Here are some of the screenshots that I took of people who had success. I'm not saying this is for everyone but I noticed Chiron (LDN ultimately worked), Washer, MovingOnMusicGal and Goosnargh all had good success taking it.
Just quit my 2nd course of accutaneshort after 3-4 months. 2 months in I started noticing shiny white/grey hairs on my head. This freaked me out. I also had extremely itchy head and some folloculitis which I have had before. Now that I've been off a month, I am noticing tons more shiny white hairs growing in. One of them tiny some of them more full. Also lots of my hairs are taking on a shine and almost appear to have me discoloration. I've scoured the internet and this thread and am coming up pretty lost on the subject. I know this thread is ongoing and anyone's help, advice, or comfort on the issue would be greatly appreciated.
8 hours ago, Chris16 said:
Yeah it is interesting that some people have responded well to LDN. My understanding is that it works on the immune system correct?
I might be wrong but LDN has nothing in common with either B12 or Iodine - Two popular paths people are currently pursuing on this forum with mixed results.
So my question is, does our main problem reside in fixing gut health where the immune system is??.....maybe!
4 hours ago, Quinn3 said:Just quit my 2nd course of accutaneshort after 3-4 months. 2 months in I started noticing shiny white/grey hairs on my head. This freaked me out. I also had extremely itchy head and some folloculitis which I have had before. Now that I've been off a month, I am noticing tons more shiny white hairs growing in. One of them tiny some of them more full. Also lots of my hairs are taking on a shine and almost appear to have me discoloration. I've scoured the internet and this thread and am coming up pretty lost on the subject. I know this thread is ongoing and anyone's help, advice, or comfort on the issue would be greatly appreciated.
Many people get grey beards at an earlier age than they'd expect. I also think a very high percentage get ginger in their beard which appears shiny.
I really don't think it's anything to do with accutane.
13 hours ago, TrueJustice said:Yeah it is interesting that some people have responded well to LDN. My understanding is that it works on the immune system correct?I might be wrong but LDN has nothing in common with either B12 or Iodine - Two popular paths people are currently pursuing on this forum with mixed results.
So my question is, does our main problem reside in fixing gut health where the immune system is??.....maybe!
I disagree. I think iodine and LDN both help with your immune system which is why some people see results. Everyone's body is differnt though so it may help others more.
From talking to others it seems the immune system and gut all come into play. This is why iodine works for some. It's like one of the strongest antibiotics you can take.
Oh and like Washer said, you have to take the right co factors when supplementing with iodine.
On 4/21/2017 at 5:34 PM, Colinboko said:Why am I experiencing such terrible voice loss/hoarseness..? I'm a singer (like professionally) so this definitely won't fly...
Could be an answer below?
Yes, gray hairs are common after Accutane treatment. Started when I was 20, months after accutane, around the time of the other side effects, it was just a couple hairs that I noticed, 8 years later and now its at about 30 or 40 gray colorless pigment hairs. Talk to any doctor about it and they'll just tell you its normal aging going into your 30's.
It's really not that complex, Accutane when it reaches its toxicity threshold in an individuals body probably shuts down the Pituitary gland and ceases GH production abruptly, earlier than say a naturally declining state.
Would be interesting to add into an orthopedic surgery list of questions whether the person/athlete had taken Accutane prior to injury (ligament, tendon, muscle tear) I think we'd all be surprised at the results.
38 minutes ago, macleod said:Yes, gray hairs are common after Accutane treatment. Started when I was 20, months after accutane, around the time of the other side effects, it was just a couple hairs that I noticed, 8 years later and now its at about 30 or 40 gray colorless pigment hairs. Talk to any doctor about it and they'll just tell you its normal aging going into your 30's.
It's really not that complex, Accutane when it reaches its toxicity threshold in an individuals body probably shuts down the Pituitary gland and ceases GH production abruptly, earlier than say a naturally declining state.
Would be interesting to add into an orthopedic surgery list of questions whether the person/athlete had taken Accutane prior to injury (ligament, tendon, muscle tear) I think we'd all be surprised at the results.
