Baby Acne Is Mild Acne That Develops in Some Newborn Babies Because of Hormone Fluctuations after Birth

The Essential Info
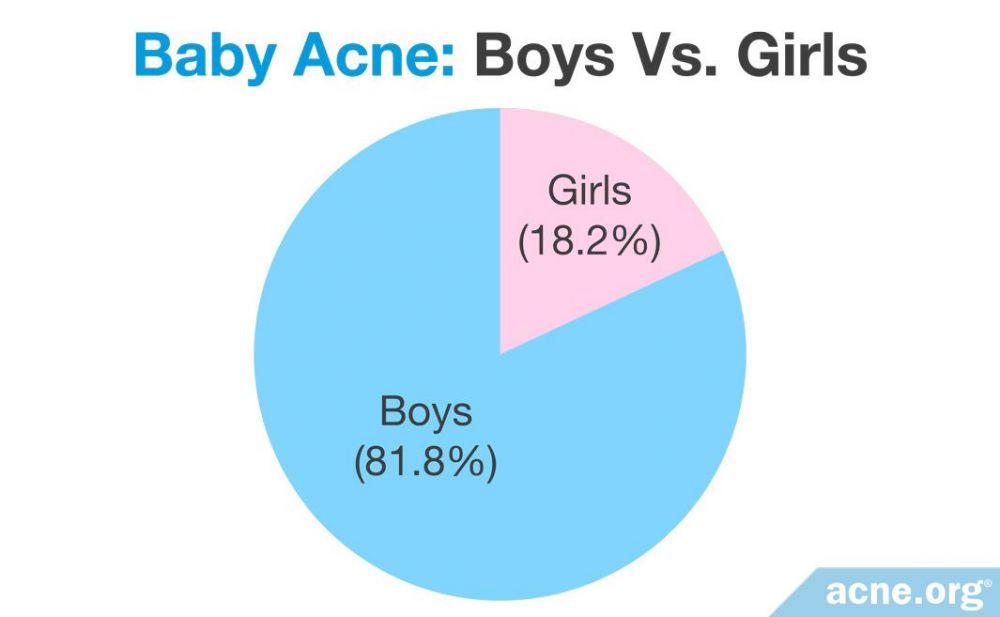
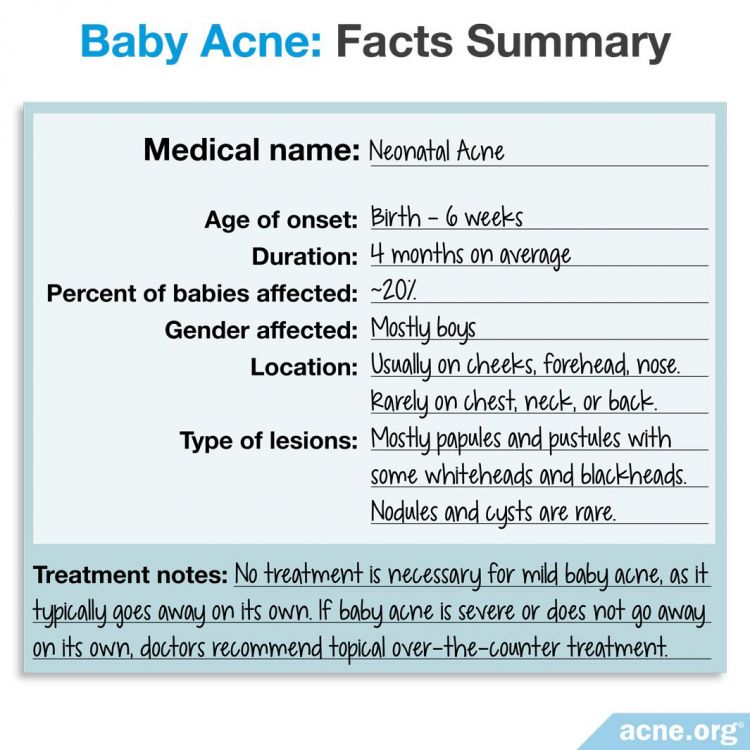
About 1 in 5 babies, mostly baby boys, are born with acne or develop it in the first six weeks of their lives. This baby acne is usually mild and appears on the face.
Baby acne occurs due to fluctuating hormones after birth, and resolves after a few months when hormone levels normalize.
No treatment is necessary unless baby acne is severe or fails to go away on its own. In such cases, doctors recommend topical treatments.
Baby Acne Can Help Predict Adolescent Acne: People who experience baby acne are more likely to develop adolescent acne and tend to suffer with more severe symptoms. If your baby is amongst one of the 1 in 5 babies with baby acne, get educated about acne and available treatments, so when your child reaches adolescence you can help keep them clear.

