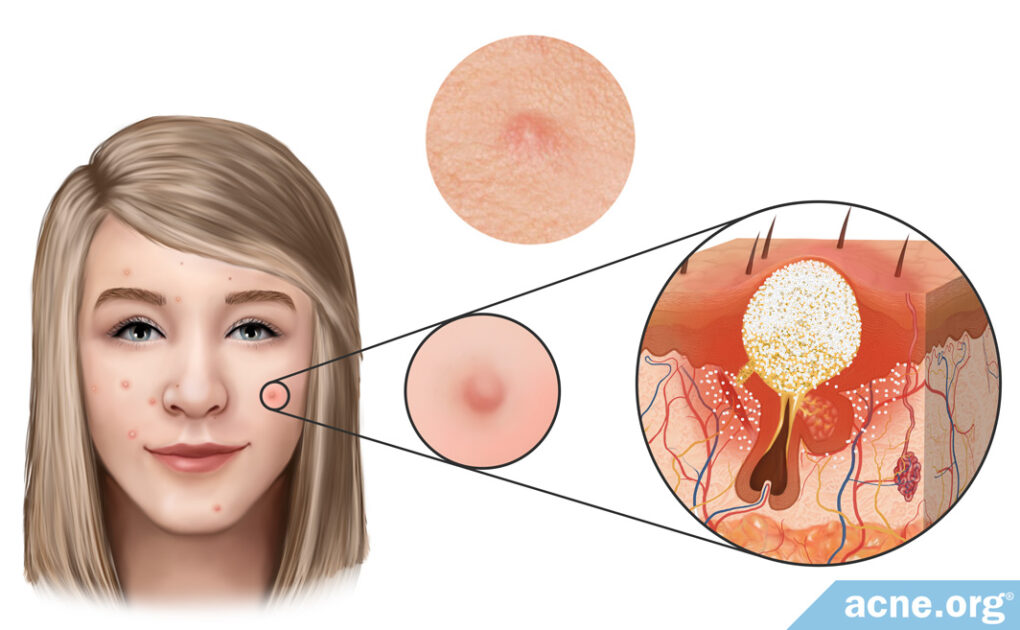
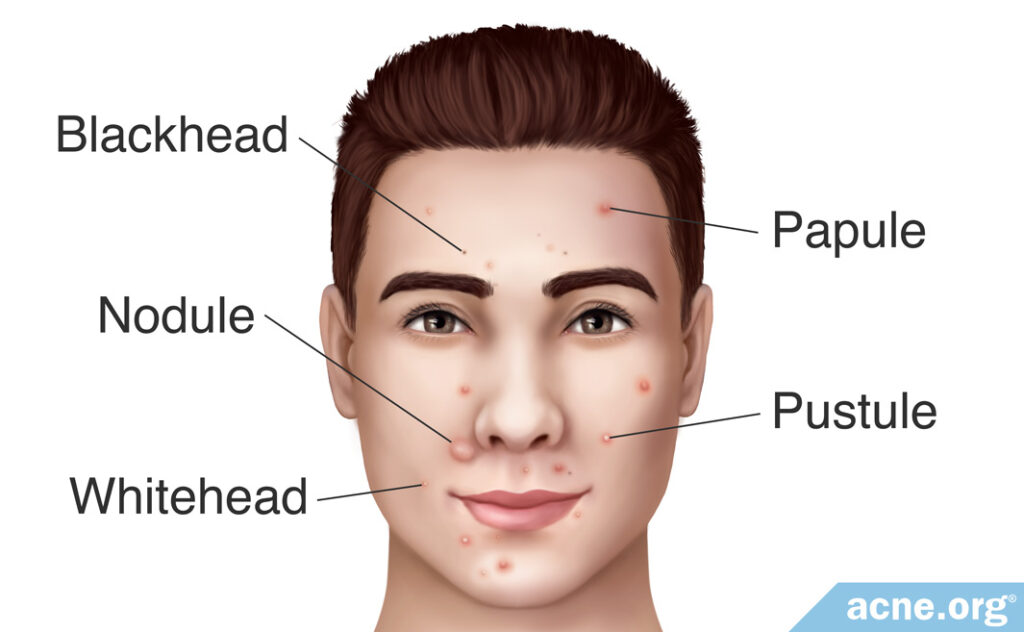
Papules are relatively small (less than 5 mm across), red, slightly elevated acne lesions that normally develop on the face, neck, chest, back, shoulders, and upper arms. After a few days, papules normally fill with pus and develop a white or yellow center, at which point they are then called pustules, which can be popped.