And of course the thinning of hair is also associated with it prematurely going grey, I've even got greys in my eyebrows.
All this doesn't bother me asmuch as the eye floaters, to of gotten them overnight after tane says it all really. Don't bother talking to your doctor about it though, they'll just say it's part of aging even though you might be only 24 years old....
Absolutely all the tests related to thyroid and iodine function, if you guys find anything let us know. Its best to have all the information possible and go from there. And then a few posts from someone who was looking into this exact same thing in 2013.
A full thyroid panel for hypothyroidism should at least include these 6 key thyroid lab tests:
TSH
Free T4
Free T3
Reverse T3
Thyroid Peroxidase Antibodies
Thyroglobulin Antibodies
NON-BLOOD TESTS
RADIOACTIVE IODINE UPTAKE
Because T4 contains much iodine, the thyroid gland must pull a large amount of iodine out from the blood stream in order for the gland to make an appropriate amount of T4. The thyroid has developed a very active mechanism for doing this. Therefore, this activity can be measured by having an individual swallow a small amount of iodine, which is radioactive. The radioactivity allows the doctor to track where the iodine molecules go. By measuring the amount of radioactivity that is taken up by the thyroid gland (radioactive iodine uptake, RAIU), doctors may determine whether the gland is functioning normally. A very high RAIU is seen in individuals whose thyroid gland is overactive (hyperthyroidism), while a low RAIU is seen when the thyroid gland is underactive (hypothyroidism). In addition to the radioactive iodine uptake, a thyroid scan may be obtained, which shows a picture of the thyroid gland
[Edited link out]
Iodine Blood Test
Iodine 24 Hour Urine
[Edited link out]
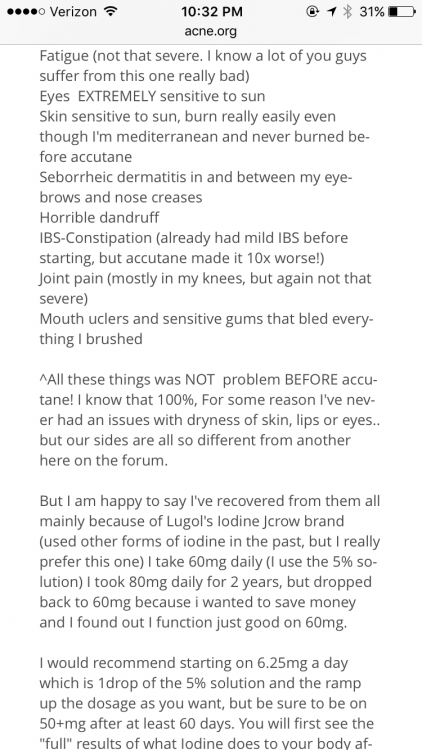
As most regulars are aware, my main issues resulting from tane use is hypothyroid like symptoms. Since coming off thyroid meds (5 months ago) i have felt like absolute shit however thyroid blood tests will tell you that I am still within normal reference range, despite having clear hypothyroid symptoms. Most on here know the importance of iodine to thyroid functioning so I got my iodine levels checked out and they are below range. Some brief research on iodine deficiency will tell you how it causes hypothyroidism (with the standard symptoms fatigue, sexual dysfunction, anxiety, low mood, dry skin, low temp, etc etc) and while blood levels can appear to be normal-ish.
Next i wanted to look at the link between tane and iodine. Retinoic acid had a direct effect on iodine metabolism, the following study shows that "Retinol was an inhibitor of TSHstimulated iodine metabolism"
Effects of Retinoids on Iodine Metabolism, Thyroid Peroxidase Gene Expression, and Deoxyribonucleic Acid Synthesis in Porcine Thyroid Cells in Culture
http://endo.endojournals.org/content/129/6/2827.short
If you check google there are loads of articles of 13cis retinoic acid being used in thyroid cancer treatment.
So clearly tane has a significant effect on iodine metabolism within our bodies. My latest theory is that low iodine levels could be a major problem as a result of tane use, causing a hypothyroid type condition, resulting in all the relevant symptoms.
