Probiotics Can Have a Positive Effect on Gut Bacteria Balance and Might Help

The Essential Info
Gut Bacteria
Gut bacteria play an important role in the human body, and disrupting the normal balance of these bacteria, as occurs when you take oral antibiotics, can cause a variety of negative effects.
How Probiotics Might Help with Acne
Probiotics can have a positive effect on the balance of gut bacteria and might help combat acne by:
- Reducing inflammation
- Decreasing skin oil production
- Helping to balance some of the negative effects of antibiotics
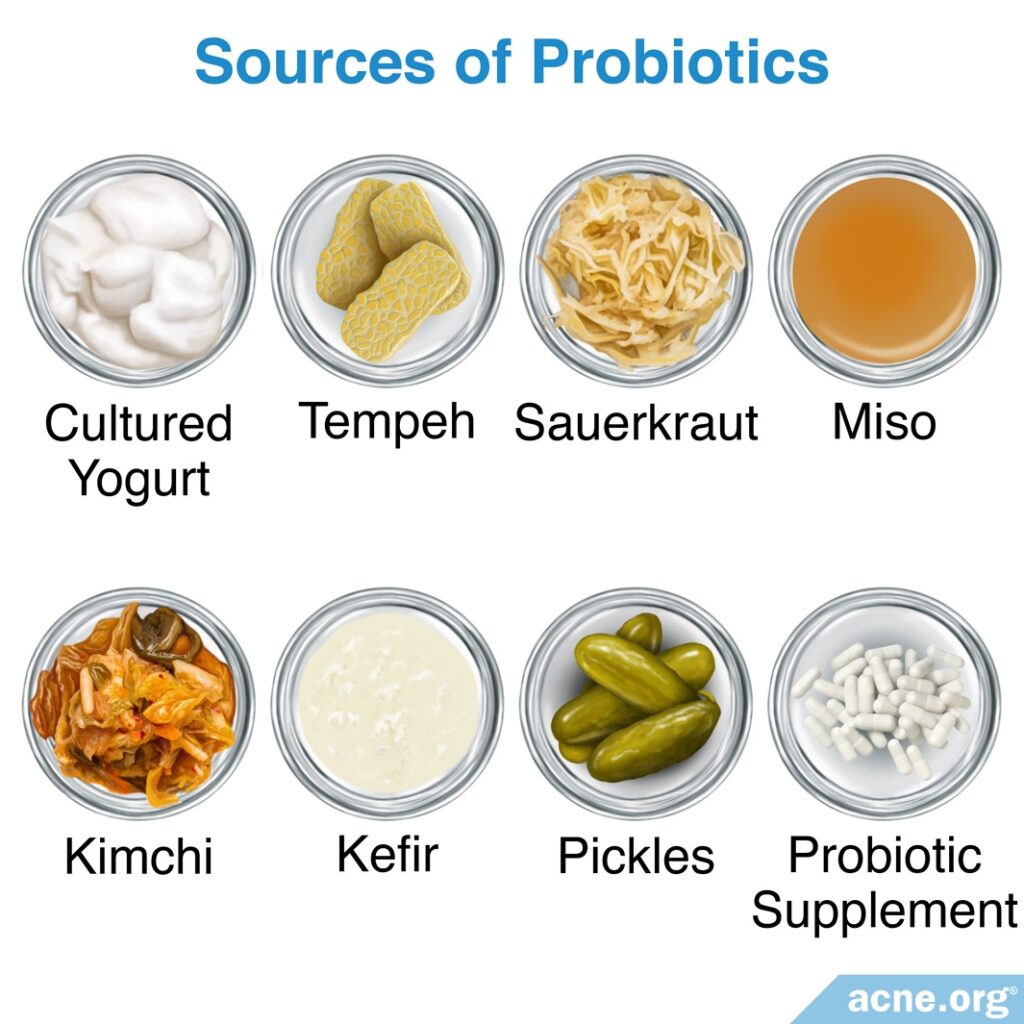
You Can Get Probiotics From:
- Yogurt
- Tempeh
- Sauerkraut
- Miso
- Kimchi
- Kefir
- Pickled foods: Make sure they don’t contain vinegar since this kills bacteria.
- Probiotic supplements: Various probiotic supplements contain different combinations of bacterial strains. There is some evidence that L. acidophilus may be beneficial in treating acne. However, other strains may be helpful as well. Probiotic supplements are not regulated by the U.S. Food and Drug Administration (FDA), and there is controversy over whether they work as well as probiotic-containing food, or even whether they work at all. Buyer beware!
