A Safe Rule of Thumb Is to Change Your Pillowcase Once per Week

The Essential Info
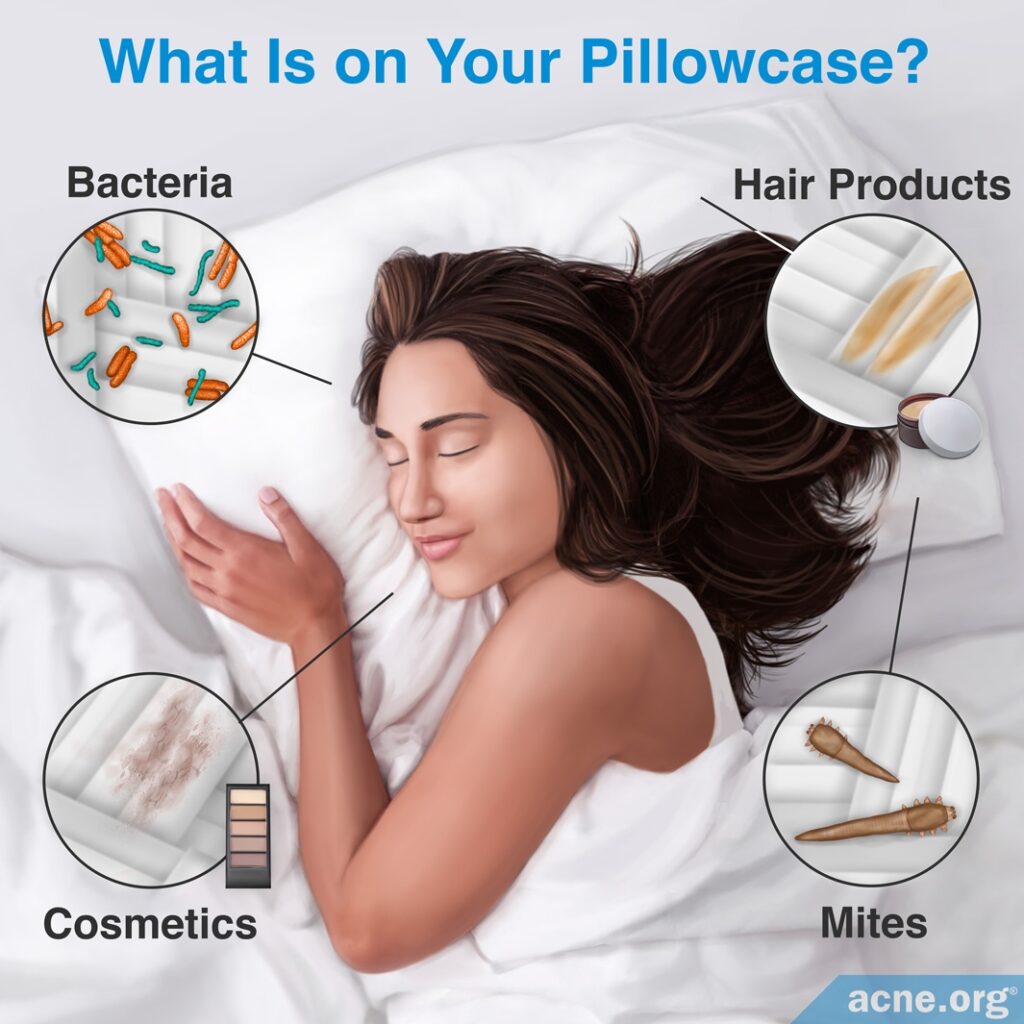
Pillowcases can pick up:
- Bacteria and cosmetics from your skin
- Haircare products from your hair
However, these things left on pillowcases are unlikely to contribute to acne, with the exception of the haircare products pomade or brilliantine. If you use pomade or brilliantine, wash your hair before going to sleep at night.
Even though your pillowcase is unlikely to contribute to acne, to be safe, a good rule of thumb is to change your pillowcase once a week.
