Milia Are Harmless Skin Bumps Unrelated to Acne

The Essential Info
Milia are tiny, harmless bumps that develop on the skin of both adults and children. Normally, they go away on their own without treatment within a few weeks, or at most a few months. However, if milia is recurring or persistent, dermatologists can effectively treat milia with surgical procedures or topical prescriptions.
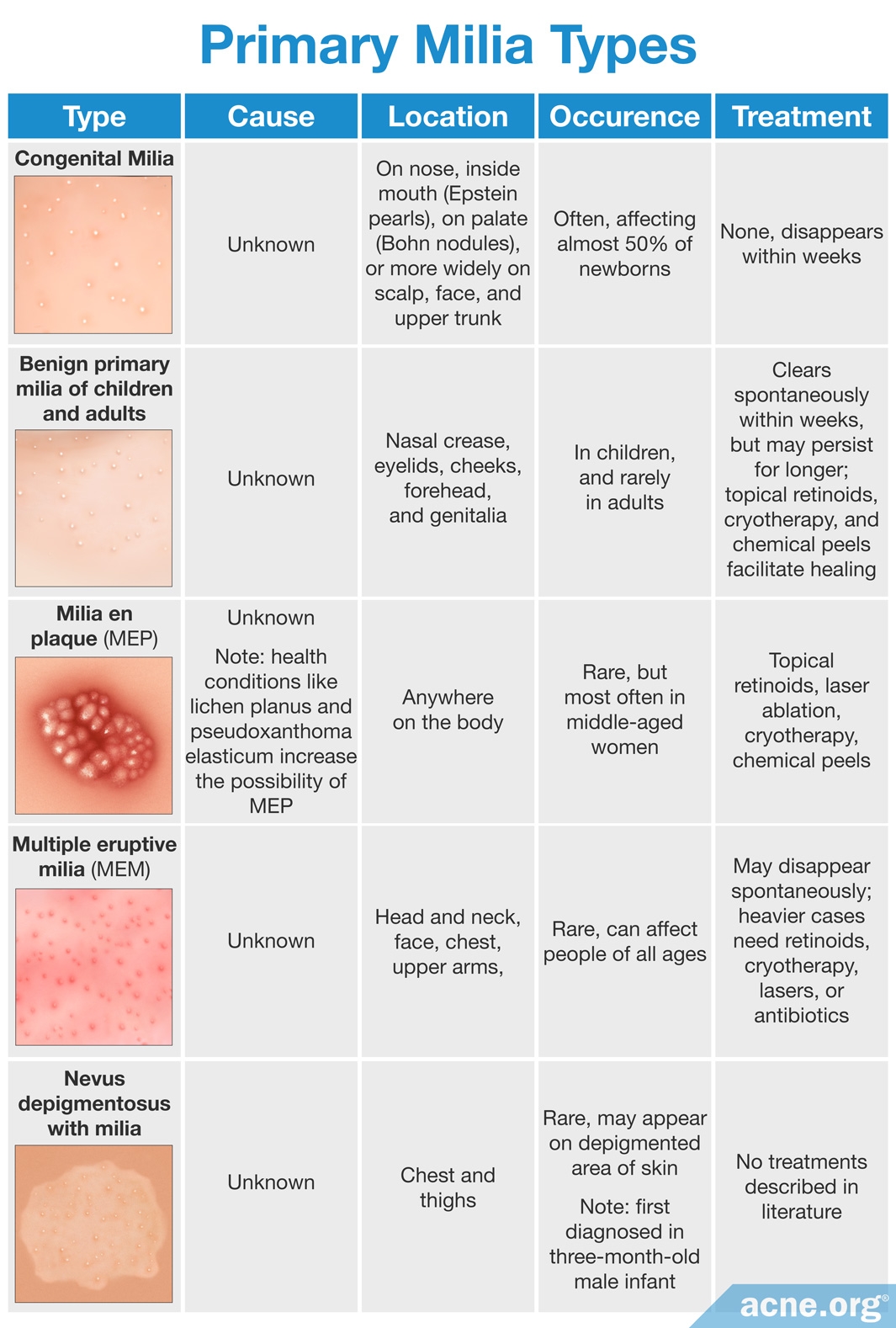
Primary milia is what most people think of when they think of milia–small white-ish bumps on the skin. They are common and develop in skin pores in people of all ages. They appear and disappear for unknown reasons, and research has not discovered the true cause(s) of primary milia.