Keep Your Expectations Realistic
While it is a fascinating area of research, taking probiotics is unlikely to completely clear acne. It won’t hurt to regularly eat probiotic-containing foods, but keep your expectations grounded.
My Take on This
My common sense tells me that focusing in too narrowly on probiotics might miss the bigger picture of overall gut health, which requires us to eat a healthy diet that is rich in fiber over a long period of time. Just taking probiotic pills is unlikely to work wonders on its own. Instead, the way I approach gut health is to avoid antibiotics unless they are absolutely necessary. I always push back on any doctor who prescribes them, and will only take them if my doctor really thinks it’s vital. And then, as an overall lifestyle, because I love fermented food like kimchi, I eat them as often as I can, but also try to focus on eating fiber-rich foods every day to feed the “good bugs” down in my intestines.

The Science
- What Is Gut Bacteria
- Relationship Between Gut Bacteria and Acne
- Probiotics Help Balance Gut Bacteria
- Do Probiotics Help Acne?
- What about Topical Probiotics?
- Buying the Right Probiotic
- The Bottom Line
Acne is in part a bacterial disease. Acne bacteria that lives in the skin plays a role in the inflammation that occurs in acne lesions.1,2
However, what about the bacteria in our gut? Can that have an effect on acne? The tentative answer at this point is “perhaps, especially while taking oral antibiotics and after taking them.”
Let’s dive in.
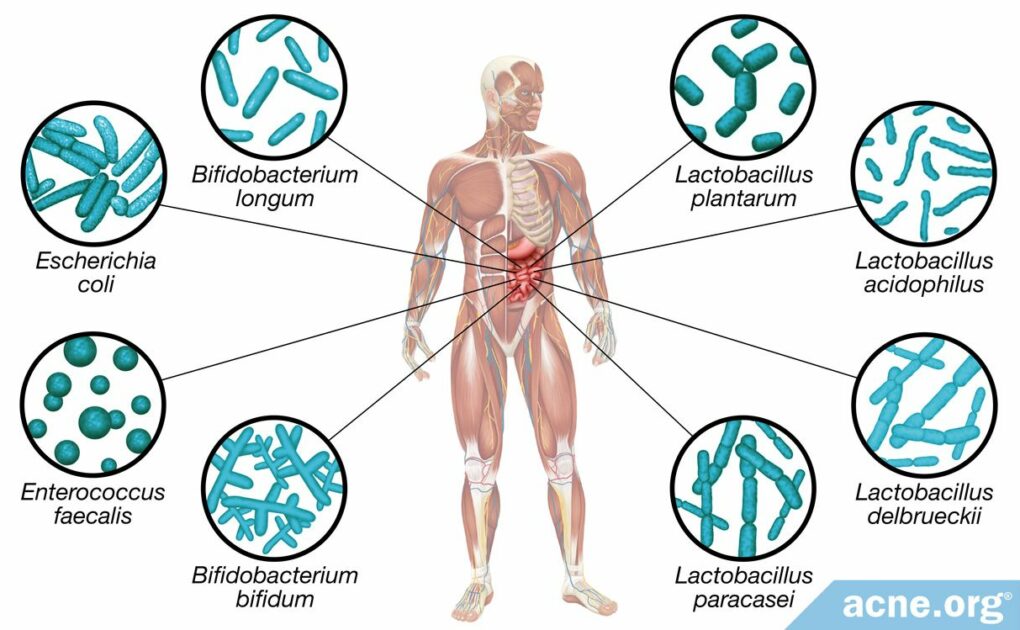
What Is Gut Bacteria?
Gut bacteria, also called the gut microbiota or microbiome, is the bacteria that lives in the gastrointestinal tract (gut). Trillions of bacteria of many different species live in the human gut. According to a 2011 article in the Journal of Clinical Gastroenterology:
“The [microbiome] of the human intestine is diverse and abundant. It is estimated there are as many as 1000 different bacterial species and >7000 different strains living in the tract.”3
Generally speaking, the bacteria that live in the gut are not harmful. In fact, research has shown that disruption of the normal balance of these bacteria is associated with a variety of conditions, such as obesity, inflammatory bowel diseases, and cancer. Some of the benefits of gut bacteria include:
- Contributing to healthy immune function.
- Providing protection against viruses and harmful bacteria that enter the gut.
- Contributing to healthy digestion by extracting energy and nutrients from food.
