It’s More about Ethnicity than Skin Color. Non-Caucasians Tend to Develop Raised Scars More Often than Caucasians, Likely for Genetic Reasons

The Essential Info
Raised scars include two types, which have complex names, but really aren’t that complex:
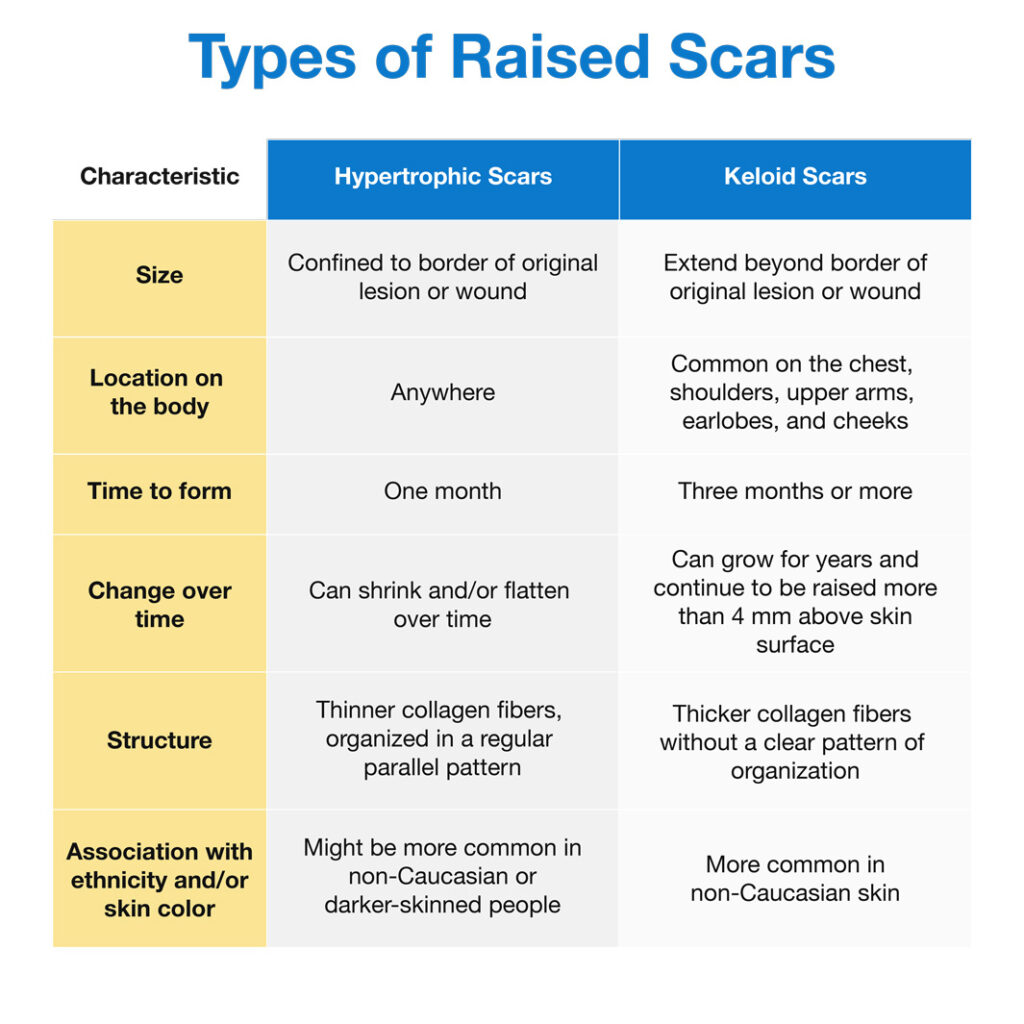
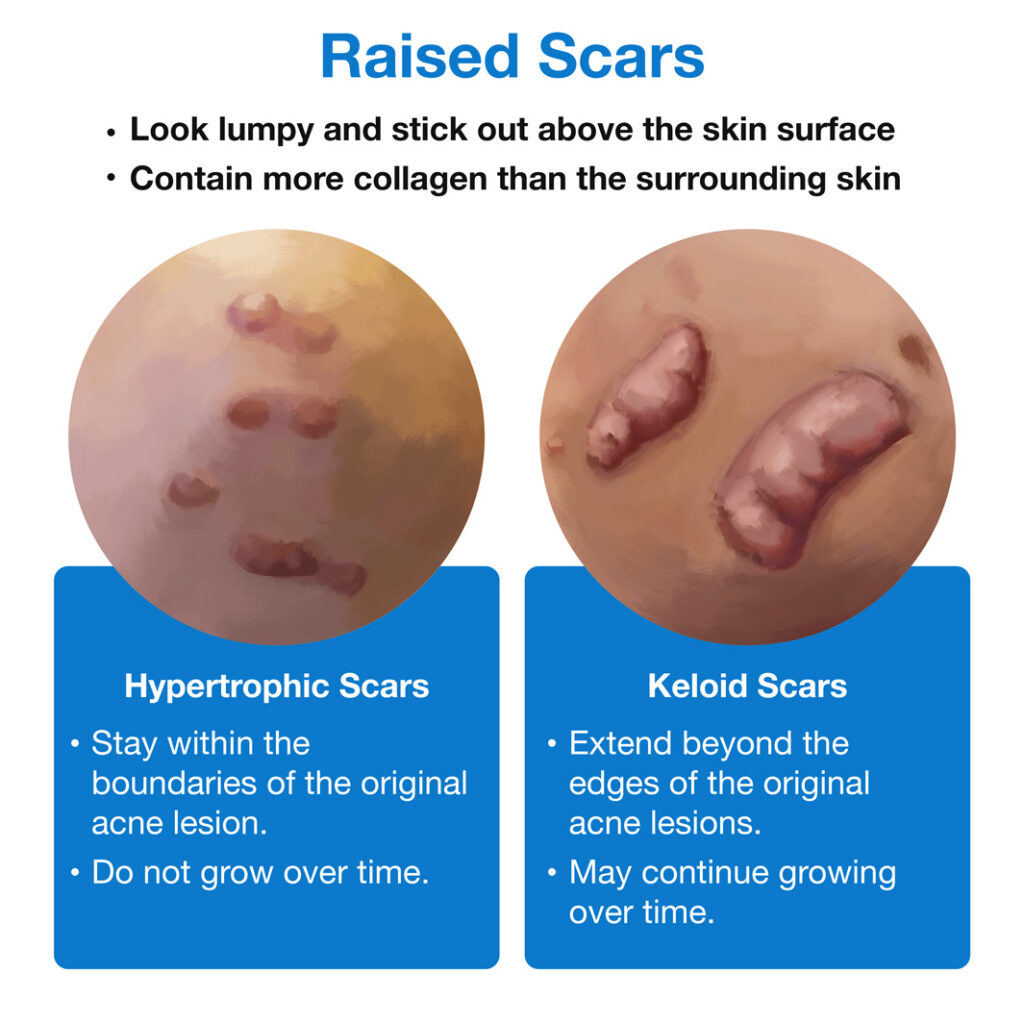
- Hypertrophic scars: These are raised scars that are the same size as the original acne lesion. Some research suggests hypertrophic scars might occur more often in non-Caucasian or darker-skinned people, but more evidence is needed.
- Keloid scars: These are raised scars that are larger than the original acne lesion. Studies show that keloids affect people of African descent most often, followed by people of Asian background, and then those of Hispanic background. In other words, non-Caucasians are more likely to develop keloid scars than Caucasians.
Hypertrophic scars:
Keloids:
Why they form: Emerging research suggests that raised scars form when inflammation goes into overdrive in deeper layers of the skin. Non-Caucasians may be genetically predisposed for this to happen, but scientists are just starting to identify some of the genes responsible.
What to do if you are prone to raised scars: Raised scars can be difficult to treat. Keloids in particular have a high chance of reappearing in the same spot. Do your best to prevent raised scars from forming by treating your acne early, and work closely with your dermatologist or plastic surgeon to develop a treatment plan for any raised scars you may already have.

