About a Third of Acne Scars Will Disappear on Their Own Within 6 Months. The Rest Are Likely Permanent but May Fade a Little over Time.

The Essential Info
Scarring after acne is very common. If an acne lesion simply leaves behind a red or dark mark, the mark may disappear on its own within a few months. However, if an acne lesion leaves behind an actual indented scar (one that looks sunken-in), there is a good chance the scar will be permanent but may fade a little over time. Unfortunately, some scars may also begin to look worse over time due to skin aging and sun damage.
One study that tracked acne scars up to 2 years found that scars tend to fall into one of three types:
- Short-term scars: About one-third of acne scars disappear on their own within half a year after forming.
- Medium-duration scars: Approximately 10% of acne scars disappear on their own sometime between half a year and 2 years after forming.
- Long-term scars: Approximately one-half of acne scars are still present 2 years after forming.
In addition, research suggests that all scars, not just acne scars, fade from red to pale over the course of about a year.

The Science
- Study Shows That about One-half of Acne Scars Are Likely Permanent
- What Research on Non-acne Scars Can Tell Us
- Preventing and Treating Acne Scars
- Risk Factors for Acne Scars
Over 90% of people with acne experience some amount of acne scarring, from barely noticeable in some cases to very severe in others.
Although scarring after acne is normal, scars can make a person feel self-conscious and impact their quality of life. Therefore, many people are anxious to know whether acne scars will fade on their own without treatment.
Let’s take a look at what science has to say regarding how long you can expect your scars to linger.
Study Shows That about One-half of Acne Scars Are Likely Permanent
One study has tracked acne scars to see what happens to them without treatment. The study closely monitored the patients for 6 months and also followed up with them 2 years later. Here are the take-away messages from this study:
- Acne scars fall into 3 types based on how long they last:
- Short-term scars: About one-third of acne scars disappear on their own within 6 months after forming.
- Medium-duration scars: About one-tenth of acne scars disappear on their own between 6 months and 2 years after forming.
- Long-term scars: About one-half of acne scars are still present 2 years after forming. The researchers wrote, “The majority…of the scars remaining at 6 months were still present at 2-year follow-up.”1 While the study didn’t follow up with the patients beyond 2 years, it’s likely the scars that lasted 2 years would end up being permanent.
Expand the section below if you would like to take a closer look at the study.
Expand to read details of study

This study was published in the Journal of the American Academy of Dermatology in 2015. The researchers looked at 32 volunteers with moderate acne from France and Canada. By examining the volunteers regularly over a period of 6 months, the researchers found that acne scars were continuously forming and made the following observations:
- Short-term acne scars: About 36% of the scars were transient, meaning they disappeared on their own during the 6-month study period. On average, a temporary scar lasted 41 days.
- Longer-term acne scars: About 64% of the scars were still around at the end of the 6-month study period. When the researchers followed up with the patients two years later, 81.7% of these scars were still there. They wrote, “The majority (81.7%) of the scars remaining at 6 months were still present at 2-year follow-up.” However, it is unknown whether the scars may have disappeared at some later period.1
Summing up the findings of this study, we can say that acne scars fall into the following three categories based on how long they persist:
| Duration | Percentage of all acne scars |
| Short-term (disappear in less than 6 months) | 36% |
| Medium-duration (disappear in 6 months-2 years) | 11.7% |
| Long-term (still present after 2 years) | 52.3% |
However, this was a small study based on only 32 participants. The researchers noted that more long-term studies should investigate what happens to acne scars beyond 2 years.1
We can also learn what to expect with untreated acne scars by looking at research on how other types of scars change over time.
What Research on Non-acne Scars Can Tell Us
One study, published in the journal Plastic and Reconstructive Surgery in 2008, experimentally created injuries and then tracked the resulting scars over the course of a year. Fifty-eight courageous men volunteered for this experiment. The researchers made two cuts on the inside of each volunteer’s arm. Each cut was 1 cm (about half an inch) long. The scientists then examined the cut skin and took pictures once a month for the next 12 months.2

The researchers observed the following:
- Scars fade but don’t disappear completely in one year: Over the course of a year, the scars changed in appearance, gradually moving from red, to pink, to white. However, the scars were still faintly visible at the end of a year.