The Science
- A Baby’s Raging Hormones
- Factors That Contribute to Baby Acne
- What Does Baby Acne Look Like?
- Where on the Face Does Baby Acne Occur Most?
- How Do You Treat Baby Acne?
- Baby Acne Vs. Other Types of Acne
Baby acne, also known as neonatal acne, is acne that a baby is born with or that develops in the first six weeks of a baby’s life.
Baby acne occurs in about one fifth of babies, usually in baby boys.
It normally appears on the face, is typically mild, and goes away on its own after 1 to 6 months.1-5
In most cases, baby acne occurs for the same reason teen acne does: hormone fluctuations. We rarely think of babies as having “raging hormones,” but, in a way, they do.
A Baby’s Raging Hormones
Before birth
Before a baby boy or girl is even born, while still in its mother’s womb, it receives androgens (male hormones that are present in both males and females) from its mother.2 Just like in teens and adults, these androgens stimulate a baby’s skin to produce more skin oil, setting up the child for potential acne after it is born.
After birth
Once the baby is born, boys’ and girls’ own adrenal glands (small organs located on top of the kidneys) take over the job of producing androgens. In baby boys, the testicles also produce androgens. This means baby boys produce more androgens than baby girls. This new rush of androgens, particularly in baby boys, can sometimes result in the skin producing too much skin oil and breaking out with acne.2,6,7
After 6 months of age
Things start to calm down after 6 months or so. From birth to 6 months old, adrenal glands are particularly large and are making more androgens than they will later in infancy. When a baby is between 6 months and 1 year old, its adrenal glands gradually shrink. As a result, the glands stop producing such large amounts of androgens. As hormone levels normalize, the skin stops producing so much skin oil, and baby acne naturally clears up.2,4,7
Factors That Contribute to Baby Acne
Aside from hormones, several additional factors can contribute to baby acne:
- Family history: A family history of acne or of elevated male hormone levels makes a child more likely to develop baby acne.
- Certain skin bacteria: Having a type of fungi called Malassezia in the skin pores might trigger inflammation (redness, swelling, and soreness) in the baby’s skin, causing baby acne. However, this theory is controversial since not all babies with baby acne have this type of fungi.2,7 Still, if a baby develops a large number of acne lesions, a doctor may prescribe an antifungal cream, such as 2% ketonazole cream, to see whether this helps to manage the acne.5,8
