Urea Is Included in Many Topical Skincare Products. It Moisturizes and Can Strengthen the Outermost Layer of Skin.

The Essential Info
What Is Urea?: Urea is often included as an ingredient in various skincare products, particularly moisturizers. This is because urea can help hydrate the skin. In fact, urea exists naturally in the outermost layer of our skin, where it helps maintain hydration.
Urea and Acne: The natural urea in our skin helps keep the top layer of the skin, called the skin barrier, strong. A healthy and strong skin barrier helps keep moisture from escaping through the skin, which keeps the skin in balance. This is particularly important for people with acne because, while still unproven, acne-prone skin may come with an impaired skin barrier more often than not. However, depending on the formula, skincare products containing synthetic urea may either strengthen or weaken the skin barrier, so it is important that the product is tested to see how it impacts the skin barrier. In other words, just because a product contains urea doesn’t mean it will be good for acne.
Urea for Other Skin Conditions: Urea can also be included at a high dose (up to 40%) in creams, lotions, shampoos, and gels, to treat skin disorders like atopic dermatitis or psoriasis. Since different conditions respond well only to specific concentrations of urea, talk to your doctor about which formulation is best for you. If you plan on using a product that contains large amounts of urea, be aware that in higher concentrations it can result in unfavorable reactions, such as stinging of the skin. However, if you simply see it as an ingredient in your moisturizer, it should be fine.

The Science
- What Is Urea?
- What Does Urea Do in the Skin?
- Varying Concentrations of Urea for Different Skin Conditions
- Side Effects
What Is Urea?
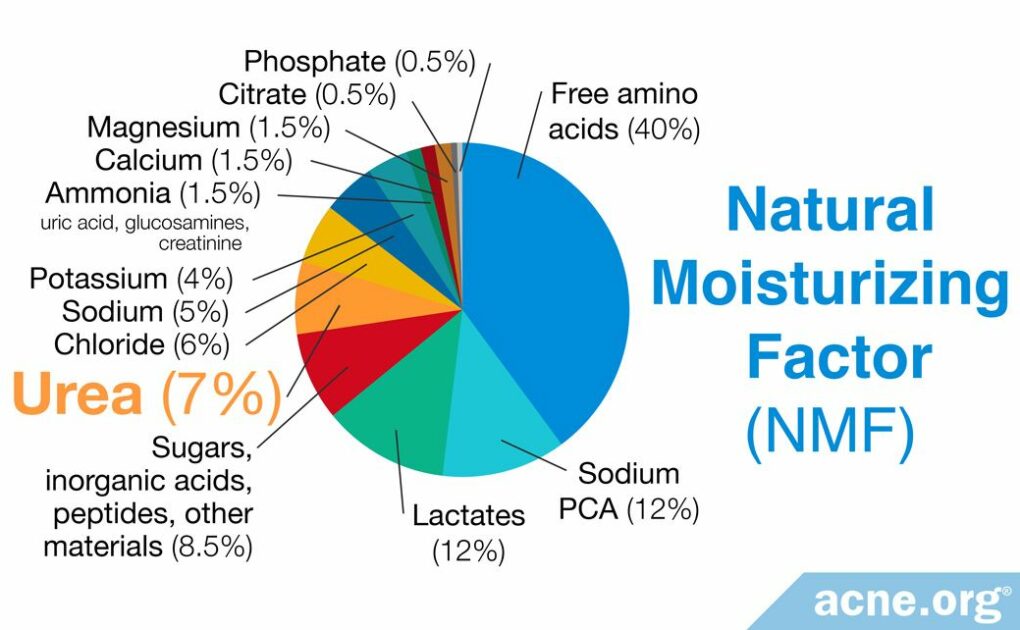
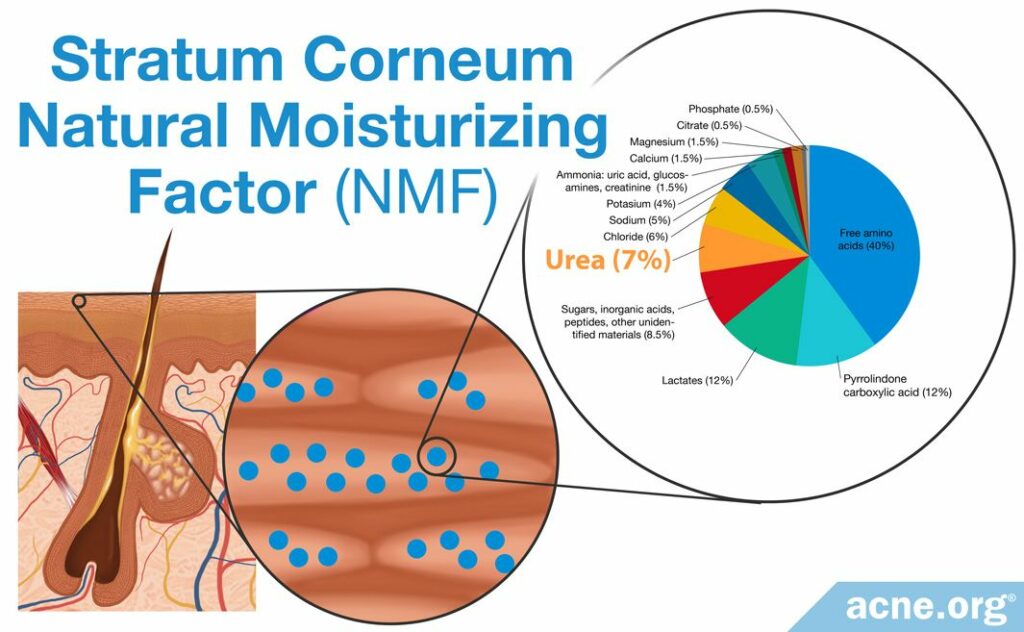
Urea is a naturally occurring waste product in urine and is also present elsewhere in the body, including in the skin, where it makes up about 7% of what dermatologists call the Natural Moisturizing Factor (NMF).1,2
What Does Urea Do in the Skin?
Urea is an important component of natural moisturizing factor (NMF). The primary purpose of the NMF is to maintain adequate hydration in the skin, particularly in the outermost layer of skin, the stratum corneum.
As a 2012 article in Practical Dermatology explains:

The role of the NMF is to maintain adequate skin hydration. Adequate hydration of the stratum corneum serves three major functions: (1) it maintains plasticity of the skin, protecting it from damage; (2) it allows […] enzymes to function in the process of [skin shedding]; and (3) it contributes to optimum [skin] barrier function.”3