The variety of species and strains of bacteria living in the gut changes throughout life according to age, diet, and certain medications, including antibiotics. Therefore, it is impossible to determine exactly what constitutes a normal gut microbiome.3,4 As the same 2011 article in the Journal of Clinical Gastroenterology explains:
“It has not been possible to determine what the [microbiome] is at any given time in a healthy individual that is varying their diet. Furthermore, once medications and drugs are taken for various clinical reasons, such as transient infections, the [microbiome] may be altered for a lengthy period of time.”3
What Is the Relationship Between Gut Bacteria and Acne?
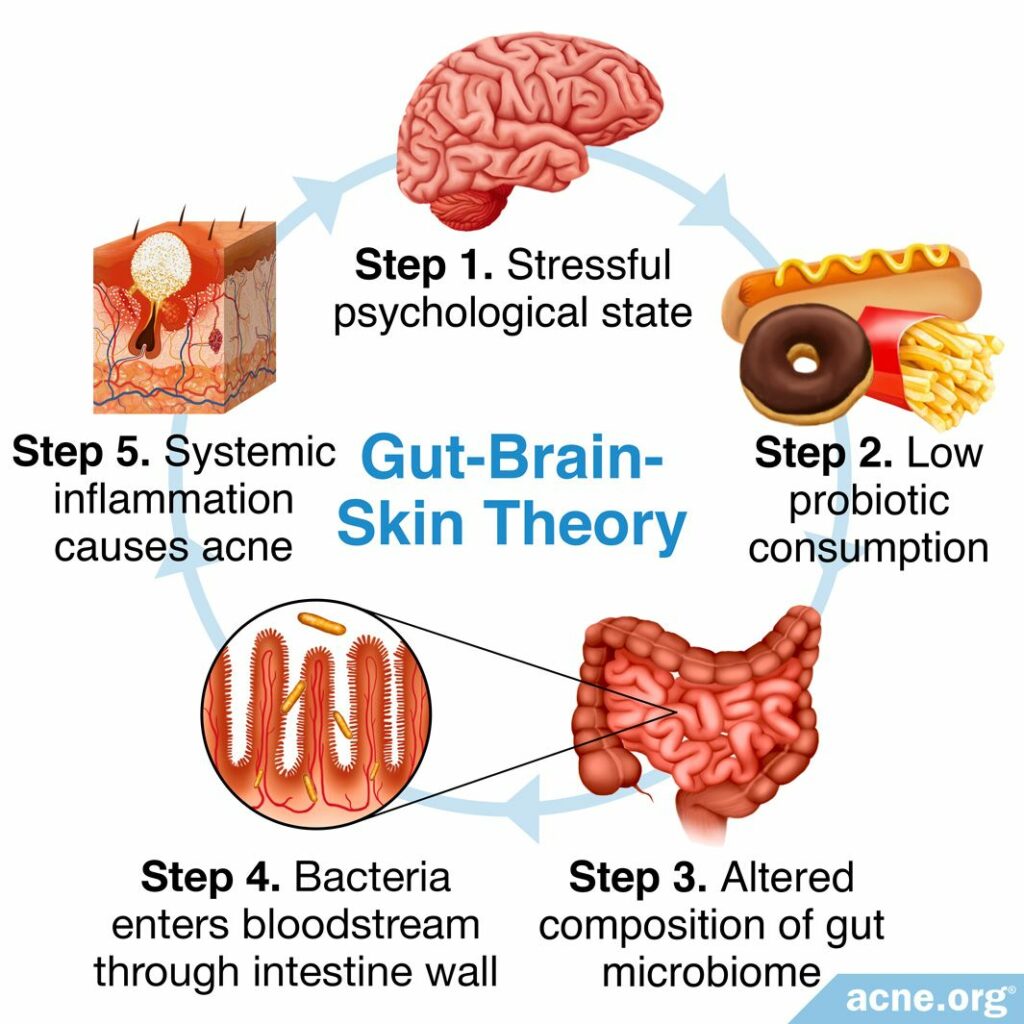
According to a theory called the Gut-Brain-Skin theory, stressful psychological states such as depression, worry, and anxiety can change the composition of the gut microbiome. This change increases the likelihood of a phenomenon called intestinal permeability, which is the ability for substances such as bacteria to pass through the intestinal wall into the bloodstream. As the bacteria move through the body into the bloodstream, the body fights back through creating inflammation.5,6 Acne is at its core an inflammatory disease, so it makes common sense that this might lead to more acne.