Then someone asked how much iodine he was taking
I was on 50mg a day, but it caused pain and swelling in my thyroid, pretty sure it is an autoimmune response...hashimoto's most probably which makes perfect sense given my symptoms. Waiting on a new doc to get some thyroid autoimmune blood tests and some sort of scan of my thyroid/neck. Could be related to tane as tane has been known to trigger autoimmune disease in those prone to it (i.e crohns) or it could also be nothing to do with tane and I just happen to have a thyroid autoimmune disease.
On 4/25/2017 at 8:24 AM, guitarman01 said:Absolutely all the tests related to thyroid and iodine function, if you guys find anything let us know. Its best to have all the information possible and go from there. And then a few posts from someone who was looking into this exact same thing in 2013.
A full thyroid panel for hypothyroidism should at least include these 6 key thyroid lab tests:
TSH
Free T4
Free T3
Reverse T3
Thyroid Peroxidase Antibodies
Thyroglobulin Antibodies
NON-BLOOD TESTS
RADIOACTIVE IODINE UPTAKE
Because T4 contains much iodine, the thyroid gland must pull a large amount of iodine out from the blood stream in order for the gland to make an appropriate amount of T4. The thyroid has developed a very active mechanism for doing this. Therefore, this activity can be measured by having an individual swallow a small amount of iodine, which is radioactive. The radioactivity allows the doctor to track where the iodine molecules go. By measuring the amount of radioactivity that is taken up by the thyroid gland (radioactive iodine uptake, RAIU), doctors may determine whether the gland is functioning normally. A very high RAIU is seen in individuals whose thyroid gland is overactive (hyperthyroidism), while a low RAIU is seen when the thyroid gland is underactive (hypothyroidism). In addition to the radioactive iodine uptake, a thyroid scan may be obtained, which shows a picture of the thyroid gland[Edited link out]
Iodine Blood Test
Iodine 24 Hour Urine
[Edited link out]
As most regulars are aware, my main issues resulting from tane use is hypothyroid like symptoms. Since coming off thyroid meds (5 months ago) i have felt like absolute shit however thyroid blood tests will tell you that I am still within normal reference range, despite having clear hypothyroid symptoms. Most on here know the importance of iodine to thyroid functioning so I got my iodine levels checked out and they are below range. Some brief research on iodine deficiency will tell you how it causes hypothyroidism (with the standard symptoms fatigue, sexual dysfunction, anxiety, low mood, dry skin, low temp, etc etc) and while blood levels can appear to be normal-ish.
Next i wanted to look at the link between tane and iodine. Retinoic acid had a direct effect on iodine metabolism, the following study shows that "Retinol was an inhibitor of TSHstimulated iodine metabolism"
Effects of Retinoids on Iodine Metabolism, Thyroid Peroxidase Gene Expression, and Deoxyribonucleic Acid Synthesis in Porcine Thyroid Cells in Culture
http://endo.endojournals.org/content/129/6/2827.shortIf you check google there are loads of articles of 13cis retinoic acid being used in thyroid cancer treatment.
So clearly tane has a significant effect on iodine metabolism within our bodies. My latest theory is that low iodine levels could be a major problem as a result of tane use, causing a hypothyroid type condition, resulting in all the relevant symptoms.
Then someone asked how much iodine he was taking
I was on 50mg a day, but it caused pain and swelling in my thyroid, pretty sure it is an autoimmune response...hashimoto's most probably which makes perfect sense given my symptoms. Waiting on a new doc to get some thyroid autoimmune blood tests and some sort of scan of my thyroid/neck. Could be related to tane as tane has been known to trigger autoimmune disease in those prone to it (i.e crohns) or it could also be nothing to do with tane and I just happen to have a thyroid autoimmune disease.
I'd be interested if he was taking the co factors with iodine. You can't just take iodine on its own at high doses.
17 minutes ago, Chris16 said:I'd be interested if he was taking the co factors with iodine. You can't just take iodine on its own at high doses.
I think if some people feel that strongly about this, it would be good to get tested if possible. any tests that might reveal something could be a benefit to everyone. Ive had my tsh tested many,many times. I believe ive had my t4 and t3 tested. not reverse t3 and havent had antibody testing. I also have not had any iodine tests. Just looking for the quickest most effective way to rule things in and out by pooling our resources and seeing what we might have in common.