What Does Baby Acne Look Like?
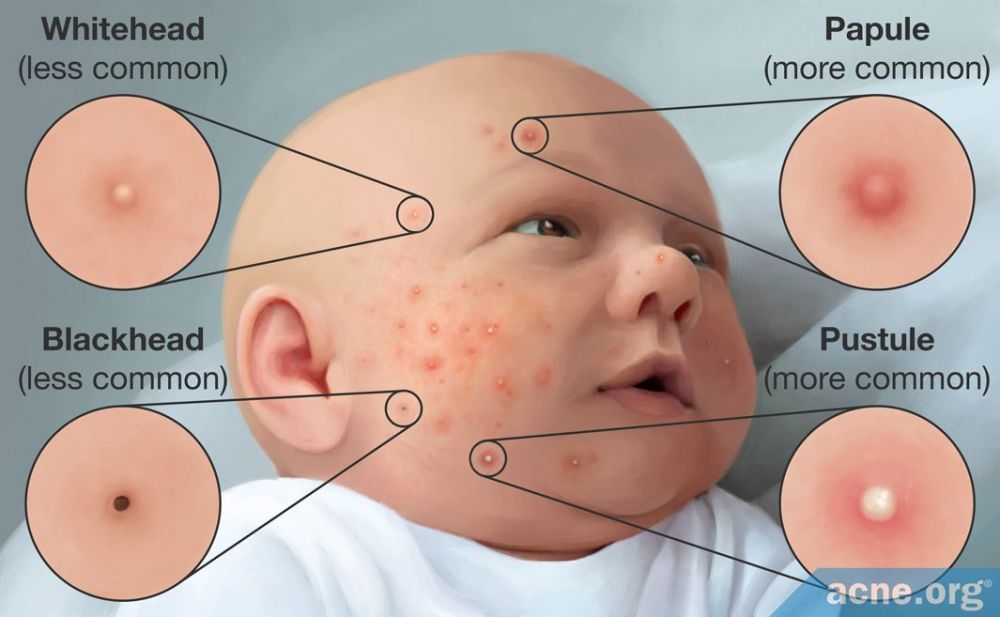
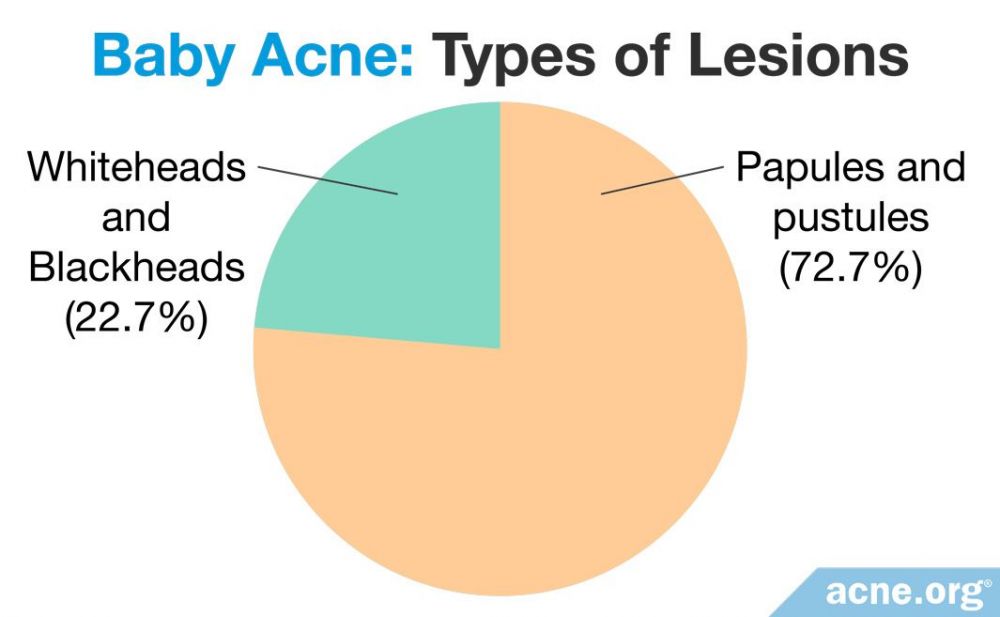
Baby acne looks similar to mild teen acne. According to a study published in the International Journal of Dermatology, the majority of the babies’ acne lesions were papules and pustules–inflamed and red lesions that most people refer to as “pimples” or “zits.” However, they had some whiteheads and blackheads–clogged pores that appear as small, non-inflamed white or black dots on the skin–as well.1,6
Where on the Face Does Baby Acne Occur Most?
Most of the babies’ acne lesions–81.8%–were on the cheeks, with occasional lesions on the back and chest.1 However, another article in the medical journal Dermatologic Clinics notes that baby acne can also appear on the forehead and nose.4 The researchers noted that, on average, the babies developed acne at 3 weeks of age, and the condition lasted 4 months.1
How Do You Treat Baby Acne?
![In most cases [of baby acne], no treatment is needed](https://www.acne.org/wp-content/uploads/2022/01/1389807925_05Inmostcasesofbabyacnenotreatmentisneeded.jpg)
Normally, baby acne requires no treatment. Between 6 months and 1 year of age, androgen levels drop off naturally, and baby acne usually clears up on its own.4

According to a 2014 article in the medical journal Cutis (meaning “skin”), “Guardians should be reassured that [baby] acne is mild, self-limited, and generally [goes away on its own] without scarring in approximately 1 to 3 months. In most cases, no treatment is needed.”2
In rare cases, baby acne may fail to heal on its own. Severe baby acne can also be concerning because it may leave scars. In such cases, doctors recommend topical treatments which are available over-the-counter. The suggested treatment depends on the type of acne lesions the baby has.
- If the baby has mostly papules and/or pustules: Doctors often recommend 2% topical erythromycin + 2.5% benzoyl peroxide
- If the baby has mostly whiteheads and blackheads: Doctors often recommend 20% azelaic acid cream + 0.025 – 0.05% tretinoin cream2,7
The baby’s doctor may have to tweak these recommendations depending on how severe the baby’s acne is.
