A Whitehead Is a Small, White or Skin-colored Clogged Pore

The Essential Info
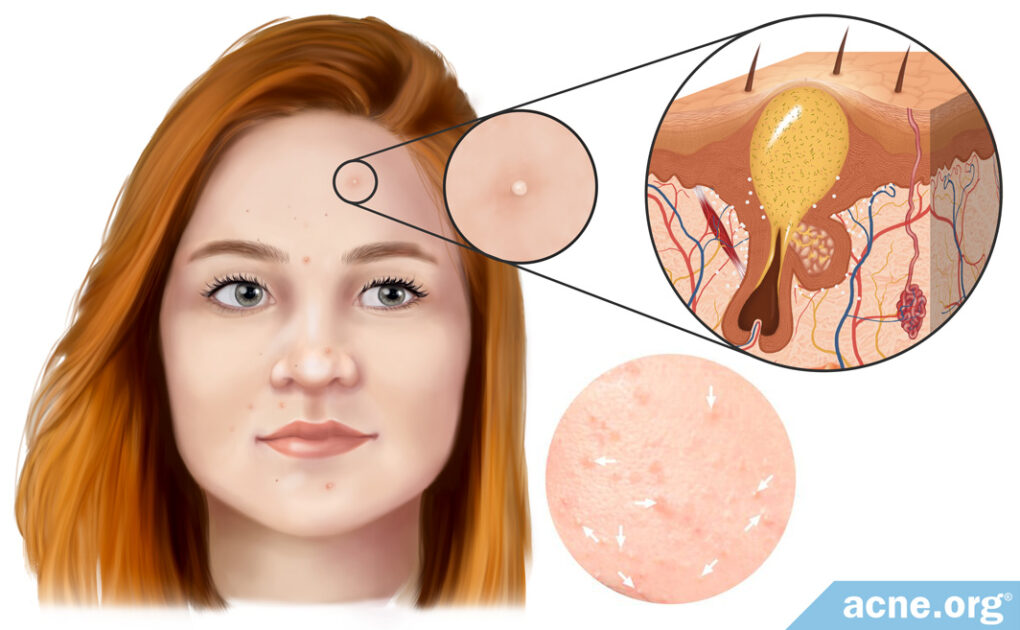
Whiteheads, also known as closed comedones, are small, non-inflammatory, white or skin-colored lesions that most often develop on the face, particularly on the nose and around the mouth. They are most common during teen years, but can be seen at any age.
These lesions develop when a pore becomes clogged and begins to fill up with trapped skin oil. A whitehead remains on the skin for only a few days, before either going away on its own, or developing into an inflammatory lesion, such as a papule, pustule, nodule, or cyst.
Not to Be Confused with a Pustule: When people think of a “whitehead” they often think of a red, sore lesion with a white or yellow center. However, this is not a whitehead, and instead is called a pustule. A whitehead is not red or sore, and is smaller than a pustule.

The Science
Whiteheads are small, white or skin-colored clogged pores (comedones) that mainly form on the nose and in the area around the mouth, but can also be found elsewhere on the face, neck, and body.
Dermatologists classify whiteheads as “non-inflammatory” acne lesions because they are not red, swollen, or painful.
Whiteheads form when a pore becomes completely clogged and skin oil gets trapped inside. Once a whitehead develops on the skin, it remains for several days, after which it either heals on its own or develops into an inflammatory acne lesion that becomes red and sore. If a whitehead heals on its own, it is usually completely gone within 12 days.1
Most people develop whiteheads in their teenage or young adult years, but developing them at a younger or older age is also common.2-4
Some people have bumps on their skin that look like whiteheads and stick around in the same spot for weeks or even months. These bumps are called milia, and they commonly occur on the nose and upper cheeks.5 Milia are harmless and unrelated to acne.
How Whiteheads Develop

Whiteheads develop in two steps:
Step 1 – Blockage of pore & formation of a microcomedone
All acne lesions begin with microscopic hair follicles, often referred to as pores, in the skin. Attached to these pores are glands, called sebaceous glands, that produce skin oil, called sebum. Normally, after the sebaceous glands produce sebum, the sebum slowly moves up the pore toward the surface of the skin where it is expelled onto the skin’s surface. However, in acne, the opening to the pore becomes blocked with skin cells, and this results in the development of a clogged pore, called a comedone. When the pore first becomes blocked, the lesion is called a microcomedone, and cannot be seen with the naked eye.