The Science
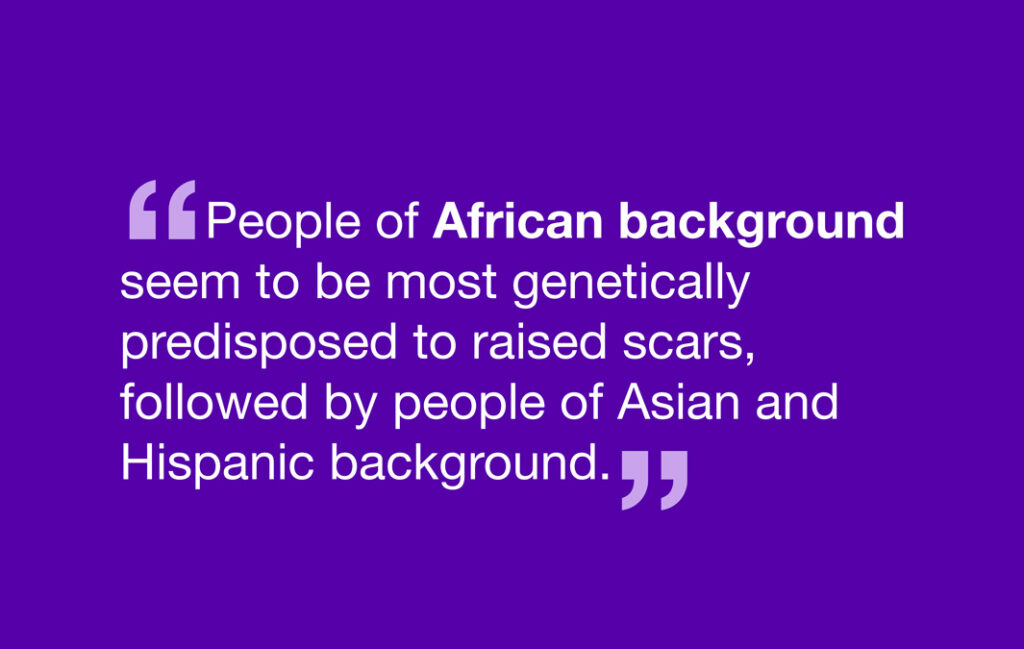
You may have heard that darker-skinned people are at greater risk for developing raised scars. However, research suggests that ethnic background rather than skin color makes certain people more prone to raised scars. Specifically, people of African background seem to be most genetically predisposed to raised scars, followed by people of Asian and Hispanic background.
Let’s take a look at the types of raised scars and who tends to be more prone to each type.
A Quick Primer on the Types of Raised Scars
When an acne lesion is healing, the body tries to fill in the spot where the lesion used to be with new skin. As part of this, the body produces collagen, a skin protein that helps fill in the hole. Raised scars result when the site of a healed acne lesion is filled in with too much new collagen. There are two types of raised scars:
- Hypertrophic scars: These scars do not go beyond the edges of the original acne lesion, and over time, they may shrink. A hypertrophic scar typically contains about 3 times more collagen than healthy skin does.
- Keloid scars: These scars extend beyond the edges of the original acne lesion. They tend not to shrink and can even grow over time. A keloid scar typically contains about 20 times more collagen than healthy skin does.1-3
Who Gets Raised Scars?