Papules occur when a pore becomes clogged, and skin oil that normally drains to the surface gets trapped inside. Acne bacteria then grows inside the trapped skin oil, and the lesion becomes a red, sore, raised lesion called a papule.
Never Attempt to Pop a Papule: Wait until it has filled with pus and has an obvious white or yellow center before attempting to pop it.

The Science
Almost everyone has had a papule. Papules are relatively small, slightly elevated, red, sore bumps less than 5mm in diameter that are commonly found on the face, neck, back, chest, shoulders, and upper arms. They are the red bumps you see on your skin before they fill with pus and turn into “zits” that have a white or yellow center.
Like other acne lesions, papules are more common among teenagers and young adults as their bodies undergo hormonal changes, but papules can also occur later in life.1
Sometimes papules develop as a side effect of cosmetics. A recent study conducted in China found that drugstore cosmetics induced papules in about a third of women.2
How Papules Develop
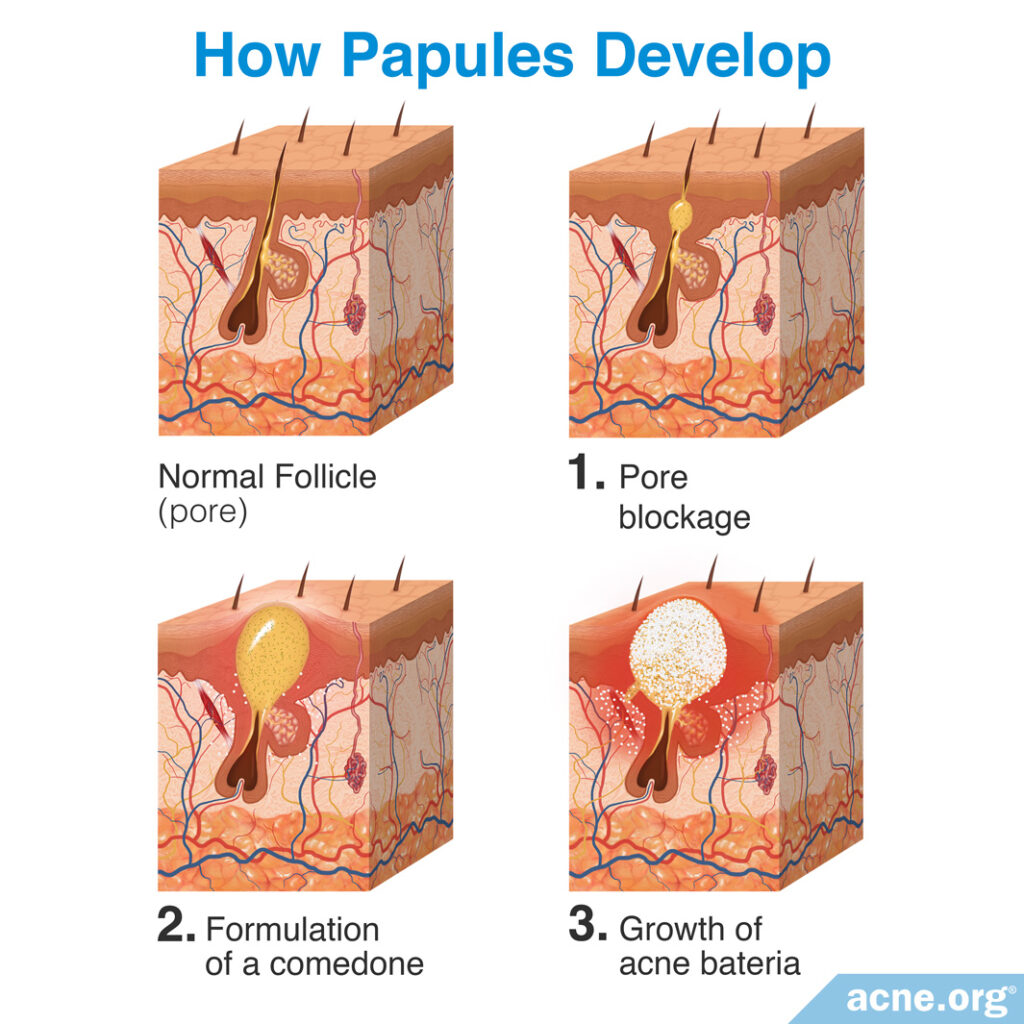
Most papules are formed in three steps:
Step 1 – Pore blockage: Acne development begins with microscopic hair follicles (pores) in the skin. Attached to these pores are glands called sebaceous glands, which produce skin oil, called sebum. Normally, the sebum freely flows out of the pore and onto the surface of the skin. Acne develops when a pore becomes blocked and sebum accumulates inside the pore.