As a component of the NMF, urea acts as a moisturizer and helps to improve the quality of the skin’s protective barrier, called the barrier function of the skin.4 This protects the body from external substances.
According to a 2011 article in the Journal of Clinical Medicine:

“Healthy skin provides protection of the body from environmental factors: physical (mechanical trauma, thermal injury, radiation), chemical (destructive agents, surface active substances, xenobiotics, allergens) and biological (bacteria, viruses, etc.). A major element of the defensive function of the skin is to maintain homeostasis by preventing the uncontrolled loss of water, ions and serum proteins from the organism into the environment.”5
Inadequate hydration of the stratum corneum results in dry skin. In fact, several skin conditions, including psoriasis and atopic dermatitis, both of which feature extremely dry skin among their primary symptoms, appear to be linked to reduced levels of NMF.3
In addition to acting as a moisturizer and helping to improve the skin’s barrier function, urea also exhibits several other important functions in the skin:
- It aids in the process of breaking down keratin, which is a protein that exists in various places in the body, including skin, nails, and hair. This is an important step in the process of shedding the outer layer of skin.2,6
- It is antimicrobial (antibacterial), interfering with the growth of bacteria and other microorganisms.2,6
- It helps to soothe itchy skin.2,6
While urea is a naturally occurring substance, it can also be created synthetically in laboratories (by placing ammonia and carbon dioxide into a reactor under high temperature and high pressure). Synthetic urea is used for multiple purposes, including medical uses.1,2,7
The most common medical application for urea is dermatology. Dermatologists have prescribed urea, mostly in cream and ointment preparations, since the 1940s. More recently, it has been added as an ingredient in many cosmetic products.5,8
Researchers have conducted numerous studies on urea as a dermatological therapy, specifically investigating:
- It as a treatment for various skin disorders such as ichthyosis (a disease featuring dry, scaly skin), atopic dermatitis, psoriasis, and severely dry skin.6,9
- Its effect on healthy skin.6,9,10
- Its role in enhancing the penetration of other topical compounds.10,11
At least two studies have identified urea as an effective moisturizer.