Several studies have found increased intestinal permeability in about two-thirds of acne patients, lending credibility to the Gut-Brain-Skin theory.5,7
Expand to see details of research

A 2014 article in the journal Beneficial Microbes reviewed two such studies. A century-old 1916 study found that 66% of a group of acne patients showed evidence of bacteria in the bloodstream that are found normally in the stool, suggesting that the intestinal walls in these patients were weak. No one in the control group, consisting of patients without acne, had such bacteria in their bloodstream.
Similarly, a 1983 study found that 65% of acne patients showed evidence of a toxin related to E. coli in the bloodstream, bacteria which normally is present in stool. Again, none of the patients without acne had this toxin in their bloodstream. The authors concluded, “intestinal permeability is a potential issue for many acne patients.”5
Probiotics Help Balance Gut Bacteria
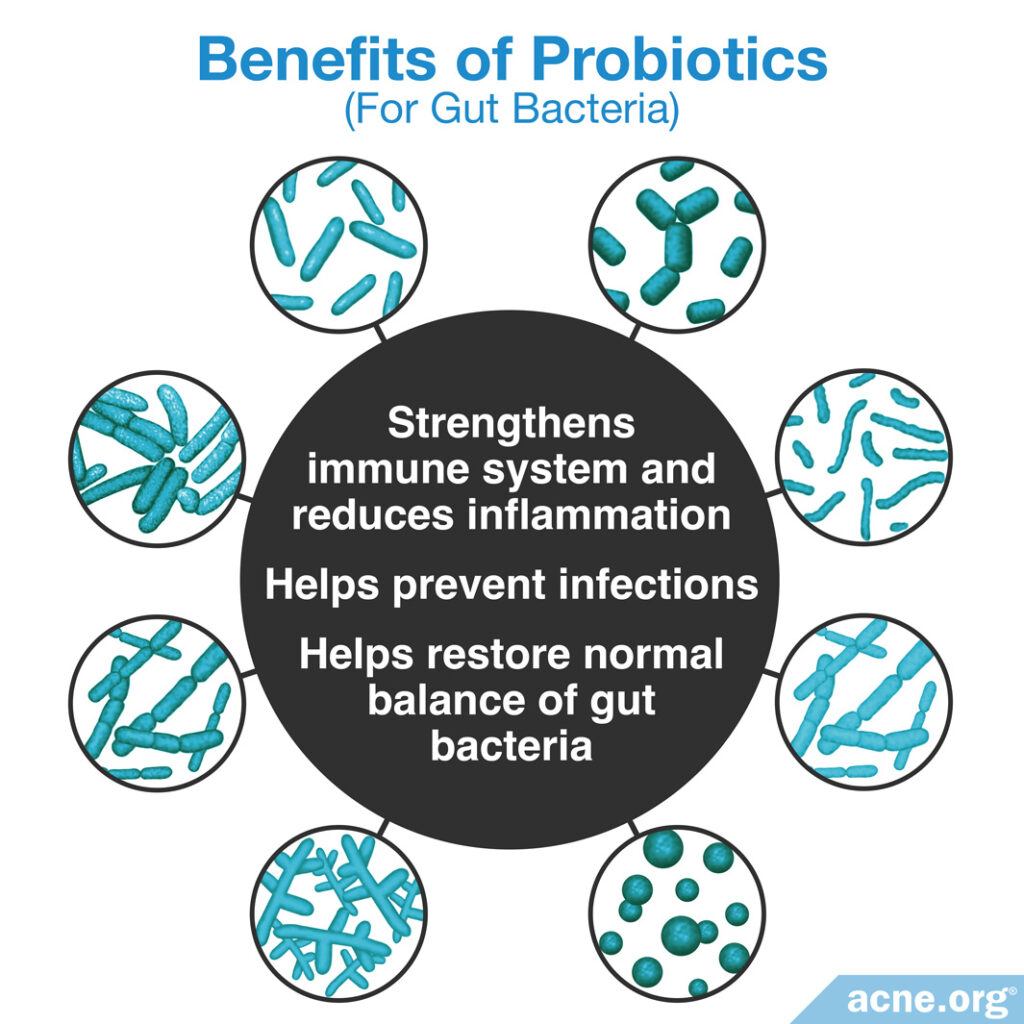
Probiotics can have an effect on the population of bacteria living in the gut and help to preserve a normal balance of the gut microbiome. In doing so, scientists believe that they might:
- Strengthen the immune system: The immune system regulates inflammation. Remember, acne is an inflammatory disease, so a strong immune system is important.