Topical treatments like these should effectively clear baby acne. If they do not, the baby’s parents should consult a doctor to make sure the acne is not a sign of an underlying condition like a hormonal problem or infection by bacteria or a virus.2,4

Similarly, if a baby’s acne persists past the age of 1, it is important to see a doctor to rule out other potential medical issues.2,4
Baby Acne Vs. Other Types of Acne
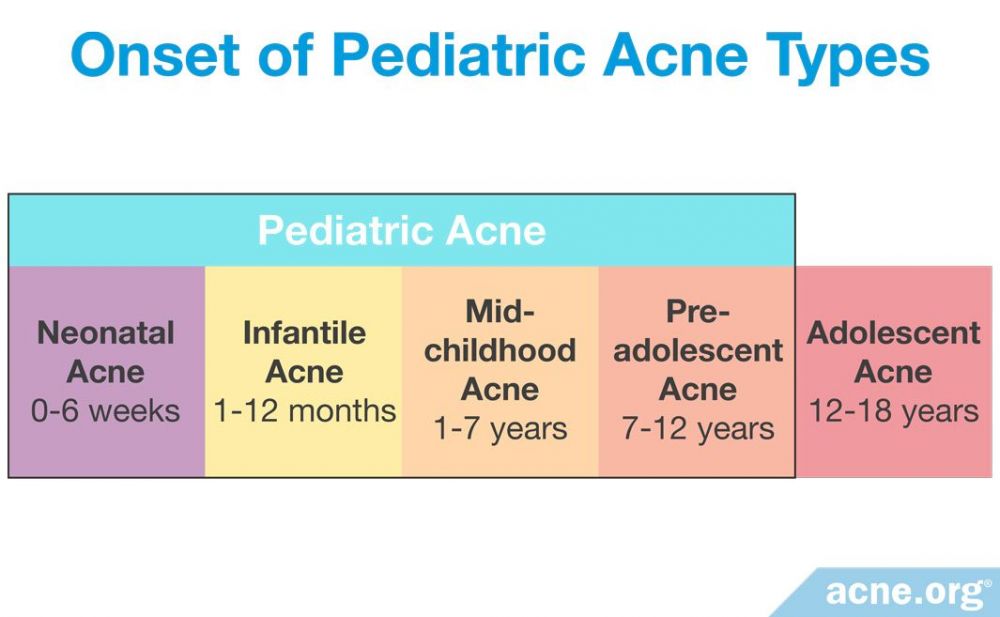
Baby acne falls under the larger umbrella of so-called pediatric (children’s) acne. Pediatric acne is any acne that develops when a child is younger than 12 years old. Baby, or neonatal, acne is the earliest type of pediatric acne that typically begins at birth or up to 6 weeks of age.3
A baby who develops baby acne is more likely to suffer from adolescent (teen) acne when he gets older. People who experienced baby acne are also more likely to develop more severe adolescent acne than people who never had baby acne.1-3
References
- Katsambas, A. D., Katoulis, A. C. & Stavropoulos, P. Acne neonatorum: A study of 22 cases. Int J Dermatol 38, 128 – 130 (1999). https://europepmc.org/abstract/med/10192162
- Serna-Tamayo, C., Janniger, C. K., Micali, G. & Schwartz, R. A. Neonatal and infantile acne vulgaris: An update. Cutis 94, 13 – 16 (2014). https://www.mdedge.com/dermatology/article/84377/pediatrics/neonatal-and-infantile-acne-vulgaris-update
- Samycia, M. & Lam, J. M. Infantile acne. CMAJ 188, E540 (2016). https://www.ncbi.nlm.nih.gov/pubmed/27873756
- Maroñas-Jiménez, L. & Krakowski, A. C. Pediatric Acne: Clinical Patterns and Pearls. Dermatol Clin 34, 195 – 202 (2016). https://www.ncbi.nlm.nih.gov/pubmed/27015779
- Admani, S. & Barrio, V.R. Evaluation and treatment of acne from infancy to preadolescence. Dermatologic Therapy 26: 462-466 (2013). https://pubmed.ncbi.nlm.nih.gov/24552409/
- Que, S.K.T. et al. Acne: Kids are not just little people. Clinics in Dermatology 34: 710-716 (2016). https://pubmed.ncbi.nlm.nih.gov/27968930/
- Herane, M. I. & Ando, I. Acne in infancy and acne genetics. Dermatology 206, 24 – 28 (2003). https://www.ncbi.nlm.nih.gov/pubmed/12566802
- Eichenfield, L.F., Krakowski, A.C., Piggott, C., Del Rosso, J., Baldwin, H., Friedlander, S.F., Levy, M., Lucky, A., Mancini, A.J., Orlow, S.J., Yan, A.C., Vaux, K.K., Webster, G., Zaenglein, A.L. & Thiboutot, D.M. American Acne and Rosacea Society. Evidence-based recommendations for the diagnosis and treatment of pediatric acne. Pediatrics. 131 Suppl 3, S163-86 (2013). https://www.ncbi.nlm.nih.gov/pubmed/23637225
 Acne.org Products
Acne.org Products