When washing your pillowcase, use the “hot” setting on your washing machine. Wash the entire pillow itself every three months, also on the “hot” setting.

The Science
- Can Bacteria on Your Pillowcase Worsen Acne?
- Can Hair Products or Cosmetics on Your Pillowcase Worsen Acne?
- Can Mites on Your Pillowcase Worsen Acne?
- The Bottom Line
If you are acne-prone, you may wonder whether sleeping on the same pillowcase night after night might make your acne worse.
It is true that pillowcases can become contaminated with bacteria from your skin or collect residue from the cosmetics and haircare products you use. Fortunately, it is unlikely that any of these things could cause acne or make acne worse.
Even though dirty pillowcases probably will not contribute to acne, to be on the safe side, wash pillowcases with water and detergent once a week.
Additionally, it is a good idea to wash the pillow itself occasionally, although there are no research-based guidelines for how often this needs to be done. To be on the safe side, wash your pillow once every three months. When you buy a pillow, check that the material is suitable for laundering, and follow the manufacturer’s instructions for washing it.
In general, pillows and pillowcases can be washed with laundry detergent using the “hot” setting. This is sufficient to kill dust mites and most bacteria.1
Can Bacteria on Your Pillowcase Worsen Acne?
Every day, your skin sheds some dead cells, which can collect on your pillowcase, along with any bacteria that may have been living on your skin.1 When you continue to sleep on the same pillowcase, some of these bacteria may be transferred back onto your face, but this is unlikely to contribute to acne.
While certain bacteria do play a role in making acne worse, they do so only when they are inside skin pores. Bacteria on the skin’s surface do not cause acne. In fact, you already have various bacteria on your skin, which do not contribute to acne.
Caution: Pillowcases Can Transfer Other Infections
On the other hand, if you share your pillow with a partner when he or she is sick with a cold, flu, or other infection, your pillowcase may pick up his or her microbes (bacteria or viruses) and transfer them onto you. In that case, you may end up with your partner’s cold or other infection.
Therefore, it is a good idea not to share pillows while your partner is sick, and to wash your pillowcase in hot water with detergent if you believe it may have picked up microbes from your partner’s infection.
Can Hair Products or Cosmetics on Your Pillowcase Worsen Acne?
Pillowcases potentially pick up haircare products from your hair and/or leftover cosmetics from your skin. Let’s look at haircare products and cosmetics in a bit more detail.
Haircare Products Left on Pillowcases – A Potential Concern in Some Cases
Some haircare products, particularly pomade, can cause a condition called pomade acne.2 Pomade is a hair styling product which is used primarily by Black people to shape their hair into a smooth and shiny hairdo. Pomade acne typically appears along the hairline, but if your pillowcase picks up some pomade from your hair, it might spread to the rest of your face and result in additional breakouts.
To prevent pomade acne, the best approach is to avoid using pomade. If you do use it, though, be sure to wash your hair thoroughly before you go to sleep at night. Additionally, if you suspect that your pillowcase may have picked up some pomade, wash the pillowcase in hot water with detergent.
As a side note, if you experience breakouts along your hairline, check your haircare products in case they may be comedogenic, meaning tending to clog skin pores.
Cosmetics Left on Pillowcases – Not a Big Concern
Remnants of cosmetics on pillowcases are highly unlikely to bring about acne. While some cosmetic products can clog pores, most sold today are relatively safe and non-comedogenic (will not clog pores). Additionally, the amount of cosmetic product that might end up on your pillowcase is most likely insignificant, so the chances that this will present a problem are negligible.
Can Mites on Your Pillowcase Worsen Acne?
Mites are small arachnids (from the family of spiders) that are barely visible to the naked eye and feed on skin cells and skin oil of humans. They live on human skin and can be found in the pores and in or on skin oil glands.
Another one of their favorite places to live is bed linens, such as pillowcases, which provide plenty of skin flakes for the mites to feed on. While mites most likely do not contribute to acne and are usually harmless to humans, they can cause health problems like allergies, worsening of asthma, or skin rashes if the number of mites living on your skin becomes excessive.3 Consequently, it is a good idea to keep mites in check by changing your pillowcase weekly and washing it as described above to kill off the mites.