Step 2 – Formation of a comedone: Once the pore is blocked and sebum begins accumulating inside the pore, it enlarges and becomes visible. This visible acne lesion is called a comedone, which is more commonly known as a whitehead or blackhead.
Step 3 – Growth of acne bacteria: Inside of a comedone is a large accumulation of sebum. This is a suitable environment for acne bacteria (C. acnes). Inside the comedone, C. acnes feeds on the sebum and begins to reproduce rapidly. As the amount of C. acnes present inside the pore increases, the body sees it as an infection and responds by sending in inflammatory cells called neutrophils. Neutrophils release enzymes to attack the C. acnes in order to kill it. However, this weakens the wall of the pore, and can cause the pore to rupture. This rupture ends up releasing the contents of the pore (sebum, C. acnes, neutrophils, and dead skin cells) into the surrounding skin. The body views these contents as “invaders” and responds with an inflammatory response, resulting in an inflamed, red, firm, slightly raised and sore acne lesion called a papule.3-6 Even though papules begin to appear red at this stage, scientists now believe that inflammation may actually start brewing inside these lesions from the earliest stages of their formation.7
Another way papules develop: A 2008 study published in the Journal of the American Academy of Dermatology found that step two of papule development was skipped in 28% of acne patients. That is to say, they had papules that did not develop from a comedone (whitehead or blackhead). Instead, the papules developed directly from an initial clogged pore.8 Researchers do not yet fully understand how this happens.
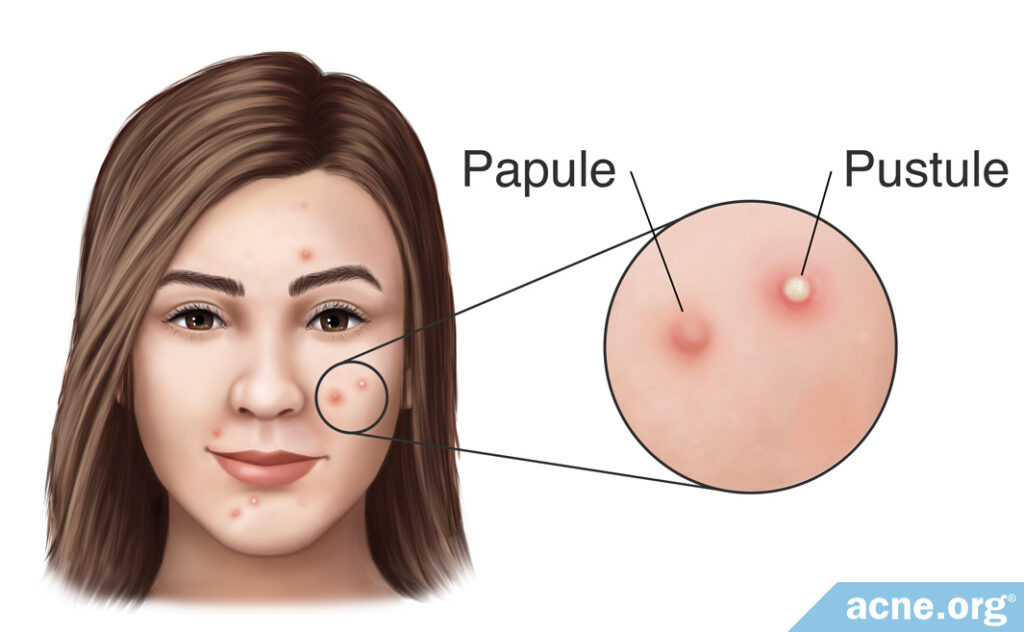
Within a few days most papules fill with pus and become pustules, which are the acne lesions that people normally refer to as “zits” that have a white/yellow center and can be popped. Occasionally, papules sometimes stay on the skin for multiple days or even weeks without developing into pustules, but this is rare.8
Depending on a person’s genetic propensity to scar, papules and pustules may clear without leaving a scar or can leave scarring behind.9,10
Never Pop a Papule!