Expand to read details of studies

A 1990 study in the Indian Journal of Dermatology tested whether various doses of urea (10% and 20% urea formulations) applied to the skin daily for two weeks were effective moisturizers in people who were chosen, having at least one of a variety of skin disorders that the researchers investigated. The authors noted, “Results indicate that urea is an effective moisturizer.”12

A 2022 study in the journal Skin Research & Technology investigated the moisturizing ability of skin products containing 10% urea. In the first part of the study, volunteers applied the moisturizer, and the researchers measured skin hydration 30 minutes later, as well as 24 hours later. In the second part of the study, volunteers applied the product twice a day for 2 weeks. The authors concluded that in both parts of the study, the moisturizer containing 10% urea significantly improved skin hydration both in the short term and long term. Therefore, moisturizers containing urea may be an effective treatment option for patients with dry skin.12
However, just because urea is added to a moisturizer does not mean that moisturizer will be sure to improve the skin’s barrier function. Based on the research we have thus far, it depends greatly on the other ingredients in the moisturizer. Some urea-containing moisturizers strengthen the skin’s barrier function while others deteriorate it.
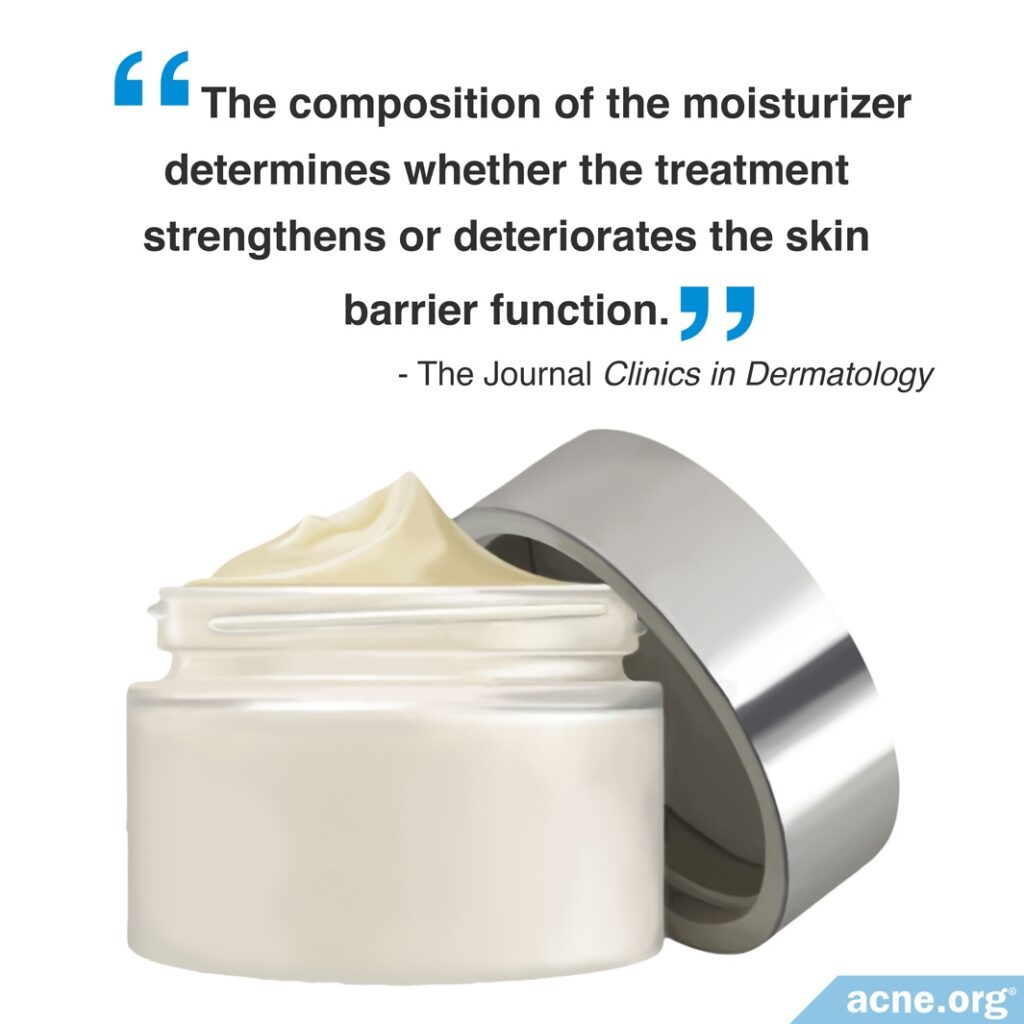
Furthermore, just because the dryness of the skin appears to improve, this does not always mean the skin’s barrier is strengthened. Research shows that while some moisturizers containing urea seem to improve barrier function, others have no effect or may even weaken the skin barrier.13-15
Expand to read details of research
According to a 2012 article in Clinics in Dermatology, “The composition of the moisturizer determines whether the treatment strengthens or deteriorates the skin barrier function, which may have consequences for the outcome of the dermatitis […] Differing outcomes have also been reported in healthy skin: some moisturizers produce deterioration in skin barrier function and others improve the skin.”