- Help prevent infections: Since acne is in part a bacterial infection in the skin, this is interesting.
- Help restore the normal balance of gut bacteria: This is particularly important after antibiotic administration, which kills beneficial bacteria along with the targeted harmful bacteria.8-10
Probiotics can be found in small amounts in certain foods, particularly in fermented foods such as cultured yogurt, tempeh, sauerkraut, and miso, and in larger amounts in manufactured dietary supplements. Interestingly, scientists do not call the beneficial bacteria that naturally live in the body probiotics; they reserve this label for beneficial bacteria that are administered through food and oral and topical supplements.9
There is still much that researchers do not know about probiotics. For one thing, there are many different strains of probiotic bacteria, and each has a different effect on the human body.
Probiotic supplements often contain many different strains, and different formulations of probiotic supplements contain different combinations of strains. Furthermore, probiotics can have different effects depending on the condition or disease that they treat. Therefore, we cannot generalize about exactly what probiotics do in the body: different strains and combinations of strains do not give the same effects. This is an area of ongoing research.
Expand to read how probiotics might help with various illnesses
The following is a list of ailments that might be suitable targets for probiotic supplementation, and the proposed mechanisms for how probiotics might alleviate the ailment:
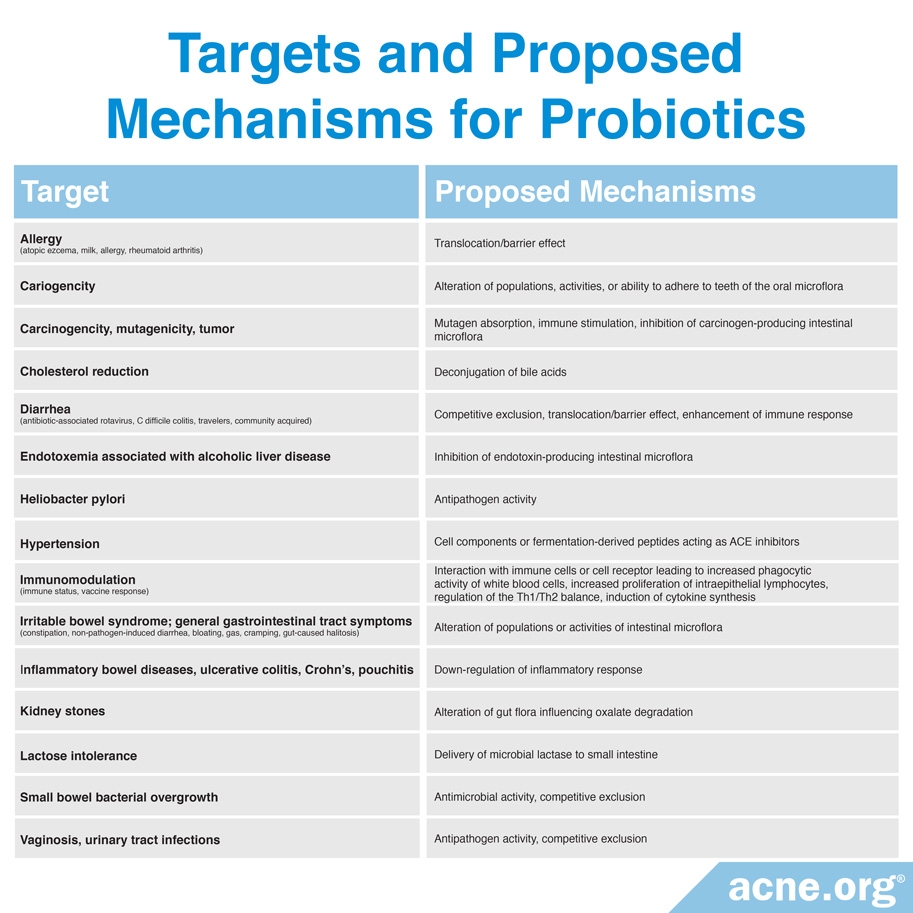
You can see there are many ailments which researchers try to treat using probiotics through different proposed mechanisms. As a 2003 article in the journal Nutrition Reviews explains:

“Much remains to be learned about the role of probiotics in human health. This is clearly an emerging area of science and one requiring confirmation of efficacy and mechanisms of action in controlled studies. However, the cumulative information that does exist has begun to establish a credible hypothesis about the role of probiotics in enhancing human health.”9
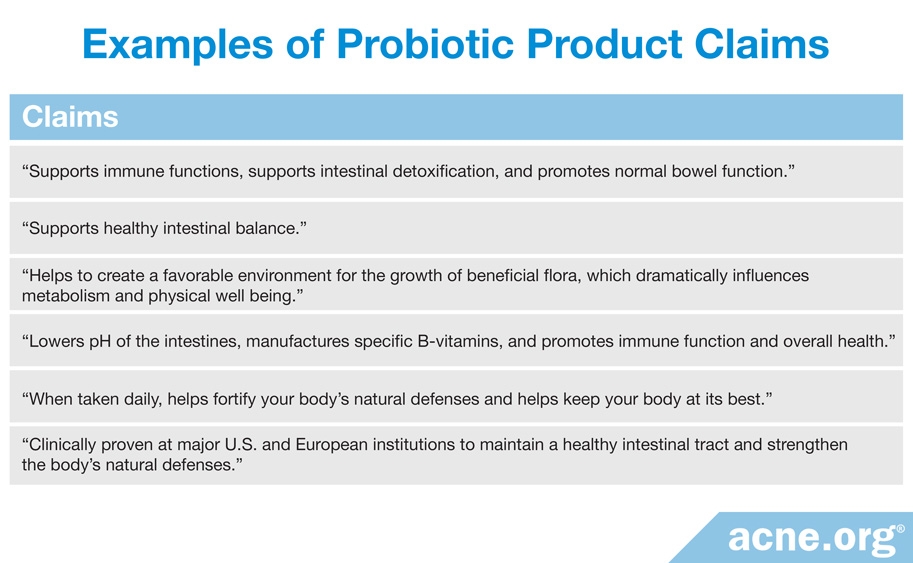
The table below shows claims probiotic manufacturers make and the related probiotic product. However, keep in mind that supplement claims are unregulated by the FDA.
Do Probiotics Help Acne?
Several studies, using a variety of different probiotic strains, have shown positive effects on acne.6,11-14
The studies also show that probiotics might help:
- Restore a healthy skin barrier function: People with acne tend to have an impaired skin barrier function, so this is intriguing.
- Reduce skin oil production: Generally speaking, less skin oil means less acne.
As a side note, taking probiotics at the same time as taking oral antibiotics may also help people tolerate the antibiotic better.6,11-13 This is relevant to acne because oral antibiotics are sometimes prescribed to treat acne.
Expand to read details of studies

A 2011 article in the journal, Gut Pathogens, reviewed two such studies. In a 1961 study, scientists gave acne patients a probiotic containing Lactobacillus strains and found that 80% of the patients had at least some improvement in their acne.