There are two species of mites commonly found on humans:
- Demodex folliculorum, which usually lives in pores on the face
- Demodex brevis, which usually lives in skin oil glands on the neck and chest3
For most people, these mites are harmless. However, in asthmatic patients and people allergic to mites, a Demodex mite infestation can trigger symptoms such as sneezing, coughing, or wheezing. Further, when the number of mites living on a person’s skin becomes too large, a condition called demodicosis may result.
Demodicosis: A Rare Skin Condition Caused by Mites
Demodicosis produces breakouts that look similar to acne, and so some people wonder if the microscopic skin mites that cause demodicosis might also play a part in acne.
Evidence is still trickling in on whether these mites affect acne, with some research showing no correlation4 and other research showing that there perhaps might be a correlation between overgrowth of Demodex mites and acne.5-7

For example, according to a study published in 2006 in the Journal of the European Academy of Dermatology and Venereology, people with acne carry a similar number of Demodex mites living on their skin as people without acne.4
However, regardless of whether these mites are correlated with acne symptoms, it is unlikely that mites on your pillowcase will directly lead to more acne.
Nonetheless, if you suffer from acne-like breakouts and regular acne treatments do not improve your symptoms, it is possible that you are actually suffering from demodicosis. Talk to your doctor about this possibility. If demodicosis is responsible for your breakouts, your doctor may recommend acaricidal therapy (treatments that kill mites and ticks).5
Reducing Your Exposure to Mites
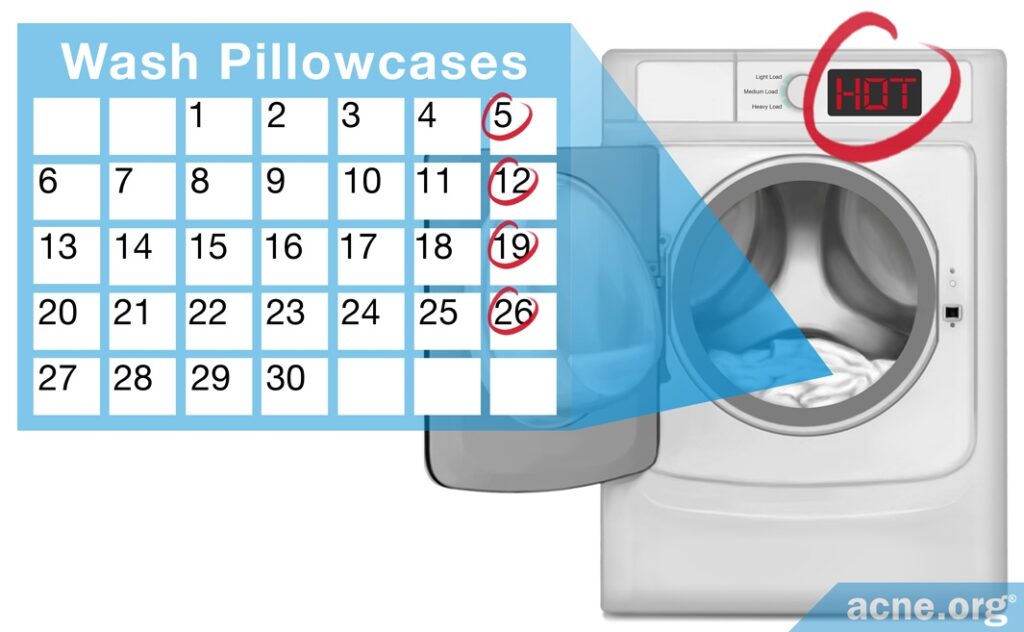
If you suffer from asthma, are allergic to mites, or have demodicosis, it is important to reduce your risk of exposure to mites. Research shows that Demodex mites die at 58°C (136°F).8 So, change your pillowcase weekly and wash it using your washing machine’s “hot” setting in order to kill mites that may be living on it. As an added bonus, this will also kill bacteria that can cause infections unrelated to acne.9
Additionally, if you are sensitive to mites, select pillowcases made of materials that block the passage of them. This will ensure that if any mites are living on your pillow itself they will not be able to pass through the pillowcase onto your face.