The same article reviewed several studies in which different formulations produced different results in skin, even when the concentration of urea in the moisturizer remained the same. For example, “One placebo-controlled study showed 5% urea was responsible for barrier improvement. Not all 5% urea formulations improve skin barrier function, however; for example, one study found inclusion of 5% urea in a simple canola oil cream did not improve skin barrier function.”13

Similarly, a 2007 study in the British Journal of Dermatology found different outcomes with two different formulations of moisturizers containing 5% urea. This study found that the two moisturizers containing urea had opposite effects, even though they had the same concentration of urea. One of these moisturizers increased skin water loss, and the other decreased water loss. In other words, one of the moisturizers weakened the skin barrier function, while the other strengthened it.14
On the other hand, a 2022 study published in the journal Clinical and Experimental Dermatology compared several simple moisturizers and found that the one containing urea was the most effective at improving the skin’s barrier function. It should be noted that the moisturizer with urea also contained glycerol, which likely contributed to the moisturizing effect.15
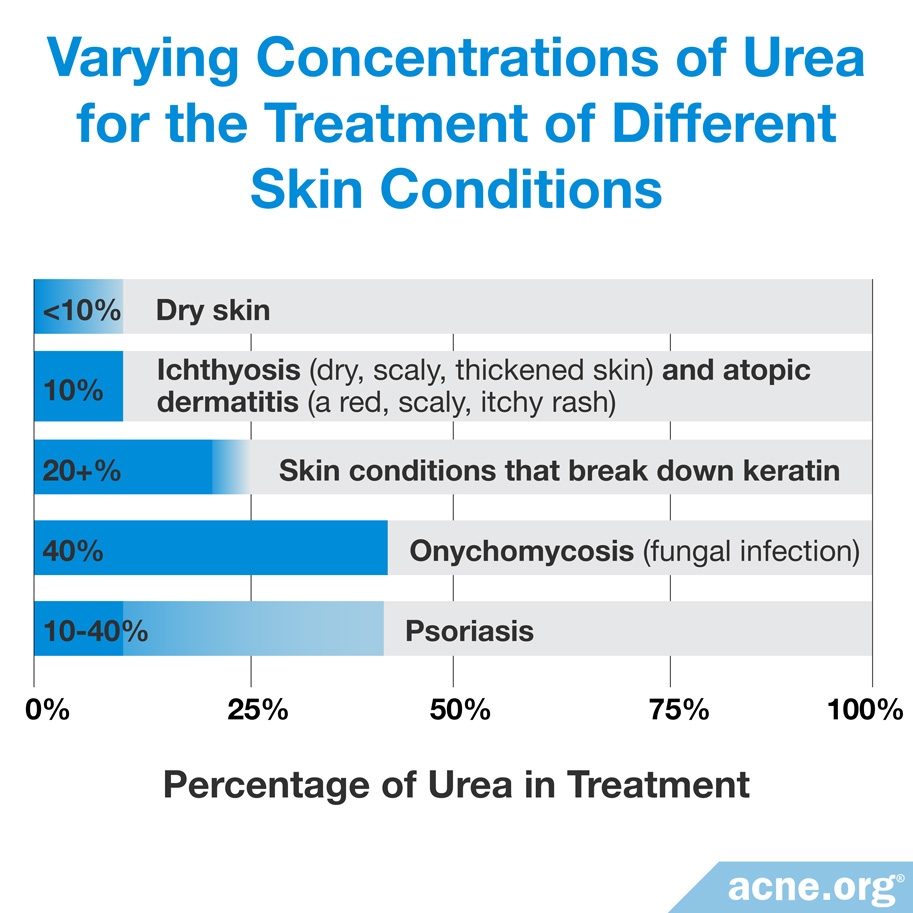
Varying Concentrations of Urea for Different Skin Conditions
Because urea performs multiple functions on the skin, doctors can prescribe and recommend it for a variety of skin concerns.
Products containing 10% urea and less usually are effective as skin moisturizers, whereas products containing 20% urea and more are effective in helping to break down keratin.6,9
Research indicates that the most commonly used concentrations of urea when treating dry skin are 10% and less. The most common concentration when treating ichthyosis (dry, scaly, thickened skin) and atopic dermatitis (a red, scaly, itchy rash) is about 10%. Products that are used to treat psoriasis vary in urea from 10% to 40%, and products that are used to treat a fungal infection called onychomycosis contain urea typically at about 40%.6,9
