Acne Scars on the Body Tend to Be Fewer but More Severe. Treatment Is the Same as for Scars on the Face.

The Essential Info
While acne scars on the body tend to be less numerous than on the face, they can often be more severe. If you would like to seek treatment for acne scars on your body, follow these recommendations:
- Make sure your skin is clear of acne before starting scar treatment.
- Protect your skin from the sun, as the sun’s rays can make scars darker and more visible.
- Research and compare scar treatment options, keeping in mind that the best results sometimes come from combining several different scar treatments.
- If you are taking isotretinoin or have recently stopped taking it, talk to your doctor to determine if you need to wait before starting scar treatment.
- Design a personalized scar treatment plan together with a trusted dermatologist or plastic surgeon who specializes in acne scar treatment.
In addition, below are some tips to help prevent new scars from forming:
- Treat severe acne without delay to minimize scarring.
- Never pick at your skin, as this can delay skin healing and worsen scarring.
- Avoid irritating your skin, because irritation worsens acne and can lead to more scarring.

The Science
Scarring after acne is, unfortunately, very common. The face, back, and chest are some of the most typical locations of acne scars.1 While scars on the body can often be covered by clothing and are therefore less visible than facial scars, they can still impact a person’s self-image and confidence.
To understand how best to approach treating acne scars on the body, let’s take a quick look at how they differ from scars on the face.
How Acne Scars on the Body Differ from Those on the Face
Researchers have noticed a few patterns when comparing acne scars on the body to those on the face:
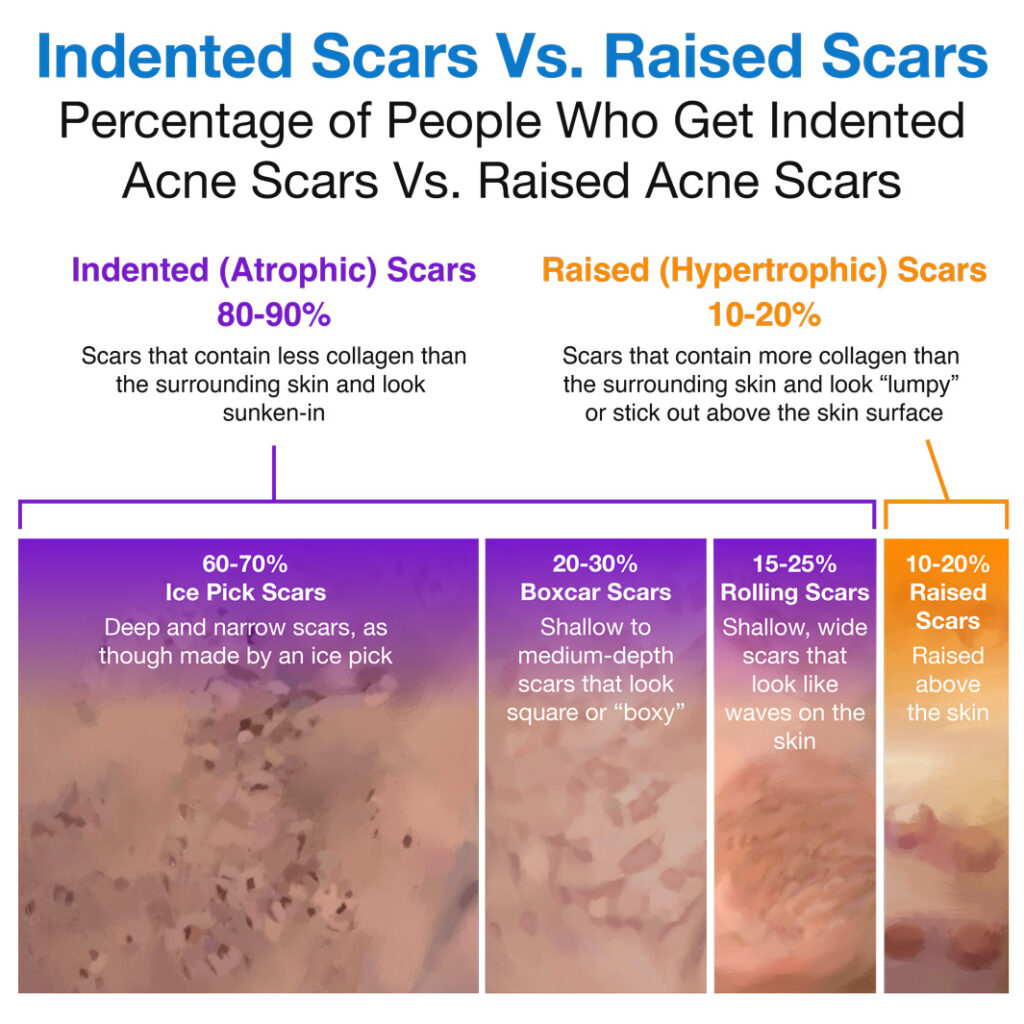
- The body tends to have fewer acne scars than the face: Acne scars develop from acne lesions, and acne lesions can occur wherever there are skin pores. Since the skin of the body contains fewer pores than the skin of the face, it makes sense that there tend to be fewer lesions and also fewer acne scars left behind on the body compared to the face. For example, one study that looked at 100 patients with acne scars found that 92% of all acne scars were on the face, with only 5% on the back and 3% on the chest.2
- The most severe types of acne scars are more likely to be located on the body than on the face: Even though the body tends to have fewer acne scars, they tend to be more severe. That’s because severe lesions often leave behind severe scars, , and the most severe types of lesions, occur most often on the body. Specifically, severe acne lesions called nodules and cysts tend to form on the back, chest, and back of the neck. These lesions tend to linger for a long time, often leaving behind significant scarring. In addition, two rare types of very severe, scarring acne called acne conglobata and acne fulminans most often affect the chest, back, and neck. Therefore, these locations on the body are the most likely to end up with severe acne scars.3
- Ice pick scars rarely develop on the body: The study mentioned above, which looked at 100 patients with acne scars, found that people rarely develop ice pick scars (a type of deep and narrow scar that looks like it was made by an ice pick) on the body. While 94% of patients had ice pick scars, almost all of these were on the face. Only 2% of patients had ice pick scars on the chest, and none had them on the back.2