Like this. anyone got these mutations in common? Im TT
I know TrueJustice said he got diagnosed with non alcoholic fatty liver, wasnt that right? They tell you to take anything for this?
I wasnt a big believer in the past, but im starting to see how you could pin alot of this on liver functions and the subsistent consequences
| SNP:rs7946(C or T) onPEMT(chromosome 17) |
| TT | Moderately higher odds of developing Non-alcoholic fatty liver disease | |
| CC | Typical odds of developing Non-alcoholic fatty liver disease | |
| CT | Slightly higher odds of developing Non-alcoholic fatty liver disease |
Sign in to 23andMe to see your genotype for this SNP
This content has not been approved by 23andMe and is for informational purposes only.
Gene mutation contributes to liver disease in patients of normal weight
- Date:
- July 22, 2015
- Source:
- Kumamoto University
- Summary:
- Non-alcoholic fatty liver disease (NAFLD) is a major worldwide health problem. The disease is strongly associated with obesity and has been found in a high percentage Asian patients of normal weight. The PNPLA3 mutant genotype has been consistently shown to be a major factor in the development of NAFLD, but the effect of a patient's weight on the relationship between NAFLD and the mutant gene had not been determined until now, at the conclusion of a study on the issue.
@hatetaneGood video. Scary. It just goes to show you cant wait on doctors sometimes to figure things out for you.I still think its possible b12 could play a part in this. Ive been diagnosed with cerebral atrophy and one of the causes that can contribute to that is low b12 levels in the brain. or that time I smoked that bowl made out of aluminum foil. Kidding. No im not...
3 hours ago, guitarman01 said:Like this. anyone got these mutations in common? Im TT
I know TrueJustice said he got diagnosed with non alcoholic fatty liver, wasnt that right? They tell you to take anything for this?
I wasnt a big believer in the past, but im starting to see how you could pin alot of this on liver functions and the subsistent consequences
SNP:rs7946(C or T) onPEMT(chromosome 17)
TT Moderately higher odds of developing Non-alcoholic fatty liver disease CC Typical odds of developing Non-alcoholic fatty liver disease CT Slightly higher odds of developing Non-alcoholic fatty liver disease Sign in to 23andMe to see your genotype for this SNP
This content has not been approved by 23andMe and is for informational purposes only.
Gene mutation contributes to liver disease in patients of normal weight
- Date:
- July 22, 2015
- Source:
- Kumamoto University
- Summary:
- Non-alcoholic fatty liver disease (NAFLD) is a major worldwide health problem. The disease is strongly associated with obesity and has been found in a high percentage Asian patients of normal weight. The PNPLA3 mutant genotype has been consistently shown to be a major factor in the development of NAFLD, but the effect of a patient's weight on the relationship between NAFLD and the mutant gene had not been determined until now, at the conclusion of a study on the issue.
Yes, this is true. Nothing major came of it other than my doctor has had me change diet, do more exercise etc.
I got caught up doing many things last year, you can imagine my frustration at getting diagnosed with fatty liver after doing about 5 Moritz liver cleanses - quite a lot of effort is needed to do them by the book which I did only to get this diagnoses.
The most painful thing though that I had to get on top of was the reflux issue - had the cameras in both ends and got diagnosed with "herniated oesophagus" Now on Pariot prob for rest of life to combat reflux - this does the job.
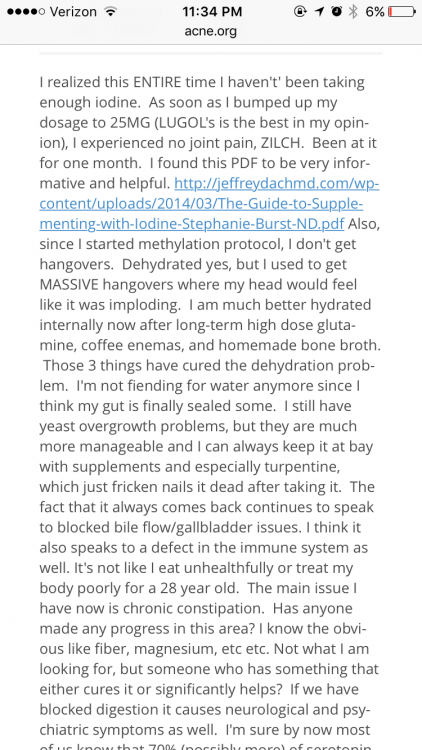
On another note, Iodine co factors are:
Selenium
Magnesium
Vit C
Vit B2/B3
No flush Niacin?