According to a study published in the Journal of Allergy and Clinical Immunology in 1999, the best materials to prevent the penetration of mites are tightly woven fabrics and non woven synthetic fabrics.10
In practical terms, this means that pillowcases with a higher thread count or those labeled as “hypoallergenic” are the best choice if you are sensitive to mites. However, most people with acne do not need to worry about this.
The Bottom Line
While bacteria, leftover hair products and cosmetics, or mites living on your pillowcase are unlikely to contribute to acne, it is not a bad idea to limit your exposure to these pillowcase contaminants.
I recommend changing and washing your pillowcase in hot water with detergent once a week. Feel free to add bleach.
Additionally, to err on the side of caution, wash your pillow approximately once every three months by following the manufacturer’s instructions.
These precautions probably will not improve your acne, but they may help to reduce other health risks, such as allergies, asthma, and bacterial infections.
References
- Creamer, E. & Humphreys, H. The contribution of beds to healthcare-associated infection: the importance of adequate decontamination. J. Hosp. Infect. 69, 8 – 23 (2008). https://www.ncbi.nlm.nih.gov/pubmed/18355943
- Bhate, K. & Williams, H. C. Epidemiology of acne vulgaris. Br. J. Dermatol. 168, 474 – 485 (2013). https://www.ncbi.nlm.nih.gov/pubmed/23210645
- Rather, P. A. & Hassan, I. Human demodex mite: the versatile mite of dermatological importance. Indian. J. Dermatol. 59, 60 – 66 (2014). https://www.ncbi.nlm.nih.gov/pubmed/24470662
- Okyay, P., Ertabaklar, H., Savk, E. & Ertug, S. Prevalence of Demodex folliculorum in young adults: relation with sociodemographic/hygienic factors and acne vulgaris. J. Eur. Acad. Dermatol. Venereol. 20, 474 – 476 (2006). https://www.ncbi.nlm.nih.gov/pubmed/16643160
- Zhao, Y. E., Hu, L., Wu, L. P. & Ma, J. X. A meta-analysis of association between acne vulgaris and Demodex infestation. J. Zhejiang. Univ. 13, 192 – 202 (2012). https://www.ncbi.nlm.nih.gov/pubmed/22374611
- Erdal, B. & Albayrak, H. Investigation of the prevalence of Demodex spp. in dermatological diseases. Turkiye Parazitol. Derg. 46, 54-59 (2022). https://pubmed.ncbi.nlm.nih.gov/35232707/
- Maldonado-Gómez, W., Guevara-Sánchez, E., Guevara-Vásquez, G., Mera-Villasis, K. & Munayco, C. V. Association between Demodex infestation and severe acne vulgaris: A cross-sectional study of 168 patients. Actas Dermosifiliogr. 113, 758-764 (2022). https://pubmed.ncbi.nlm.nih.gov/35504311/
- Zhao, Y. E., Guo, N. & Wu, L. P. The effect of temperature on the viability of Demodex folliculorum and Demodex brevis. Parasitol. Res. 105, 1623-1628 (2009). https://www.ncbi.nlm.nih.gov/pubmed/19774398
- Fijan, S. & Turk, S. Š. Hospital textiles, are they a possible vehicle for healthcare-associated infections? Int. J. Environ. Res. Public Health. 9, 3330-3343 (2012). https://www.ncbi.nlm.nih.gov/pubmed/23202690
- Vaughan, J. W., McLaughlin, T. E., Perzanowski, M. S. & Platts-Mills, T. A. Evaluation of materials used for bedding encasement: effect of pore size in blocking cat and dust mite allergen. J. Allergy. Clin. Immunol. 103, 227 – 231 (1999). https://www.ncbi.nlm.nih.gov/pubmed/9949312
 Acne.org Products
Acne.org Products