Step 2 – Formation of whitehead (comedone)
After a microcomedone forms, the sebum, which is unable to escape the pore, begins to build up. Eventually, the microcomedone becomes larger due to this buildup of sebum. When the microcomedone grows large enough to be visible to the naked eye, it is called a comedone.
There are two types of comedones, whiteheads and blackheads.
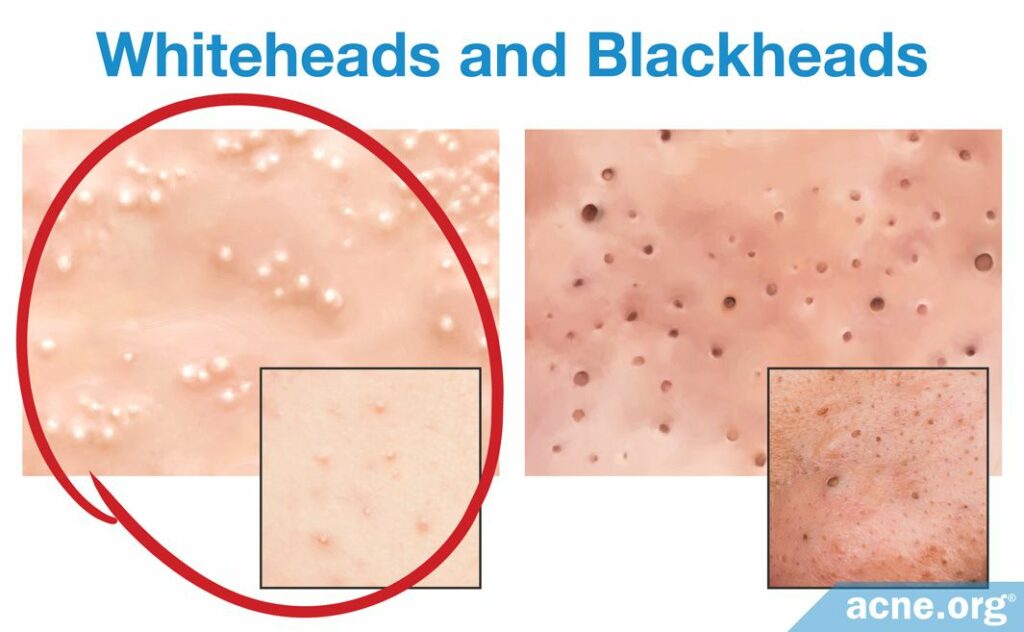
- Whiteheads: Whiteheads are also called closed comedones, because the opening of the pore is completely blocked, and nothing can enter or escape. When the sebum cannot escape, it accumulates, and this buildup of sebum gives the whitehead its characteristic white or skin-colored hue. Once developed, a whitehead remains on the skin for 3 – 12 days. After this time, it will either heal on its own, which occurs in about 25% of whiteheads, or develop into an inflammatory acne lesion that becomes red and sore, which occurs in about 75% of whiteheads.
- Blackheads: Blackheads are also called open comedones, because the opening of the pore is not completely blocked, allowing for air to penetrate into the pore. When oxygen in the air enters the pore, it undergoes a chemical reaction that gives rise to the characteristic dark brown or black color. Contrary to popular belief, the dark color of a blackhead is not due to dirt, but due to oxidation (chemical reaction with oxygen) of the pigment melanin, which is found in sebum. Once developed, a blackhead can remain on the skin for several weeks or even months.2-4,6-8
What Causes a Whitehead?