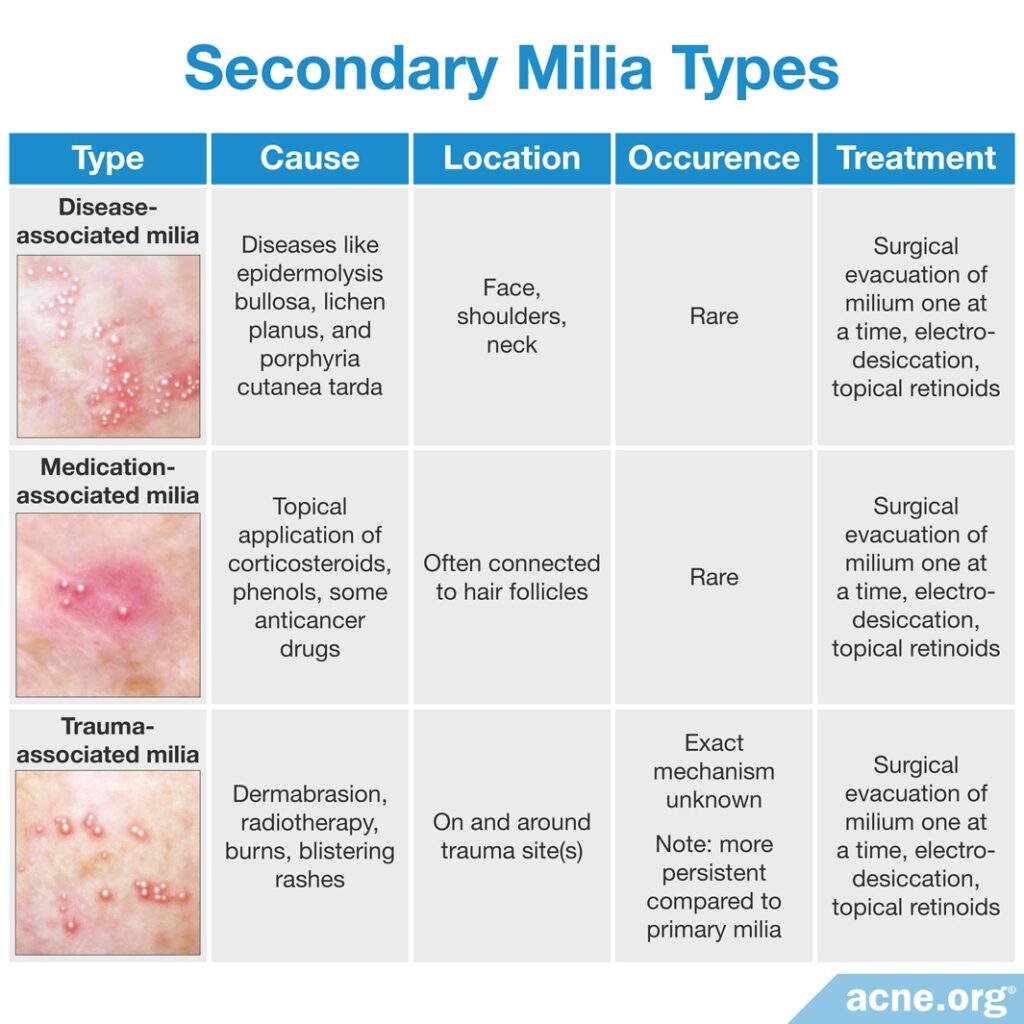
Secondary milia are rare and almost always develop in sweat ducts as a side effect of particular skin diseases, medications, or traumas.
While milia and acne can look similar, they are not the same and do not respond to the same treatment.

The Science
- Definition of Milia
- Types of Milia
- At What Age Do People Experience Milia?
- What Are the Most Common Forms?
- Development of Milia
- Causes of Milia
- Milia and Acne
- Treatments for Milia
Milia are tiny, harmless bumps that can affect adults and children and resemble acne but have little connection to acne. The condition responds to certain treatments, but normally goes away without treatment.