Urea is not regarded as an acne treatment, but it can be a welcome ingredient in moisturizers designed for acne-prone skin. Researchers agree that a weakened skin barrier may contribute to acne, and urea can help repair the skin barrier.16 However, it is important that the manufacturer tests the product to ensure that it does strengthen the skin’s protective barrier.
Side Effects
While urea typically causes few side effects, creams and lotions containing urea sometimes can bring about adverse skin reactions, such as stinging and smarting (a sharp, superficial sensation) after applying the urea-containing product.17
References
- Urea https://pdfs.semanticscholar.org/56a2/92d74e09090ae1bfce823b98a717111144bb.pdf
- Fowler, J. Understanding the role of natural moisturizing factor in skin hydration. Pract. Dermatol. 36 – 40 (2012). https://practicaldermatology.com/articles/2012-jul/understanding-the-role-of-natural-moisturizing-factor-in-skin-hydration
- Paris, J. & Parish, L. The use of urea in contemporary dermatology. J. Am. Acad. Dermatol. 60, P1636 (2009). https://www.jaad.org/article/S0190-9622(08)01876-8/fulltext
- Darlenski, R., Kazandjieva, J. & Tsankov, N. Skin barrier function: morphological basis and regulatory mechanisms. J. Clin. Med. 4, 36 – 45 (2011). https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&ved=2ahUKEwjj4oiDmMjmAhUCZc0KHXpmANkQFjAAegQIARAC&url=http%3A%2F%2Fwww.communitas-bg.org%2Fdownloads%2F41%2FSKIN%2520BARRIER%2520FUNCTION%3A%2520MORPHOLOGICAL%2520BASIS%2520AND%2520REGULATORY%2520MECHANISMS.pdf&usg=AOvVaw3MsZoDDNsQGBMyjKovqj_L
- Raab, R. P. Urea from the chemist’s point of view. J. Appl. Cosmetol. 9, 9 – 13 (1991). http://www.iscd.it/files/UREA-FROM-THE-CHEMIST-S-POINT-OF-VIEW.pdf
- Celleno, L., D’amore, A. & Cheong, W.K. The use of urea cream for hand eczema and urea foam for seborrheic dermatitis and psoriasiform dermatoses of the scalp. Clin. Cosmet. Investig. Dermatol. 11, 2445-2454 (2022). https://pubmed.ncbi.nlm.nih.gov/36387960/
- Kraft, J. N. & Lynde, C. W. Moisturizers: what they are and a practical approach to product selection. Skin Therapy Lett. 10, 1 – 8 (2005). https://www.ncbi.nlm.nih.gov/pubmed/15986082
- Pan, M. Heinecke, G., Bernardo, S., Tsui, C. & Levitt, J. Urea: a comprehensive review of the clinical literature. Dermatol. Online J. 19, 1 – 14 (2013). https://www.ncbi.nlm.nih.gov/pubmed/24314769