A 1987 study found that acne patients who took a probiotic supplement containing L. acidophilus and Bifidobacterium bifidum strains along with an antibiotic not only showed improvement in their acne but also tolerated the antibiotic better.6

A 2011 study in the European Journal of Dermatology found in the lab that a probiotic containing Lactobacillus paracasei reduced skin inflammation and accelerated recovery of the skin’s protective barrier.11

A 2013 study in the Journal of Cutaneous Medicine and Surgery examined the effect of a probiotic containing a combination of Lactobacillus acidophilus, Lactobacillus delbrueckii (subspecies bulgaricus), and Bifidobacterium bifidum on acne. This study divided acne patients into three groups: patients receiving only the probiotic, patients receiving only an antibiotic, and patients receiving both the probiotic and antibiotic. The researchers found that acne improved in all patients after four weeks but that after eight weeks, the patients who had received both the probiotic and antibiotic had the most improvement in their acne and, in addition, tolerated the antibiotic better. They concluded, “Probiotics may be considered a therapeutic option or adjunct for acne vulgaris by providing a synergistic anti-inflammatory effect with systemic antibiotics while also reducing potential adverse events secondary to chronic antibiotic use.”12

As we can see from these studies, there is some evidence that systemic probiotic supplementation might be beneficial in treating acne. According to a 2014 article in the Journal of the American Academy of Dermatology,“One of the potential benefits that systemic probiotics may offer is the reduction of inflammation in acne…Probiotics may also decrease sebum [skin oil] content, which can lead to lower…colonization by C. acnes and therefore decrease inflammation.”13

A 2019 study published in the Open Access Macedonian Journal of Medical Sciences supports the idea that probiotics might reduce inflammation in people with acne. The study included 33 people with acne who took a probiotic once a day for 30 days. The probiotic contained 5 different species of beneficial bacteria, including Lactobacillus acidophilus. The researchers measured the amounts of anti-inflammatory substances in the participants’ blood before and after the course of probiotic treatment. The scientists found that after taking the probiotics, the participants had significantly higher levels of anti-inflammatory substances in their blood. Since inflammation is the process underpinning all of acne, anything that stimulates the body to produce more anti-inflammatory substances might help keep acne in check. Accordingly, the researchers wrote, “Probiotic [sic] are useful for acne because they can help inflammatory regulation.”14
Taking Probiotics after Taking Antibiotics
Oral antibiotics can have profound effects on the bacteria living in the gut. Numerous studies have shown that taking oral antibiotics results in changes in the gut microbiome, including a loss of diversity in bacterial species and strains, that can last anywhere from 6 months to 2 years. This is because antibiotics not only kill the particular bacteria that they were prescribed for, but also many other species and strains of bacteria.15 This is why probiotics may be especially beneficial after taking oral antibiotics.