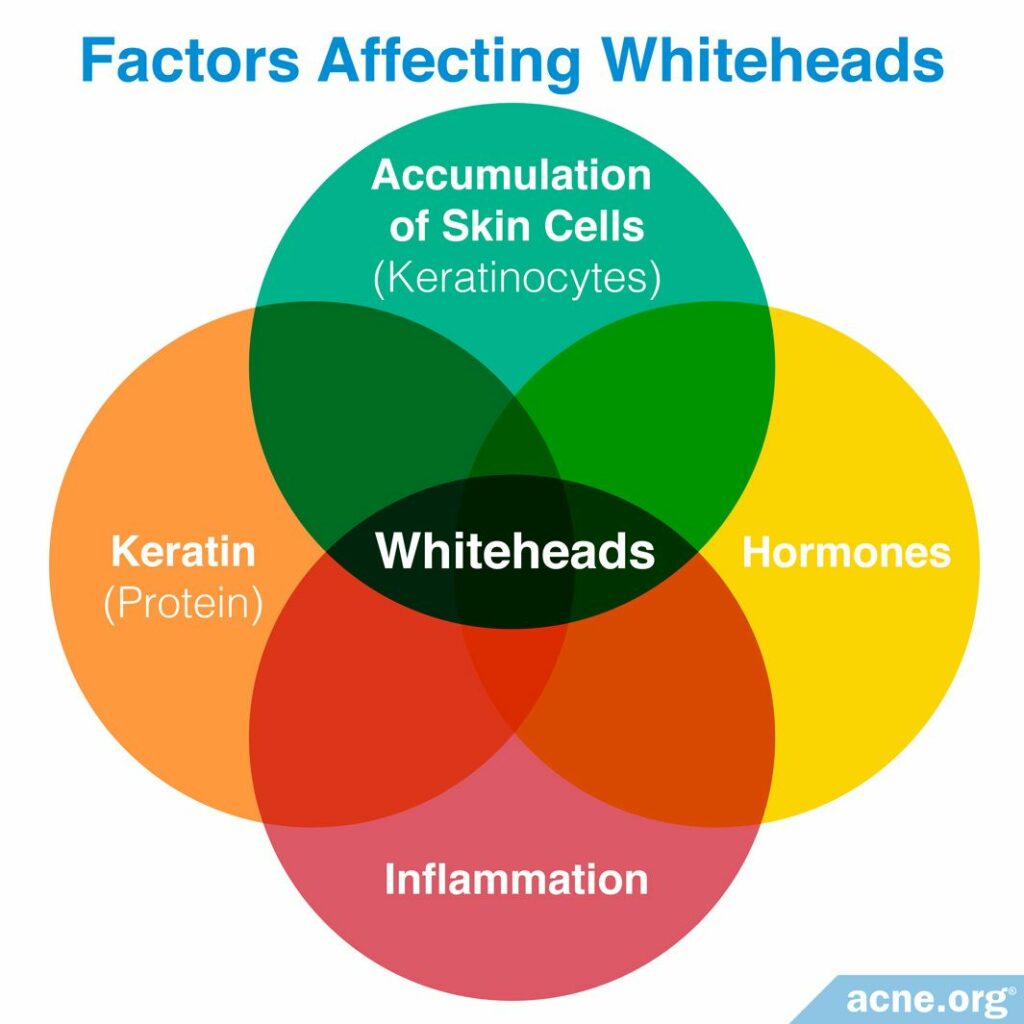
Several factors are thought to contribute to the development of whiteheads, including:
- Inflammation: Although whiteheads are classified as “non-inflammatory” acne lesions because they are not red, swollen, or painful, researchers have found some inflammatory molecules in whiteheads. One study discovered that an inflammatory molecule called interleukin 1 (IL-1) is found in up to 76% of comedones, including whiteheads and blackheads. This suggests that although whiteheads are not red, swollen, or sore, there is almost always inflammation present in them that likely affects their development.
- Hormones: Hormones, especially androgens, which are male hormones present in both males and females, play a vital role in the development of acne. In fact, without hormones, acne would not exist. An increase in hormones leads to the development of all acne lesions, including whiteheads.
- Accumulation of skin cells: Skin cells, known as keratinocytes, are in a constant state of renewal. In healthy skin, they are produced within the skin, slowly move toward the skin surface, and flake off in a balanced way. In acne, the balance is off and these skin cells do not die on time and flake off as they should. This causes an accumulation of both new skin cells and dead skin cells along the wall of the pore. This accumulation leads to a clogged pore and development of comedones, including both whiteheads and blackheads.