Definition of Milia
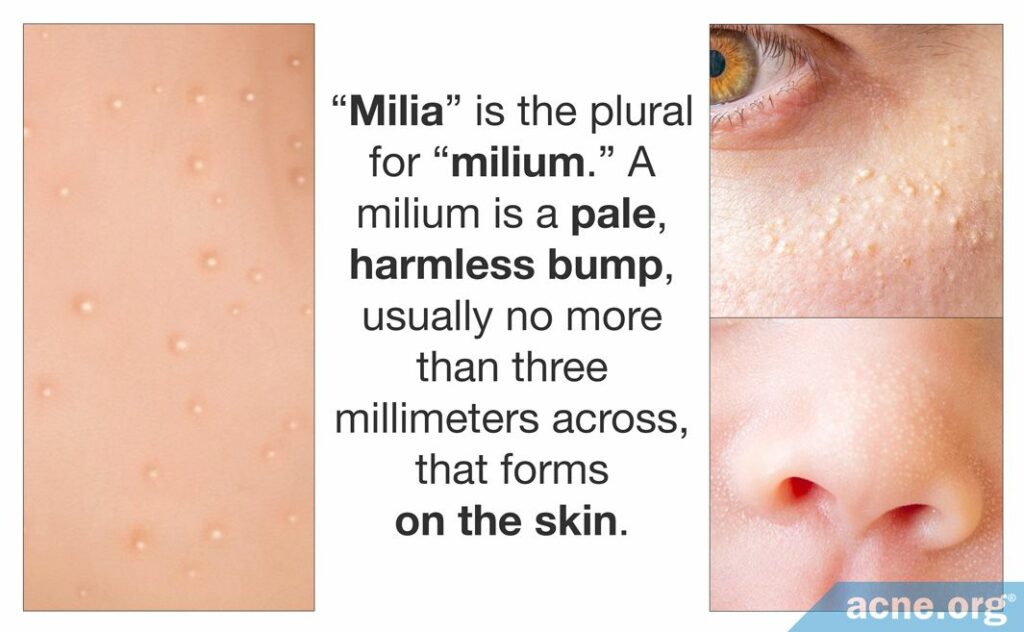
“Milia” is the plural for “milium.” A milium is a pale, harmless bump, usually no more than three millimeters across, that forms on the skin. In the Journal of Investigative Dermatology in 1956, Epstein and Kligman described milia as the most common type of benign skin tumors.1,2
Medical experts call these bumps “cysts,” and these tiny cysts contain keratin (a skin protein).
Types of Milia
Many types of milia exist, but they usually fall into two categories.
- [Common] Primary milia, which occur without any obvious cause and are located inside pores.
- [Uncommon] Secondary milia, which develop as a side effect of certain diseases, such as herpes zoster, contact dermatitis, and leishmaniasis, and traumas, including blistering, sun damage, dermabrasion, or medications like corticosteroids, and are located next to sweat ducts.
At What Age Do People Experience Milia?
Milia can affect people at any age, although it affects babies most often.
According to a 2008 article in American Family Physician, “They occur in up to 50 percent of newborns.”3 This condition, called congenital milia, usually resolves itself within a few months.
What Are the Most Common Forms?
Congenital milia and a form of milia that affects older children and adults for no apparent reason, called benign (harmless) primary milia, are the two most common forms.
Rarer and more severe forms include multiple eruptive milia (MEM), in which so many milia form that doctors can no longer call it benign,4,5 and milia en plaque (MEP), in which the bumps form lesions (breaks in the skin) and plaques (raised patches of skin).6
Development of Milia
Limited information exists on exactly how milia develop, and whether the cells inside milia divide like normal skin cells or like abnormal cells.7 However, scientists have learned more about where in the skin they develop.