Some of these differences between scars on the body and on the face are due to differences in skin structure between these areas. Expand the section below if you are curious to learn more.
Differences in Skin Structure Between the Body and Face
The skin on the body tends to be thicker than the skin on the face. Specifically, it is the outer layer of the skin, called the epidermis, that is thicker on the body compared to the face.
The epidermis includes the topmost layer of the skin, known as the stratum corneum. The stratum corneum is the layer of skin that you can see and touch, and it is the one that forms a barrier between your body and everything outside. For this reason, the stratum corneum is also called the skin barrier.
The skin barrier serves the important function of keeping moisture in the skin, preventing dehydration. Research suggests that proper hydration of the skin is critical for healing after any type of skin damage or injury, including after acne. In other words, if anything damages the skin barrier, we can expect loss of moisture from the skin, leading to delayed healing and possibly more scarring.4,5
Since the skin barrier on the body is thicker than on the face, this suggests that it is less prone to damage, making the skin on the body better protected from drying out and from delayed healing leading to scarring. This may partly explain why there tend to be fewer acne scars on the body than on the face.
Skin on body compared to skin on face:
Thicker skin barrier -> Less moisture loss from skin -> Faster healing -> Lower chance of scars
Medical research has shown that the worst scars, whether it be from acne or other causes, tend to develop in the shoulder, back, and chest areas, while the mildest scarring tends to occur in the mouth.6 Future studies will likely uncover further explanations why some regions of the body are more prone to scarring than others.
Treating Acne Scarring on the Body

When it comes to scar treatment, the skin on the body has two advantages over the skin on the face:
- It can handle more aggressive treatments: Because the skin on the body is thicker than the skin on the face, it can potentially handle harsher, more aggressive treatments that may have a higher chance of producing dramatic results.
- It is better protected from the sun: Unlike the skin on the face, the skin on the body is usually covered by clothing, protecting it from the sun’s harmful rays. This reduces the chances of treatment side effects like skin darkening (hyperpigmentation), which tend to get worse and more pronounced with sun exposure.7
However, despite these differences, the medical community currently gives identical treatment recommendations for acne scars regardless of their location. Below are some tips for treating acne scars on the body:7-11
- Get clear before starting scar treatment: Experts recommend delaying scar treatment until your skin is clear of any active acne. Otherwise, you may find yourself in a cycle of treating old acne scars while new ones continuously form.
- Protect your skin from the sun: Excessive sun exposure can slow down skin healing, possibly leading to worse scarring. In addition, the sun’s UV rays can darken existing scars and make them more visible. Protect your skin from the excessive sunlight by wearing long-sleeved clothing and/or applying a broad-spectrum sunscreen.