Risk factors for hypertrophic scars:
- Younger age: Hypertrophic scars tend to occur in people who are 11-30 years old, perhaps because younger people produce collagen at a faster rate compared to older people.1
- [Maybe] Darker skin: Some evidence suggests that non-Caucasians or people with darker skin may be more prone to developing hypertrophic scars than people with lighter skin. Scientists are investigating what anatomical and/or genetic differences might explain this.1
Risk factors for keloid scars:
- Younger age: Like hypertrophic scars, keloid scars are also more common in people who are 11-30 years of age than in older people.1
- Non-Caucasian ethnic background: Keloid scars are most common in people of African descent, followed by those of Asian descent and then those of Hispanic descent. In these ethnic groups, the incidence of keloids ranges from 4.5% to 16%. Caucasians are the least likely to develop keloid scars.2
- Family history: Studies show that a tendency to form keloids runs in families. For example, in identical twins, if one twin is prone to keloids, the other twin likely is as well. This points to genetic factors that probably predispose certain people to forming keloids.4-6
- Specific genes and genetic conditions: Scientists have already identified a few genes that may make a person prone to keloid scars. For example, one large family in Nigeria belonging to the Yoruba ethnic group has a gene called ASAH1 that is linked to keloid formation.4 Future research will likely reveal many more genes that predispose people to keloids. In addition, people with rare genetic conditions like Rubinstein-Taybi syndrome and Goeminne syndrome are more likely to develop keloid scars.6
- Traumatic injury or acne: One study found that among 159 patients with keloid scars in Nigeria, the top two causes of keloids were traumatic injuries and acne. In fact, one-fifth of the keloids had formed as a result of acne.7
Acne Keloidalis Nuchae (AKN): A Special Type of Neck Acne That May Lead to Keloid Scars and Occurs Most Often in African-American Males
Some people can develop a special type of acne on the back of the neck called acne keloidalis nuchae, or AKN for short. This type of acne most often strikes African-American males and can be triggered by ongoing skin irritation, such as from close shaves and collars rubbing against the neck. Other triggers may include heat, humidity, skin infections, and certain medications. AKN appears as papules and pustules on the back of the neck which may end up leaving keloid scars.8
If you think you may have AKN, try the following to reduce your chances of keloid scars:
- Ask your barber to be super gentle and not go over any area of skin more than once if possible.
- Ask your barber not to shave the hair on the back of the neck closer than ¼ inch.
- Treat the affected skin with benzoyl peroxide followed by glycolic acid.
Treatment Options for Hypertrophic Scars and Keloids
While there are a number of options for treating raised scars, none of them can fully remove raised scars. Keloids in particular have a tendency to form again in the same spot after treatment.
Therefore, the best strategy with these types of scars is prevention. Do your best to prevent raised scars from forming by treating your acne early and not picking at any existing lesions.
When it comes to raised scars that have already formed, it is important to do your research on the treatment options and work closely with your dermatologist to choose the best scar repair method for your case.1,2,9-11 Experts caution that a poorly chosen treatment can actually make keloids worse. Therefore, according to a medical reference ebook on keloids, “If one has no idea what to do, the best advice is to leave the keloid alone.”2
Some options for treating raised scars include:
- Corticosteroids
- Surgical removal
- Cryotherapy
- Laser treatment
You can see a full list of treatment options here.
What Scientists Know so Far about Why Raised Scars Form
To understand why raised scars form, we need to take a quick look at the healing process. Just like any other skin damage, acne lesions heal in three stages:
- Inflammation: Inflammation begins in the earliest stages of acne and continues as an acne lesion starts to heal. We can see the signs of inflammation as redness, swelling, and pain at the lesion site. The purpose of inflammation is to summon cells that will clean up the damaged skin at the lesion and repair the skin. Prolonged inflammation during this stage may make a scar more likely.
- Cell proliferation: In this stage, many new skin cells grow (“proliferate”) to replace skin cells that were damaged in the acne lesion. At the same time, the skin starts to build a temporary “matrix,” which will later become the deeper layer of the skin. The protein collagen is an important building block of this new matrix.
- Too much collagen production during this stage can cause a raised scar: Excess collagen results in raised scars like hypertrophic and keloid scars.