Inositol
There are obviously dosages that one must also follow too. This is from a supplement point of view but I'd imagine someone with hyperthyroid would possibly be on a drug of some sort over say just supplementing, having said that I don't know if anyone has developed this after Accutane? certainly not clear cut hyperthyroid that I know of, just the symptoms. That's the fucked thing after tane - nothing is ever conclusive which makes me wonder is it worth going for deeper thyroid tests only to be disappointed again, I've had that many blood tests in last 9 months, I've lost track of what the hell they've tested me for!!?
Supplementing might be a good place to start with thyroid, easy enough to quit them whenever you want I guess.
7 hours ago, TrueJustice said:Yes, this is true. Nothing major came of it other than my doctor has had me change diet, do more exercise etc.
I got caught up doing many things last year, you can imagine my frustration at getting diagnosed with fatty liver after doing about 5 Moritz liver cleanses - quite a lot of effort is needed to do them by the book which I did only to get this diagnoses.The most painful thing though that I had to get on top of was the reflux issue - had the cameras in both ends and got diagnosed with "herniated oesophagus" Now on Pariot prob for rest of life to combat reflux - this does the job.
On another note, Iodine co factors are:
Selenium
Magnesium
Vit C
Vit B2/B3
No flush Niacin?
InositolThere are obviously dosages that one must also follow too. This is from a supplement point of view but I'd imagine someone with hyperthyroid would possibly be on a drug of some sort over say just supplementing, having said that I don't know if anyone has developed this after Accutane? certainly not clear cut hyperthyroid that I know of, just the symptoms. That's the fucked thing after tane - nothing is ever conclusive which makes me wonder is it worth going for deeper thyroid tests only to be disappointed again, I've had that many blood tests in last 9 months, I've lost track of what the hell they've tested me for!!?
Supplementing might be a good place to start with thyroid, easy enough to quit them whenever you want I guess.
http://www.healthline.com/health/gerd/thyroid
Has anybody tried dopamine blockers such as Risperdal for the sexual dysfunction side effects of Accutane? As far as I can tell, Accutane can affect the dopamine systems of the brain. By upregulating dopamine receptors, as such the dopamine pathways are likely over stimulated and become desensitized. If you could use a dopamine receptor blocker, it would reduce dopaminergic firing, and then give you resensitization once you cease taking the dopamine blocker.
I know this sounds a bit crazy, but I saw post where one guy claimed this helped him regain his sex drive. I feel that this side effect bothers people the most. Thus it may be worth investigating. There is no doubt that dopamine signalling is responsible for libido and gaining pleasure from things like sex. Additionally, I experimented with Test Ethanate when I was 21, to see if this could help my Accutane induced sexual dysfunction. Despite going up to a high dose of 600mg/week at one point, I still noticed no change in libido. This would support the idea of Accutance somehow reducing dopamine sensitivity or dopaminergic firing.
In both of these studies, ISO treatment was cut short and it was suggested that the hyperhomocysteinemia seen during ISO therapy, which developed secondary to hepatic dysfunction, was associated with the inhibition of the cystathionine--synthase enzyme.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4248518/
I typed a bunch of stuff clicked submit and then the page went down. Awesome.
not typing all that again. Basically im looking into this. This could lead to elevated methionine levels in the blood that could eventually become a neurotoxin if this enzyme was still inhibited. And this is the 5th recent study now citing lower b12 levels associated with accutane treatment.
notes on b12,sublingual has not been proven more effective then oral. Also havent seen many studies showing Active b12 has been proven more effective then plain oldcyanocobalamin, which is much more researched. In fact, per mayo clinic, methyl forms of b12 are considered more unstable so much higher dosages are required.