- Celleno L. Topical urea in skincare: A review. Dermatol. Ther. 31, e12690 (2018). https://www.ncbi.nlm.nih.gov/pubmed/30378232
- Grether-Beck, S., Felsner, I., Brenden, H. et al. Urea uptake enhances barrier function and antimicrobial defense in humans by regulating epidermal gene expression. J. Invest. Dermatol. 132, 1561 – 1572 (2012). https://www.ncbi.nlm.nih.gov/pubmed/22418868
- Banerjee, P. K., Choudhury, A. K. & Panja, S. K. Topical urea in dermatology. Indian J. Dermatol. 35, 17 – 24 (1990). https://www.ncbi.nlm.nih.gov/pubmed/2245997
- Gallinger, J., Kuhn, A., Wessel, S., Behm, P., Heinecke, S., Filbry, A., Hillemann, L. & Rippke, F. Depth-dependent hydration dynamics in human skin: Vehicle-controlled efficacy assessment of a functional 10% urea plus NMF moisturizer by near-infrared confocal spectroscopic imaging (KOSIM IR) and capacitance method complemented by volunteer perception. Skin Res. Technol. 28, 342-349 (2022). https://pubmed.ncbi.nlm.nih.gov/35034387/
- Lodén, M. Effect of moisturizers on epidermal barrier function. Clin. Dermatol. 30, 286 – 296 (2012). https://www.ncbi.nlm.nih.gov/pubmed/22507043
- Buraczewska, I. Berne, B., Lindberg, M., Torma, H. & Loden, M. Changes in skin barrier function following long-term treatment with moisturizers, a randomized controlled trial. Br. J. Dermatol. 156, 492 – 498 (2007). https://www.ncbi.nlm.nih.gov/pubmed/17300239
- Danby, S. G., Andrew, P. V., Taylor, R. N., Kay, L. J., Chittock, J., Pinnock, A., Ulhaq, I., Fasth, A., Carlander, K., Holm, T. & Cork, M. J. Different types of emollient cream exhibit diverse physiological effects on the skin barrier in adults with atopic dermatitis. Clin. Exp. Dermatol. 47, 1154-1164 (2022). https://pubmed.ncbi.nlm.nih.gov/35167133/
- Lynde, C. W., Andriessen, A., Barankin, B. et al. Moisturizers and ceramide-containing moisturizers may offer concomitant therapy with benefits. J. Clin. Aesthet. Dermatol. 7, 18 – 26 (2014). https://www.ncbi.nlm.nih.gov/pubmed/24688622
- Lodén, M. et al. A double-blind study comparing the effect of glycerin and urea on dry, eczematous skin in atopic patients. Acta Derm. Venereol. 82, 45 – 47 (2002). https://www.ncbi.nlm.nih.gov/pubmed/12013198
 Acne.org Products
Acne.org Products