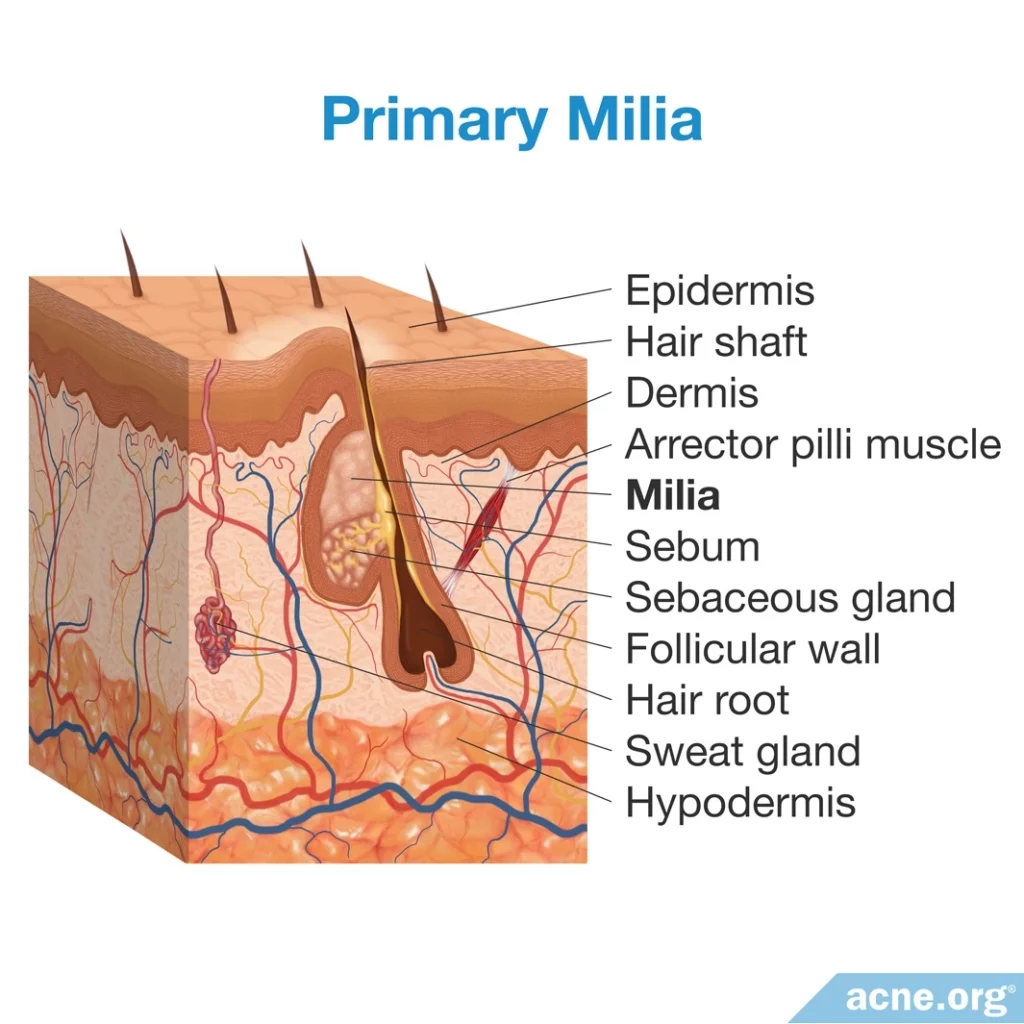
Where Do Primary Milia Develop?
Primary milia often occur in the sebaceous glands (oil glands) inside hair follicles (skin pores).
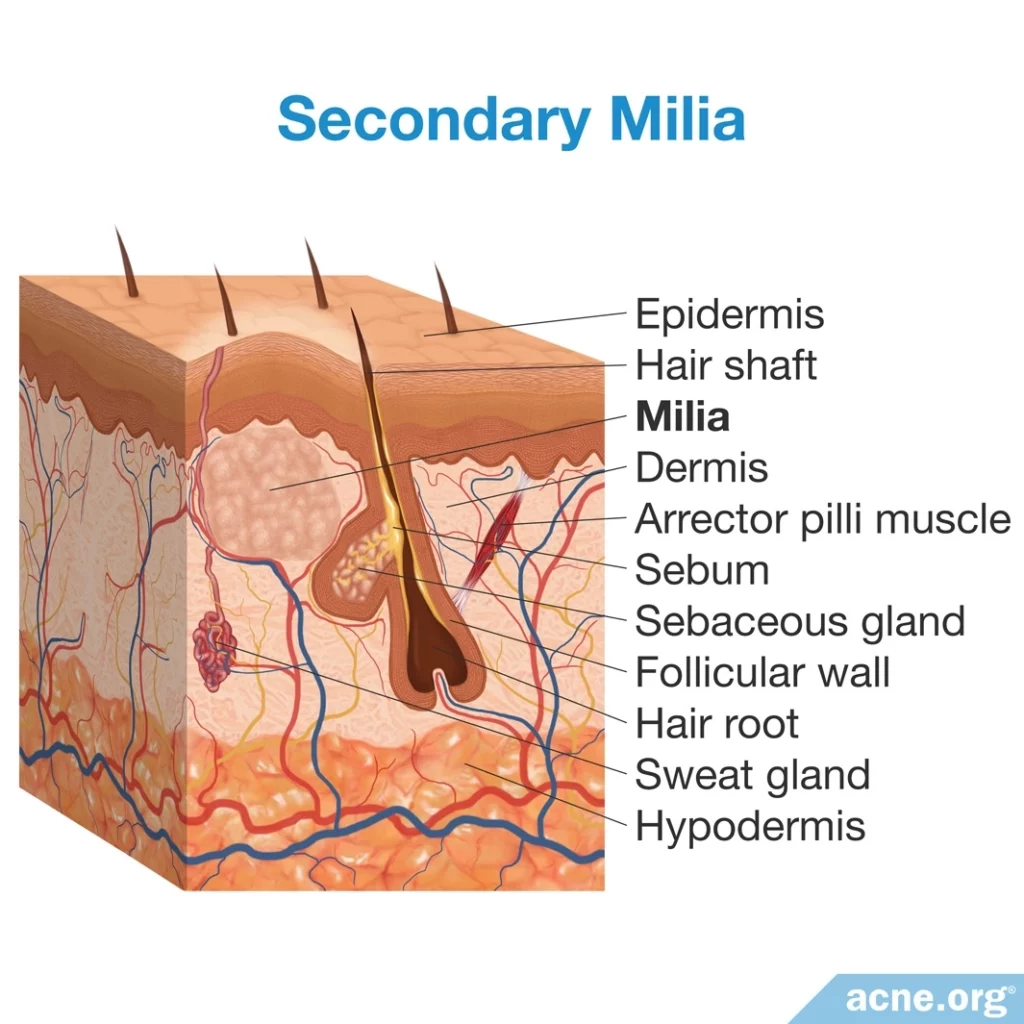
Where Do Secondary Milia Develop?
Secondary milia normally occur next to eccrine ducts (sweat ducts).
A study published in the Journal of Investigative Dermatology in 1975 reports that of the 73 biopsy specimens taken from 10 patients with secondary milia, 54 of them had milia connected to eccrine ducts; 2 had milia in skin pores; and the remaining 17 specimens had milia with no connections to skin pores or to eccrine ducts.8
Causes of Milia
What Causes Primary Milia?
Scientists have yet to discover what causes primary milia. Some members of the public speculate that when primary milia occurs in adults, cosmetics may play a role, claiming that ingredients in cosmetics that cause or aggravate acne may also cause or aggravate milia. However, no research studies exist to support this claim.
What Causes Secondary Milia?
Secondary milia are rare and occur as a side effect of certain skin diseases, topical medications, or skin trauma.
Expand to read details of a study on corticosteroid medication and milia
A study on medication-induced milia in a 1986 issue of the journal Archives of Dermatology examined six men and three women treated with topical corticosteroids (drugs used to treat inflammation). The corticosteroids caused these patients to experience milia followed by skin deterioration and dilated blood vessels in the skin. The examiners stated, “Fifteen (88%) of 17 milia removed were connected with hair follicles; the origin of the others was not clear.” The authors of the study believed that the weakening of collagen (skin protein) around the follicles may have led to the milia.9
Milia may also occur after skin treatments.