When vitamin B12supply is low, the folate needed for DNA synthesis remains trapped in the methylation cycle and cell replication is impaired
CBS Mutations
CBS (cystathionine beta synthase) catalyzes the first step of the transsulfuration pathway, from homocysteine to cystathionine. CBS defects are actually an upregulation of the CBS enzyme. This means the enzyme works too fast. In these patients, it's common to see low levels of cystathionine and homocysteine since there is a rapid conversion to taurine. This leads to high levels of taurine and ammonia. The CBS upregulation has been clinically observed to result in sulfur intolerance in some patients. It has also been observed that BH4 can also become depleted with a CBS upregulation. BH4 helps regulate neurotransmitters and mood. Other mutations, such as MTHFR A1298C, Chronic bacterial infections, and aluminum can also lead to low BH4 levels. Lack of BH4 can lead to mast cell degranulation and possibly mast cell activation disorder (MCAD).
BH4 also serves as a catalyst for the production ofnitric oxide. Among other things, nitric oxide is involved invasodilation, which improves systematic blood flow. The role of BH4 in this enzymatic process is so critical that some research points to a deficiency of BH4 and thus, of nitric oxide as being a core cause of the neurovascular dysfunction
Conditions associated with untreated, aberrant methionine metabolism include, but are not limited to:
- Abnormal neurotransmitter metabolism and psychiatric disorders such as schizophrenia and bipolar disorder
- Neurodegenerative diseases
- Autism
- Dysregulation of nitric acid homeostasis
- Oxidative stress
- Global under-methylation, synthesis and repair of DNA
- Immune dysregulation/autoimmunity
- Cancer
- Cardiovascular disease
- Congenital heart disease and birth defects
- Impaired endogenous detoxification processes
- Increased risk for Down syndrome.
so if there was abnormal methionine metabolism would blood levels be elevated? simple as checking that?
is there a reason to test nitric oxide?
- First saliva nitric oxide test strip used by Olympians & pro athletes.
- Most affordable 10 strips with easy-to-use patented saliva absorption for rapid saliva collection and real-time testing.
- Individually sealed and durable for the active individual and athlete 'on the go'.
- Allows you to monitor your nitric oxide status to make dietary adjustment throughout the day.
- Saliva Nitric Oxide Test Strips are hand held strips that rapidly turn from white to deep pink based on the amount of a surrogate marker for Nitric Oxide. Within seconds, you are able to self-check and assess your Nitric Oxide status by comparing the intensity of the color on the Nitric Oxide Test strips to a color chart found on the Berkeley Test tube.
Methionine and Sulfur Metabolism Disorders
Disease (OMIM Number) | Defective Proteins or Enzymes | Defective Gene or Genes (Chromosomal Location) | Comments |
*Gene has been identified, and molecular basis has been elucidated. | |||
Disease (OMIM Number) | Defective Proteins or Enzymes | Defective Gene or Genes (Chromosomal Location) | Comments |
Homocystinuria(236200) | Cystathionine-synthase | CBS (21q22.3)* | Biochemical profile:Methioninuria, homocystinuria Clinical features:Osteoporosis, scoliosis, fair complexion, ectopia lentis, progressive intellectual disability, thromboembolism Treatment:Pyridoxine, folate,betainefor unresponsive patients, low methionine diet with some L-cysteine supplementation |
Methylenetetrahydrofolate reductase deficiency (236250) | Methylenetetrahydrofolate reductase | MTHFR (1p36.3)* | Biochemical profile:Low to normal plasma methionine, homocystinemia, homocystinuria Clinical features:Varies from asymptomatic to microcephaly, hypotonia, seizures, gait abnormality, and intellectual disability to apnea, coma, and death Treatment:Pyridoxine, folate (folic acid), hydroxycobalamin, methionine,betaine |