What about Topical Probiotics?

While most of the time we think of probiotics as something we ingest orally, some research provides evidence that applying probiotics topically might also improve acne.16-18
Expand to read details of research

A 2009 study in the Journal of Microbiology found that a lotion containing a probiotic called CBT SL-5 performed significantly better than a lotion not containing a probiotic in reducing inflammatory acne lesions.16
A 2018 article in the International Journal of Dermatology reviewed recent evidence suggesting that topical probiotics might help with acne.17 According to the authors of the article, most studies in this area tested topical probiotics in a lab rather than on people with acne. For example, in several studies, researchers grew acne bacteria in a petri dish and then applied probiotics to see whether this would block the growth of acne bacteria.
These studies found that some probiotics may reduce the growth of acne bacteria in the lab, but we do not know whether they would work the same way when applied directly to people’s skin. The authors of the review article wrote, “[M]ore detailed research should be performed in order to prove the real efficacy and safety of probiotics in these situations.”17

A 2019 article in the journal Experimental Dermatology also reviewed research on topical antibiotics for the treatment of acne. The authors of the article noted that a few studies have tested topical antibiotics directly on people with acne and shown promising results. These studies found that cultures of the bacteria Lactobacillus plantarum and Enterococcus faecalis helped acne patients by reducing the number of acne lesions, decreasing skin redness, and strengthening the skin barrier. However, the authors of the review article observed that each study used a different method, so it is difficult to compare their results and draw overall conclusions.18
Buying the Right Probiotic
Despite some promising early results suggesting that probiotics might help with acne, we should remember that probiotics are not regulated by the U.S. Food and Drug Administration (FDA). In other words, the quality of the oral and topical probiotics currently on the market may vary widely, and some of them may not actually contain the cultures they claim.19
Therefore, when you are buying a probiotic, do your research and make sure you’re buying from a reputable source.
The Bottom Line
Maintaining the balance of gut bacteria plays an important role in the health of the body. When this balance is disrupted, it can lead to increased inflammation and possibly to the formation of acne. Probiotics can positively impact the balance of bacteria in the gut, which may, in turn, benefit acne sufferers by (1) reducing inflammation, (2) decreasing skin oil production, and (3) helping to lessen some of the negative side effects of antibiotics.
It is best not to look for dramatic improvement in your acne from simply taking probiotics, but, especially if you are on oral antibiotics or have recently finished a course of oral antibiotics, taking probiotics may help.