Because papules are not filled with pus, they cannot be popped. If you attempt to pop a papule, it will likely make the lesion worse, cause it to stay around for a longer time, and increase the chance of scarring. Always wait until a papule has filled with pus and has an obvious white or yellow center before attempting to pop it.
Treating Papules
Since you can’t pop papules, attack them with proven anti-acne treatments, which include both over-the-counter and prescription options.11,12 A stand-out over-the-counter treatment is benzoyl peroxide. You can find a full list of acne treatments and their ratings here.
References
- Cleveland Clinic: Acne Papules; https://my.clevelandclinic.org/health/diseases/22905-acne-papules
- Wang, S., Jiang, Y., Lyu, J., Li, J. &, Diao, Q. Adverse reactions to cosmetics reported to the Chongqing adverse drug reaction monitoring centre system in China. Contact Dermatitis 88, 201-205 (2023). https://pubmed.ncbi.nlm.nih.gov/36385252/
- Bhate, K. & Williams, C. Epidemiology of acne vulgaris. Br. J. Dermatol. 168, 474 – 485 (2013). https://pubmed.ncbi.nlm.nih.gov/23210645/
- Degitz, K., Placzek, M., Borelli, C. & Plewig, G. Pathophysiology of acne. JDDG 5, 316 – 323 (2007). https://pubmed.ncbi.nlm.nih.gov/17376098/
- Toyoda, M. & Morohashi, M. Pathogenesis of acne. Med. Electron. Microsc. 34, 29 – 40 (2001). https://pubmed.ncbi.nlm.nih.gov/11479771/
- Brogden, R. & Goa, K. Adapalene. Drugs 53, 511 – 519 (1997). https://pubmed.ncbi.nlm.nih.gov/9074847/
- Tanghetti, E. A. The role of inflammation in the pathology of acne. J. Clin. Aesthet. Dermatol. 6, 27‐35 (2013). https://pubmed.ncbi.nlm.nih.gov/24062871/
- Do, T. et al. Computer-assisted alignment and tracking of acne lesions indicate that most inflammatory lesions. arise from comedones and de novo. J. Am. Acad. Dermatol. 58, 603 – 608 (2008). https://pubmed.ncbi.nlm.nih.gov/18249468/
- Orentreich, N. & Durr, N. The natural evolution of comedones into inflammatory papules and pustules. J. Investig. Dermatol. 62, 316 – 320 (1974). https://core.ac.uk/download/pdf/82174419.pdf
- Buxton, P. ABC of Dermatology (4th ed). 49 (Blackwell Publishing, 2003). http://famona.sezampro.rs/medifiles/abc/abc%20of%20dermatology.pdf
- Oon, H. H., Wong, S. N., Aw, D. C. W., Cheong, W. K., Goh, C. L. & Tan, H. H. Acne management guidelines by the Dermatological Society of Singapore. J. Clin. Aesthet. Dermatol. 12, 34‐50 (2019). https://pubmed.ncbi.nlm.nih.gov/31531161/
- Seok, J., Kim, J. H., Kim, J. M. et al. Effects of intradermal radiofrequency treatment and intense pulsed light therapy in an acne-induced rabbit ear model. Sci. Rep. 9, 5056 (2019). https://www.nature.com/articles/s41598-019-41322-x
 Acne.org Products
Acne.org Products