- Keratin: Keratin is a sticky protein produced by keratinocytes that causes the keratinocytes to stick together, preventing the cells from flaking off the skin as they should, leading to a clogged pore.9
In addition, the acne bacteria called C. acnes may also play a part in the development of whiteheads. Researchers are still trying to determine at what point in the formation of an acne lesion these bacteria start to overgrow. One study found that even pores that are just beginning to clog may already contain over-active C. acnes bacteria. However, it is unclear exactly what role these bacteria may play in turning a pore that is starting to clog into a bona fide acne lesion.10
Conclusion
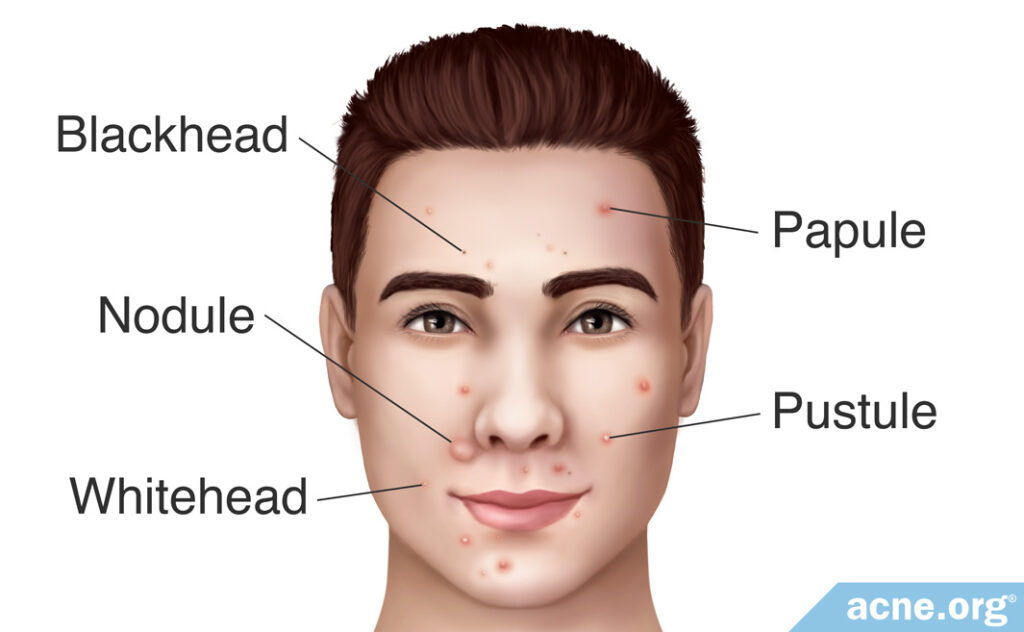
Whiteheads, also known as closed comedones, are small, non-inflammatory, white or skin-colored lesions that most often develop on the face. These lesions develop when a pore becomes clogged with skin cells, and this clogged pore begins to fill up with sebum (skin oil). A whitehead normally remains on the skin for only a few days, before either healing on its own, or developing into an inflammatory lesion, such as a papule, pustule, nodule, or cyst.
References
- Cunliffe, W. J, Holland, D. B & Jeremy, A. Comedone formation: etiology, clinical presentation, and treatment. Clin Dermatol 22, 367-74 (2004). https://pubmed.ncbi.nlm.nih.gov/15556720/
- Do, T. et al. Computer-assisted alignment and tracking of acne lesions indicate that most inflammatory lesions arise from comedones and de novo. J Am Acad Dermatol 58, 603 – 608 (2008). https://www.ncbi.nlm.nih.gov/pubmed/18249468
- Thiboutot, D. The role of follicular hyperkeratinization in acne. J Dermatolog Treat 11, 5 – 8 (2000). https://www.tandfonline.com/doi/abs/10.1080/095466300750163645
- Brogden, R. & Goa, K. Adapalene. Drugs 53, 511 – 519 (1997). https://www.ncbi.nlm.nih.gov/pubmed/9074847
- Ramli, R., Malik, A. S., Hani, A. F. & Jamil, A. Acne analysis, grading and computational assessment methods: an overview. Skin Res Technol 18, 1-14 (2012). https://pubmed.ncbi.nlm.nih.gov/21605170/
- Kunachak, S. Laser treatment for acne vulgaris. Am J Cosmet Surg 12, 127 – 131 (1995). https://journals.sagepub.com/doi/10.1177/074880689501200206
- Saurat, J. Strategic targets in acne: the comedone switch in question. Dermatology 231, 105 – 111 (2015). https://www.ncbi.nlm.nih.gov/pubmed/26113292
- Orentreich, N. & Durr, N. The natural evolution of comedones into inflammatory papules and pustules. J Investig Dermatol 62, 316 – 320 (1974). https://core.ac.uk/download/pdf/82174419.pdf
- Tanghetti, E. The role of inflammation in the pathology of acne. J Clin Aesthet Dermatol 6, 27 – 35 (2013). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3780801/
- Josse, G., Mias, C., Le Digabel, J. et al. High bacterial colonization and lipase activity in microcomedones. Exp Dermatol 29, 168‐176 (2020). https://www.ncbi.nlm.nih.gov/pubmed/31863492
 Acne.org Products
Acne.org Products