- Scars heal faster in older adults: Scars progressed to a mature-looking, faded scar faster in men aged 55 and over faster than in younger men. Men younger than 30 years old were the most likely to have scars that healed slowly and remained red for up to three months.2
However, we should note that a cut made with a scalpel damages the skin in a different way than an acne lesion. Therefore, while these findings help us understand how skin healing progresses, they don’t necessarily help us predict exactly how long it will take for an acne lesion to heal.
Factors that determine how long a scar lasts
According to other studies, several factors besides age determine how long it takes for a non-acne scar to fade:
- Extent of the injury: The deeper and more extensive the injury, the longer the scar will take to fade.
- Individual variation in genes: Some people’s genetics predispose them to longer healing times.
- Ethnic background: Research suggests that people of certain ethnic backgrounds are more prone to some scar types, such as keloid scars (raised scars that grow beyond the edges of the original injury), and may also experience longer healing times.3
Despite these patterns, at this point we cannot predict how long a given scar will last. According to a 2017 article in the medical journal Scars, Burns & Healing, “Given all of the elements that affect scar formation, there’s no easy metric to use when predicting when a scar begins to fade.”3 In fact, some scientists speculate that some scars may even start to look worse over time due to aging and skin damage from sun exposure.4
Preventing and Treating Acne Scars
Prevention
When it comes to acne scars, “an ounce of prevention is worth a pound of cure.” There are two key steps you can take to minimize the formation of new acne scars:5
- Treat your acne: Research suggests that long, drawn-out inflammation in the skin is what triggers and worsens acne scarring. By treating your acne, you can reduce the severity of inflammation in your skin and minimize scarring. According to a 2017 article in the Journal of Clinical and Aesthetic Dermatology, “Early treatment of active acne remains the best way to prevent or limit acne-related scarring.”6
- Never pick at your skin: Picking at your acne lesions irritates the skin, boosting the inflammation happening under the surface. As we have already discussed, increased inflammation leads to increased scarring, so don’t pick!
Treatment
For scars that have already formed, many treatment options are available. However, since most scars are painless (with the exception of some keloid scars), it is not necessary to treat them unless you feel they are detracting from your quality of life. The American Association of Dermatologists recommends that doctors use the following questions to determine whether acne scars are worsening a patient’s quality of life:7
- Do you often wish you could get rid of your acne scars?
- Do you feel that your scars limit your opportunities to date, get a job, advance your career, or perform well in school?
- Are you less social now than before you had acne scars?
If you answered yes to any of these questions, this suggests that your scars may be interfering with your social life and emotional well-being and that you may want to consider scar treatment.
Specific treatments will depend on the type, size, and severity of your scars. Feel free to research the options here at Acne.org as well as consult your doctor to decide on the best options for you. Many scar treatments require multiple sessions to be effective, and often, doctors will recommend combining two or more different types of treatments for best results.4,8,9,
Finally, remember that you need to clear your skin of any existing acne before embarking on scar treatment. Otherwise, you may end up chasing scars around your face, treating older scars while new scars continue to form.210 As a 2017 article in the Journal of Clinical and Aesthetic Dermatology puts it, “It is…imperative to ensure active acne has been treated before approaching scar treatment so as not to create a cycle where active lesions continue to scar in areas already addressed.”6
Risk Factors for Acne Scars
Why some acne lesions leave a scar and others don’t continues to be a topic of intense research. So far, researchers have noted the following risk factors that increase the chances of scarring:
- Acne severity: More severe acne tends to mean more severe inflammation, which, in turn, is likely to lead to more scarring.
- Types of acne lesions: One study found that only 2% of acne scars came from whiteheads and pustules. The vast majority of scars resulted from papules and from dark/red marks left over from acne lesions (this is called post-inflammatory hyperpigmentation and is, as the name implies, a result of inflammation in the skin during acne).1
- How long acne stays untreated: The longer you leave acne untreated, the more inflammation has a chance to run wild, increasing the risk of scarring.
- Gender: Males appear to be at greater risk for acne scars compared to females.