- Too little collagen production during this stage can case an indented scar: A lack of collagen results in indented (atrophic) scars like icepick, boxcar, and rolling scars.12,13
- Remodeling: In this stage, the skin remodels the temporary matrix into a more permanent connective tissue that will ultimately form the deeper layer of the skin.14,15
Scientists think that a problem in the very first stage, inflammation, may send a lesion on the path to forming a raised scar. Since raised scars only form after deep skin damage, perhaps long-term inflammation in deep layers of the skin is what leads to raised scars. Some researchers speculate that weaker inflammation may cause hypertrophic scars while stronger inflammation may result in keloid scars.1,2,16
So why do some people’s acne lesions tend to heal with prolonged inflammation, resulting in raised scars? The answer may be genetics. People who are prone to raised scars may be more sensitive to skin injuries, so that such injuries trigger the production of too many inflammatory substances. Studies confirm that raised scars contain increased amounts of inflammatory substances called interleukins. Therefore, for people who are prone to raised scars, reducing inflammation in acne may be especially important.16
References
- Carswell, L. & Borger, J. Hypertrophic Scarring Keloids. [Updated 2020 Aug 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537058/
- McGinty, S. & Siddiqui, W. J. Keloid. [Updated 2020 Aug 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507899/
- Juckett, G. & Hartman-Adams, H. Management of keloids and hypertrophic scars. Am Fam Physician. 80, 253-60 (2009). https://pubmed.ncbi.nlm.nih.gov/19621835/
- Santos-Cortez, R. L. P., Hu, Y., Sun, F., Benahmed-Miniuk, F., Tao, J., Kanaujiya, J. K., Ademola, S., Fadiora, S., Odesina, V., Nickerson, D. A., Bamshad, M. J., Olaitan, P. B., Oluwatosin, O. M., Leal, S. M. & Reichenberger, E. J. Identification of ASAH1 as a susceptibility gene for familial keloids. Eur J Hum Genet. 25, 1155-1161 (2017). https://pubmed.ncbi.nlm.nih.gov/28905881/
- Glass, D. A. 2nd. Current understanding of the genetic causes of keloid formation. J Investig Dermatol Symp Proc. 18, S50-S53 (2017). https://pubmed.ncbi.nlm.nih.gov/28941494/
- Halim, A. S., Emami, A., Salahshourifar, I. & Kannan, T. P. Keloid scarring: understanding the genetic basis, advances, and prospects. Arch Plast Surg. 39, 184-9 (2012). https://pubmed.ncbi.nlm.nih.gov/22783524/
- Belie, O., Ugburo, A. O. & Mofikoya, B. O. Demographic and clinical characteristics of keloids in an urban center in Sub-Sahara Africa. Niger J Clin Pract. 22, 1049-1054 (2019). https://pubmed.ncbi.nlm.nih.gov/31417046/
- Al Aboud, D. M. & Badri, T. Acne Keloidalis Nuchae. [Updated 2020 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459135/
- Lee, H. J. & Jang, Y. J. Recent Understandings of Biology, Prophylaxis and treatment strategies for hypertrophic scars and keloids. Int J Mol Sci. 19, 711 (2018). https://pubmed.ncbi.nlm.nih.gov/29498630/
- Betarbet, U. & Blalock, T. W. Keloids: A review of etiology, prevention, and treatment. J Clin Aesthet Dermatol. 13, 33-43 (2020). https://pubmed.ncbi.nlm.nih.gov/32308783/
- Wang, Z. C., Zhao, W. Y., Cao, Y., Liu, Y. Q., Sun, Q., Shi, P., Cai, J. Q., Shen, X. Z. & Tan, W. Q. The roles of inflammation in keloid and hypertrophic scars. Front Immunol. 11, 603187 (2020). https://pubmed.ncbi.nlm.nih.gov/33343575/
- Fabbrocini, G., Annunziata, M. C., D’Arco, V., De Vita, V., Lodi, G., Mauriello, M. C., Pastore, F. & Monfrecola, G. Acne scars: pathogenesis, classification and treatment. Dermatol Res Pract. 2010, 893080 (2010). https://pubmed.ncbi.nlm.nih.gov/20981308/
- Fife, D. Practical evaluation and management of atrophic acne scars: tips for the general dermatologist. J Clin Aesthet Dermatol. 4, 50-7 (2011). https://pubmed.ncbi.nlm.nih.gov/21909457/
- Ozgok Kangal, M. K. & Regan, J. P. Wound Healing. [Updated 2020 Jul 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK535406/
- Guo, S. & Dipietro, L. A. Factors affecting wound healing. J Dent Res. 89, 219-29 (2010). https://pubmed.ncbi.nlm.nih.gov/20139336/
- Ogawa, R. Keloid and hypertrophic scars are the result of chronic inflammation in the reticular dermis. Int J Mol Sci. 18, 606 (2017). https://pubmed.ncbi.nlm.nih.gov/28287424/
- Nishiguchi, M. A., Spencer, C. A., Leung, D. H. & Leung, T. H. Aging suppresses skin-derived circulating SDF1 to promote full-thickness tissue regeneration. Cell Rep.24, 3383-3392.e5 (2018). Erratum in: Cell Rep.25, 3898 (2018). https://pubmed.ncbi.nlm.nih.gov/30257200/
 Acne.org Products
Acne.org Products