Expand to read details of studies on skin treatments and milia

The Journal of the American Academy of Dermatology reported in 2008 that hyaluronic acid, a popular filler for acne scars, causes side effects that include “erythema, edema, bruising, inflammation, delayed reactions, infection, pain, milia or acne, and rare reports of necrosis.” It also stated that possible side effects from laser therapy “may include delayed healing, erythema, milia, acne, edema, hyperpigmentation or hypopigmentation, infection, or scarring.”10

A 2001 article in the journal Dermatologic Clinics notes that milia “appear as part of the healing process…after dermabrasion,” although it also found that “saline scrubs immediately post-surgery may minimize [the development of] milia.“11
Milia and Acne
Although milia and acne develop in the skin, they have little to do with each other, mostly because milia has no connection with inflammation or bacteria as acne does.12 However, excessive picking or rubbing of milia can cause inflammation and make milia look like red, inflamed acne. Dermatologists call this red, inflamed milia pseudoacne. Because it is not acne, common acne treatments will not effectively treat it.13
Treatments for Milia
Primary milia usually go away on their own within a few weeks or at most a few months. However, some patients with persistent or recurring cases may want to see a dermatologist to help to make them heal faster. Fortunately, both primary and secondary milia respond to a number of medical treatments, including:
Common Treatments
- Medical staff can treat them surgically, with tools such as scalpels or needles.14
- A six-week course of a topical retinoid drug called tretinoin can eliminate milia.1 Other retinoid drugs, such as tazarotene and adapalene, work similarly to tretinoin. If tretinoin works, then these may work as well.