Methylmalonic acidemia-homocystinuria (cblE; 236270) | Methionine synthase reductase | MTRR (5p15)* | Biochemical profile:Homocystinuria, homocystinemia, low plasma methionine, no methylmalonic aciduria, normal B12and folate Clinical features:Feeding difficulty, growth failure, intellectual disability, ataxia, cerebral atrophy Treatment:Hydroxycobalamin, folate, L-methionine |
Methylmalonic acidemia-homocystinuria (cblG; 250940) | Methylene tetrahydrofolate homocysteine methyltransferase | MTR (1q43)* | Same as methylmalonic acidemia-homocystinuria cblE |
Hypermethioninemia (250850) | Methionine adenosyltransferase I and III | MAT1A (10q22)* | Biochemical profile:Elevated plasma methionine Clinical features:Mainly asymptomatic, fetid breath Treatment:None needed |
Cystathioninuria(219500) | -Cystathionase | CTH (16)* | Biochemical profile:Cystathioninuria Clinical features:Usually normal; intellectual disability reported Treatment:Pyridoxine |
Sulfite oxidase deficiency(606887) | Sulfite oxidase | SUOX (12q13)* | Biochemical profile:Elevated urine sulfite, thiosulfate, and S-sulfocysteine; decreased sulfate Clinical features:Developmental delay, ectopia lentis, eczema, delayed dentition, fine hair, hemiplegia, infantile hypotonia, hypertonia, seizures, choreoathetosis, ataxia, dystonia, death Treatment:No effective treatment |
Molybdenum cofactor defect (252150) | MOCS1A and MOCS1B proteins | MCOS1 (14q24)* | Biochemical profile:Elevated urinary sulfite, thiosulfate, S-sulfocysteine, taurine, hypoxanthine, and xanthine; decreased sulfate and urate Clinical features:Similar to sulfite oxidase deficiency but also urinary stones Treatment:No effective treatment Low sulfur diet possibly helpful in patients with milder symptoms |
Molybdopterin synthase | MCOS2 (6p21.3)* | ||
Gephyrin | GEPH (5q21)* | ||
Another way to maybe sniff out if anything abnormal was going on with b12
Cobalamin deficiency with and without neurologic abnormalities: differences in homocysteine and methionine metabolism.
Abstract
The unknown biochemical basis for neurologic dysfunction in cobalamin deficiency and the frequent divergence between neurologic and hematologic manifestations led us to study homocysteine metabolism in 22 patients with pernicious anemia. Serum levels of total homocysteine (tHcy), methionine, S-adenosylmethionine (AdoMet), cysteine, cysteinylglycine (cys-gly), and glutathione (GSH) were measured. Only levels of tHcy and cysteine were increased and only GSH was decreased in cobalamin deficiency as a whole, compared with 17 control subjects. AdoMet correlated only with methionine levels (P =.015) and cysteine only with cys-gly (P =.007) in healthy subjects, but in cobalamin-deficient patients AdoMet correlated instead with cysteine, cys-gly, and folate levels only (P =.008, P =.03, and P =.03, respectively). Significant differences appeared in clinically subgrouped cobalamin-deficient patients. The 11 patients with neurologic defects had higher mean levels of folate (27.9 versus 15.4 nM), AdoMet (117.2 versus 78.6 nM), cysteine (462 versus 325 microM), and cys-gly (85.0 versus 54.7 microM) than the 11 neurologically unaffected patients. Cobalamin therapy restored all metabolic changes to normal. The results indicate that changes in several metabolic pathways differ in patients with and without neurologic dysfunction. Cysteine levels were the most significant predictors of neurologic dysfunction, but it is unclear if they are direct or indirect indicators of neurotoxicity. The higher AdoMet levels in neurologically affected patients may result from inhibition of glycine N-methyltransferase by those patients' higher folate levels. The origin of the folate differences is unclear and possibly varied. Low AdoMet and GSH levels were independent predictors of anemia.
Could people who have experienced persistent sexual dysfunction/libido problems after using Accutane, comment with a contact email and maybe even some info about when they used Accutane, how it has affected their sexual function and how long this has been a problem.
If we have any chance of making any impact or persuading any researchers to look into this properly we need to be more organised, and able to be contacted to share important info.
 Acne.org Products
Acne.org Products