- Genetics: A family history of acne scarring makes a person more likely to develop acne scars. This suggests that genetics is a factor, and researchers are starting to identify specific genes that predispose people to scars.6,11,12
Risk factors for raised scars
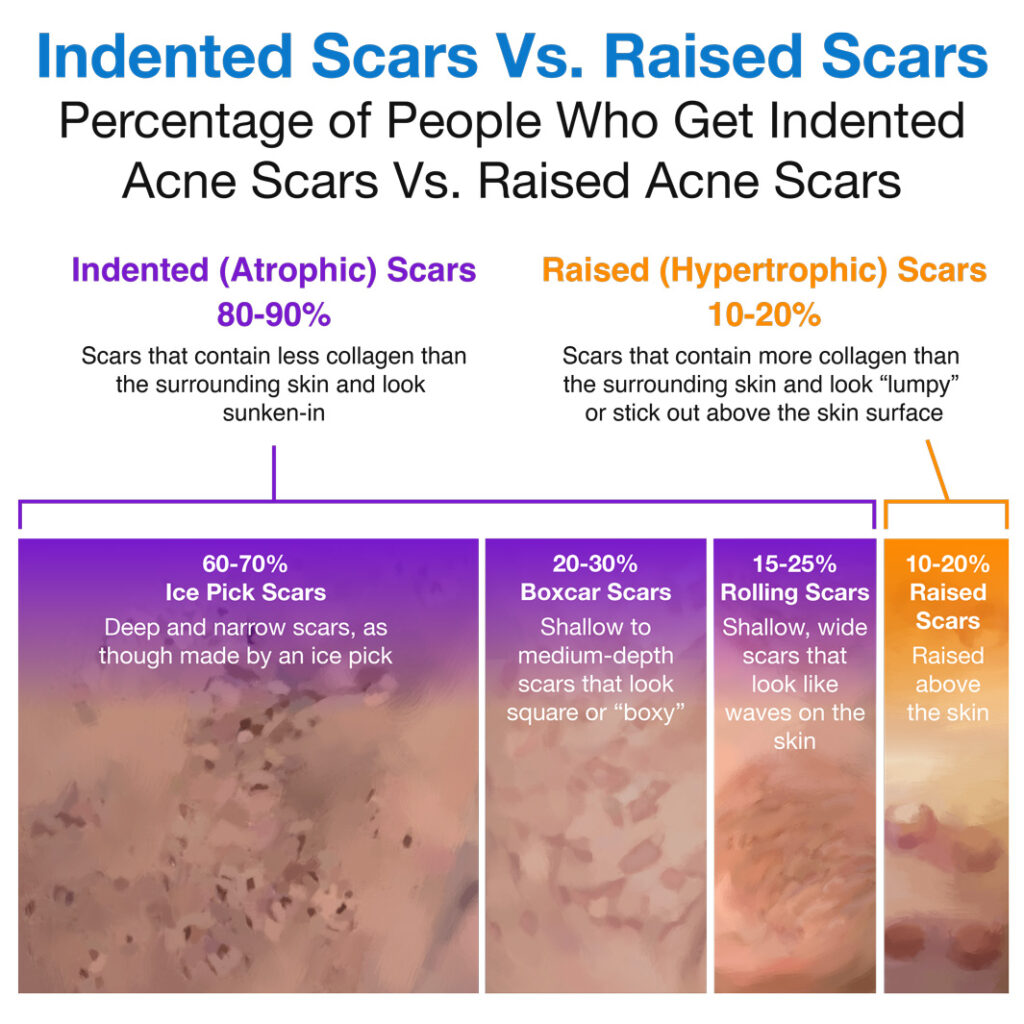
Raised scars are scars that stick out above the skin surface, and they account for about 10-20% of all acne scars.5,13
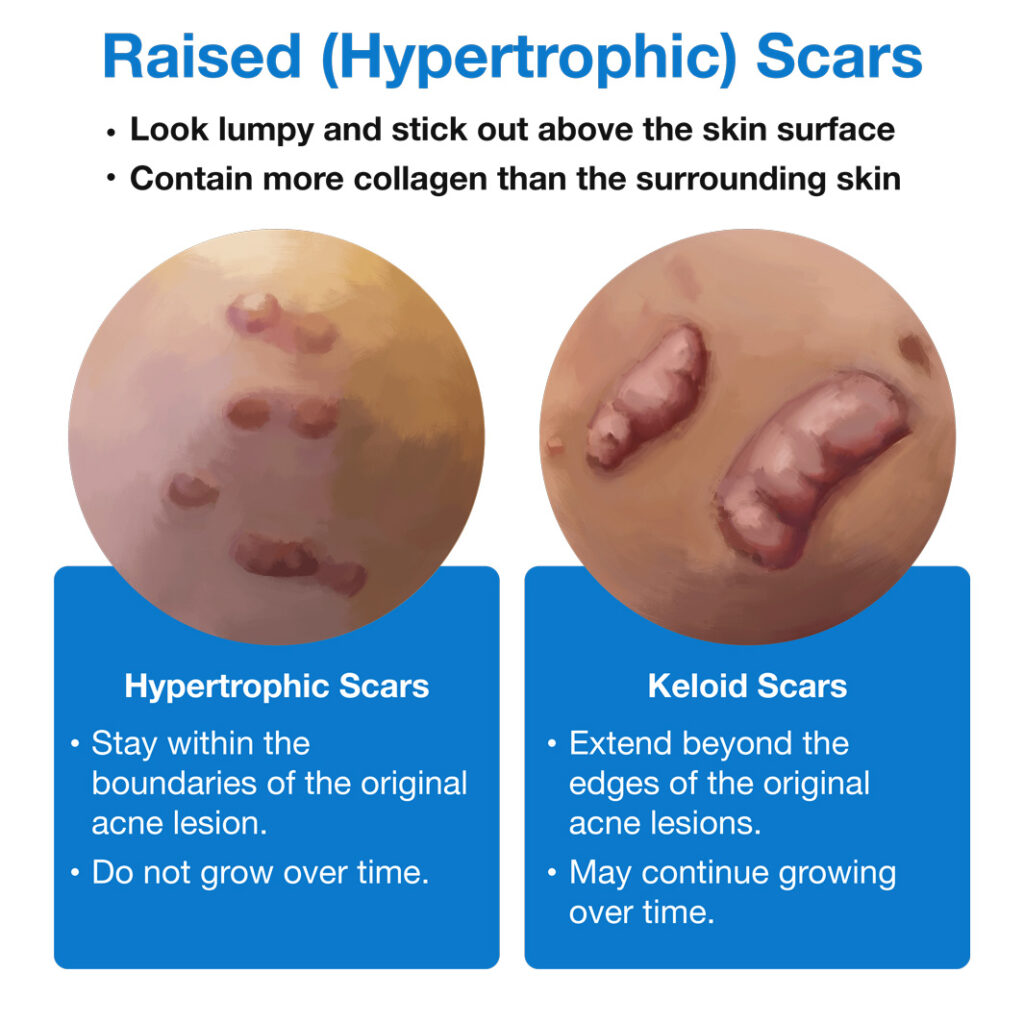
Researchers have identified many risk factors for developing raised scars:
- Age: People under 30 years old are at greater risk for developing raised scars, particularly keloid scars, than those who are older.
- Ethnic background: People of certain ethnicities, such as those of African or Afro-Caribbean descent, are more likely to develop raised scars.
- Family history: People whose relatives have raised scars are more prone to developing these types of scars.
- Location on the body: Certain areas of the body have higher skin tension, which means the skin in these areas is more tightly stretched. Such areas include the shoulder, back, and chest. These areas are more likely to develop raised scars.
- Duration of inflammation: Just as with other types of acne scars, raised acne scars are more likely to form in skin where inflammation has been present for a long time.