References
- Das, S. & Reynolds, R. V. Recent advances in acne pathogenesis: implications for therapy. Am. J. Clin. Dermatol. 15, 479 – 488 (2014). https://www.ncbi.nlm.nih.gov/pubmed/25388823
- Goodman, G. J. Post-acne scarring: a short review of its pathophysiology. Australas. J. Dermatol. 42, 84 – 90 (2001). https://www.ncbi.nlm.nih.gov/pubmed/11309028
- Floch, M. H. Intestinal microecology in health and wellness. J. Clin. Gastroenterol. 45 Suppl, S108 – 110 (2011). https://www.ncbi.nlm.nih.gov/pubmed/21992947
- Lozupone, C. A., Stombaugh, J. I., Gordon, J. I., Jansson, J. K. & Knight, R. Diversity, stability and resilience of the human microbiota. Nature 489, 220 – 230 (2012). https://www.ncbi.nlm.nih.gov/pubmed/22972295
- Bowe, W., Patel, N. B. & Logan, A. C. Acne vulgaris, probiotics and the gut-brain-skin axis: from anecdote to translational medicine. Benef. Microbes 5, 185 – 199 (2014). https://www.ncbi.nlm.nih.gov/pubmed/23886975
- Bowe, W. P. & Logan, A. C. Acne vulgaris, probiotics and the gut-brain-skin axis – back to the future? Gut. Pathog. 3, 1 (2011). https://www.ncbi.nlm.nih.gov/pubmed/21281494
- Sánchez-Pellicer, P., Navarro-Moratalla, L., Núñez-Delegido, E., Ruzafa-Costas, B., Agüera-Santos, J. & Navarro-López, V. Acne, microbiome, and probiotics: The gut-skin axis. Microorganisms 10, 1303-1326 (2022). https://pubmed.ncbi.nlm.nih.gov/35889022/
- Million, M., Lagier, J. C., Yahav, D. & Paul, M. Gut bacterial microbiota and obesity. Clin. Microbiol. Infect. 19, 305 – 313 (2013). https://www.ncbi.nlm.nih.gov/pubmed/23452229
- Sanders, M. E. Probiotics: considerations for human health. Nutr. Rev. 61, 91 – 99 (2003). https://www.ncbi.nlm.nih.gov/pubmed/12723641
- Baralić, K., Živančević, K., Bozic, D. & Đukić-Ćosić, D. Probiotic cultures as a potential protective strategy against the toxicity of environmentally relevant chemicals: State-of-the-art knowledge. Food Chem. Toxicol. 172, 113582 (2023). https://pubmed.ncbi.nlm.nih.gov/36581092/
- Philippe, D., Blum, S. & Benyacoub, J. Oral Lactobacillus paracasei improves skin barrier function recovery and reduces local skin inflammation. Eur. J. Dermatol. 21, 279 – 280 (2011). https://www.ncbi.nlm.nih.gov/pubmed/21489918
- Jung, G. W., Tse, J. E., Guiha, I. & Rao, J. Prospective, randomized, open-label trial comparing the safety, efficacy, and tolerability of an acne treatment regimen with and without a probiotic supplement and minocycline in subjects with mild to moderate acne. J. Cutan. Med. Surg. 17, 114 – 122 (2013). https://www.ncbi.nlm.nih.gov/pubmed/23582165
- Baquerizo Nole, K. L., Yim, E. & Keri, J. E. Probiotics and prebiotics in dermatology. J. Am. Acad. Dermatol. 71, 814 – 821 (2014). https://www.ncbi.nlm.nih.gov/pubmed/24906613
- Rahmayani, T., Putra, I. B. & Jusuf, N. K. The effect of oral probiotic on the interleukin-10 serum levels of acne vulgaris. Open Access Maced. J. Med. Sci. 7, 3249-3252 (2019). https://pubmed.ncbi.nlm.nih.gov/31949525/
- Becattini, S., Taur, Y. & Pamer, E. G. Antibiotic-induced changes in the intestinal microbiota and disease. Trends Mol. Med. 22, 458 – 478 (2016). https://www.ncbi.nlm.nih.gov/pubmed/27178527
- Kang, B. S. et al. Antimicrobial activity of enterocins from Enterococcus faecalis SL-5 against Propionibacterium acnes, the causative agent in acne vulgaris, and its therapeutic effect. J. Microbiol. 47, 101 – 109 (2009). https://www.ncbi.nlm.nih.gov/pubmed/19229497
- Mottin, V. H.M. & Suyenaga, E. S. An approach on the potential use of probiotics in the treatment of skin conditions: acne and atopic dermatitis. Int. J. Dermatol. 57, 1425-1432 (2018). https://www.ncbi.nlm.nih.gov/pubmed/29676446
- Knackstedt, R., Knackstedt, T. & Gatherwright, J. The role of topical probiotics on skin conditions: A systematic review of animal and human studies and implications for future therapies. Exp. Dermatol. 29, 15-21 (2019). https://www.ncbi.nlm.nih.gov/pubmed/31494971
- Lee, G. R., Maarouf, M., Hendricks, A. J., Lee, D. E. & Shi, V. Y. Topical probiotics: the unknowns behind their rising popularity. Dermatol. Online J. 25, 5 (2019). pii: 13030/qt2v83r5wk. https://www.ncbi.nlm.nih.gov/pubmed/31220895
 Acne.org Products
Acne.org Products