A CO2 laser treatment successfully treated four milia patients in a 2010 study reported in the Journal of Cosmetic and Laser Therapy.15

One extreme case in the Journal of Cutaneous Medicine and Surgery in 2006 demonstrated more than 80 percent clearing of the patient’s condition in 3 months with a special device used to remove skin cells by drying them out (electrodesiccation).16
References
- Connelly, T. Eruptive milia and rapid response to topical tretinoin. Arch. Dermatol. 144, 816 – 817 (2008). https://www.ncbi.nlm.nih.gov/pubmed/18559787
- Epstein, W. & Kligman, A. M. The Pathogenesis of Milia and Benign Tumors of the Skin. J. Investig. Dermatol. 26, 1 – 11 (1956). https://www.ncbi.nlm.nih.gov/pubmed/13295633
- Connor, N. R., McLaughlin, M. R. & Ham, P. Newborn skin: Part I. Common rashes. Am. Fam. Physician 77, 47 – 52 (2008). https://www.ncbi.nlm.nih.gov/pubmed/18236822
- Cairns, M. L. & Knable, A. L. Multiple Eruptive Milia in a 15-year-old Boy. Pediatr. Dermatol. 16, 108 – 110 (1999). https://pdfs.semanticscholar.org/e1fe/9d87147a58f54401c364ede2e11d38b5a69c.pdf
- Diba, V. C., Handfield-Jones, S., Rytina, E., Hall, P. & Burrows, N. Multiple eruptive milia in a 9-year-old boy. Pediatr. Dermatol. 25, 474 – 476 (2008). https://onlinelibrary.wiley.com/doi/abs/10.1111/jdv.13476
- Hubler, W. R. Jr., Rudolph, A. H. & Kelleher, R. M. Milia en plaque. Cutis 22, 67 – 70 (1978). https://www.ncbi.nlm.nih.gov/pubmed/668413
- Berk, D. R. & Bayliss, S. J. Milia: A review and classification. J. Am. Acad. Dermatol. 59, 1050 – 1063 (2008). https://www.ncbi.nlm.nih.gov/pubmed/18819726
- Tsuji, T., Sugai, T. & Suzuki, S. The mode of growth of eccrine duct milia. J. Investig. Dermatol. 65, 388 – 393 (1975). https://www.ncbi.nlm.nih.gov/pubmed/1176789
- Tsuji, T., Kadoya, A., Tanaka, R., Kono, T. & Hamada, T. Milia induced by corticosteroids. Arch. Dermatol. 122, 139 – 140 (1986). https://jamanetwork.com/journals/jamadermatology/article-abstract/546864
- Rivera, A. E. Acne scarring: A review and current treatment modalities. J. Am. Acad. Dermatol. 59, 659 – 676 (2008). https://www.ncbi.nlm.nih.gov/pubmed/18662839
- Brody, H. J. Complications of chemical resurfacing. Dermatol. Clin. 19, 427 – 438 (2001). https://www.ncbi.nlm.nih.gov/pubmed/11599399
- Vlassova, N., Han, A., Zenilman, J. M., James, G. & Lazarus, G. S. New horizons for cutaneous microbiology: The role of biofilms in dermatological disease. Br. J. Dermatol. 165, 751 – 759 (2011). https://www.ncbi.nlm.nih.gov/pubmed/21668434
- Admani, S. & Barrio, V. R. Evaluation and treatment of acne from infancy to preadolescence. Dermatol. Ther. 26, 462 – 466 (2013). https://www.ncbi.nlm.nih.gov/pubmed/24552409
- Thami, G. P., Kaur, S. & Kanwar, A. J. Surgical pearl: Enucleation of milia with a disposable hypodermic needle. J. Am. Acad. Dermatol. 47, 602 – 603 (2002). https://www.ncbi.nlm.nih.gov/pubmed/12271307
- Pozo, J. D., Castiñeiras, I. & Fernández-Jorge, B. Variants of milia successfully treated with CO(2) laser vaporization. J. Cosmet. Laser Ther 12, 191 – 194 (2010). https://www.semanticscholar.org/paper/Variants-of-milia-successfully-treated-with-CO(2)-Pozo-Castiñeiras/f76daac45a25512433e0b8fd14efbb51130e4dfe
- Al-Mutairi, N. & Joshi, A. Bilateral Extensive Periorbital Milia en Plaque Treated with Electrodesiccation. J. Cut. Med. Surg. 10, 193 – 196 (2006). https://www.ncbi.nlm.nih.gov/pubmed/17234118
 Acne.org Products
Acne.org Products