- Hormonal fluctuations: People are more likely to develop raised scars during puberty and pregnancy, two periods when hormone levels are fluctuating.14-16
References
- Bourdes, V. et al. Modeling of natural history of primary acne lesions and evolution to acne scars. Journal of the American Academy of Dermatology 72, AB8 (2015). https://www.jaad.org/article/S0190-9622(15)00160-7/fulltext
- Bond, J. S. et al. Maturation of the human scar: An observational study. Plastic and Reconstructive Surgery 121, 1650–1658 (2008). https://pubmed.ncbi.nlm.nih.gov/18453989/
- Kravvas, G. & Al-Niaimi, F. A systematic review of treatments for acne scarring. Part 1: Non-energy-based techniques. Scars, Burns & Healing 3, 205951311769531 (2017). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5965325/
- Fife, D. Practical evaluation and management of atrophic acne scars: Tips for the general dermatologist. The Journal of Clinical and Aesthetic Dermatology 4, 50-7 (2011). https://jcadonline.com/practical-evaluation-and-management-of-atrophic-acne-scars-tips-for-the-general-dermatologist/
- Fabbrocini, G. et al. Acne scars: Pathogenesis, classification and treatment. Dermatology Research and Practice 2010, 893080 (2010). https://pubmed.ncbi.nlm.nih.gov/20981308/
- Connolly, D., Vu, H. L., Mariwalla, K. & Saedi, N. Acne scarring- pathogenesis, evaluation, and treatment options. Journal of Clinical and Aesthetic Dermatology 10, 12–23 (2017). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5749614/
- American Academy of Dermatology. Acne scars: Diagnosis and treatment. https://www.aad.org/public/diseases/acne/derm-treat/scars/treatment
- Werschler, W. P., Herdener, R. S., Ross, V. E. & Zimmerman, E. Critical considerations on optimizing topical corticosteroid therapy. The Journal of Clinical and Aesthetic Dermatology 8, S2-8 (2015). https://pubmed.ncbi.nlm.nih.gov/26392839/
- Ravenscroft, J. Evidence based update on the management of acne. Archives of Disease in Childhood: Education and Practice Edition 90, 98–101 (2005). https://ep.bmj.com/content/90/4/ep98
- Dréno, B. et al. Prevention and reduction of atrophic acne scars with adapalene 0.3%/benzoyl peroxide 2.5% gel in subjects with moderate or severe facial acne: Results of a 6-month randomized, vehicle-controlled trial using intra-individual comparison. American Journal of Clinical Dermatology 19, 275–286 (2018). https://pubmed.ncbi.nlm.nih.gov/29549588/
- Fife, D. & Zachary, C. B. Combining techniques for treating acne scars. Current Dermatology Reports 1, 82–88 (2012). https://link.springer.com/article/10.1007/s13671-012-0011-0
- Tan, J., Kang, S. & Leyden, J. Prevalence and risk factors of acne scarring among patients consulting dermatologists in the USA. Journal of Drugs in Dermatology 16, 2 (2017). https://jddonline.com/articles/dermatology/S1545961617P0097X
- Bijlard, E. et al. A systematic review on the prevalence, etiology, and pathophysiology of intrinsic pain in dermal scar tissue. Pain Physician 20, 1–13 (2017). https://pubmed.ncbi.nlm.nih.gov/28158149/
- Tziotzios, C., Profyris, C. & Sterling, J. Cutaneous scarring: Pathophysiology, molecular mechanisms, and scar reduction therapeutics: Part II. Strategies to reduce scar formation after dermatologic procedures. Journal of the American Academy of Dermatology 66, 13–24 (2012). https://pubmed.ncbi.nlm.nih.gov/22177632/
- Aydoğmuş, S. et al. Factors affecting the development of scar formation in abdominal surgery performed for gynecologic and obstetric conditions. Arch Dermatol Venereology 51, 12–19 (2017). https://www.semanticscholar.org/paper/Factors-affecting-the-development-of-scar-formation-Aydogmus-Kelek%C3%A7i/4bf24518e010bda0e635e1efe5d4ccc3ad486a61
- Wolfram, D., Tzankov, A., Pülzl, P. & Piza-Katzer, H. Hypertrophic scars and keloids—A review of their pathophysiology, risk factors, and therapeutic management. Dermatologic Surgery35, 171–181 (2009). https://pubmed.ncbi.nlm.nih.gov/19215252/
 Acne.org Products
Acne.org Products