- Research treatment options here at Acne.org: There are numerous treatment options for acne scars, including laser therapy, chemical peels, microneedling, and many others. Some treatments are best suited to specific types of scars, and the treatments vary widely in the number of appointments needed, cost, success rate, and side effects. Since most people have a mixture of scar types on their skin, a combination of several different scar treatments may produce the best results.
For example, one 2020 study published in the Journal of Clinical and Aesthetic Dermatology tested a combination approach on 139 patients with acne scarring and reported high patient satisfaction. In that study, the patients received chemical peels, subcision (a treatment in which a doctor probes the skin underneath rolling scars with a needle), and microneedling, but many other combinations are possible.10 - Talk to your doctor if you are taking isotretinoin or have recently stopped taking it: The medical community has long been concerned that isotretinoin might interfere with skin healing. Therefore, the standard recommendation is to wait 6 months after stopping isotretinoin therapy before starting most scar repair procedures. However, experts have recently begun to question this recommendation. Since it is currently unclear how much isotretinoin might impact healing, stay on the safe side and consult your doctor on how long to wait before proceeding with scar treatment, especially if you are considering some of the more invasive scar treatments like lasers, dermabrasion, chemical peels, or microneedling.
- Design a personalized treatment plan together with your doctor: Experts recommend that doctors should tailor a scar treatment plan to each patient. For example, a 2015 article in the Journal of Clinical and Aesthetic Dermatology states, “Dermatologists should individualize the best treatment options for each patient.”8 Your treatment plan should take into account the size, type, severity, and location of your scars as well as other factors like your medical history. After doing your research here, come to your medical appointment armed with questions for your doctor.
When it comes to acne scars, prevention is worth a pound of cure. To give yourself the best chance of developing as few new acne scars as possible, follow these guidelines:
- Treat severe acne early to minimize scarring: If you have severe acne, begin treating it as soon as possible. The longer you delay acne therapy, the more time there is for inflammation to run wild in your skin, increasing the chances of scarring.
- Never pick at your skin: Picking at your skin triggers inflammation and worsens scarring, so make an effort to quit this habit immediately.
- Avoid irritating your skin: Skin irritation caused by clothing or sports equipment rubbing against your skin can make acne worse and can even sometimes trigger acne in areas where you never had breakouts. Limit repeated skin irritation as much as possible, as it can lead to more scarring.
References
- Kravvas, G. & Al-Niaimi, F. A systematic review of treatments for acne scarring. Part 1: Non-energy-based techniques. Scars Burn Heal. 3, 2059513117695312 (2017). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5965325/
- Agrawal, D. A. & Khunger, N. A. Morphological study of acne scarring and its relationship between severityand treatment of active acne. J Cutan Aesthet Surg. 13, 210-216 (2020). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7646434/
- Hafsi, W. & Badri, T. Acne Conglobata. [Updated 2020 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459219/
- Tagami, H. Location-related differences in structure and function of the stratum corneum with special emphasis on those of the facial skin. Int J Cosmet Sci. 30, 413-34 (2008). https://pubmed.ncbi.nlm.nih.gov/19099543/
- Mustoe, T. A. & Gurjala, A. The role of the epidermis and the mechanism of action of occlusive dressings in scarring. Wound Repair Regen. 19 Suppl 1, s16-s21 (2011). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3725331/
- Bayat, A., McGrouther, D. A. & Ferguson, M. W. Skin scarring. BMJ. 326, 88-92 (2003). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1125033/
- Al-Shaqsi, S. & Al-Bulushi, T. Cutaneous scar prevention and management: Overview of current therapies. Sultan Qaboos Univ Med J. 16, e3-e8 (2016). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4746040/
- Werschler, W. P., Herdener, R. S., Ross, V. E. & Zimmerman, E. Critical considerations on optimizing topical corticosteroid therapy. J Clin Aesthet Dermatol. 8 (8 Suppl), S2-S8 (2015). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4570086/
- Abdel Hay, R., Shalaby, K., Zaher, H., Hafez, V., Chi, C. C., Dimitri, S., Nabhan, A. F. & Layton, A. M. Interventions for acne scars. Cochrane Database Syst Rev. 4, CD011946 (2016). The Cochrane database of systematic reviews. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7069546/
- Rullan, P. P., Olson, R. & Lee, K. C. A Combination approach to treating acne scars in all skin types: Carbolic chemical reconstruction of skin scars, blunt bi-level cannula subcision, and microneedling – A case series. J Clin Aesthet Dermatol. 13, 19-23 (2020). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7380695/
- Acne mechanica. Br Med J. 1, 130 (1976). https://pubmed.ncbi.nlm.nih.gov/129186/
 Acne.org Products
Acne.org Products