How did I get these antibodies?
Most the time, doctors do not know why some people get antiphospholipid antibodies. In a small number of people, an infection or drug caused the antibody.
(im sure this could apply to numerous types of antibodies triggered by a drug)
Antiphospholipid syndrome (APS) is an immune disorder that commonly manifests with a variety of CNS effects.
Moderate/severe erectile dysfunction in patients with antiphospholipid syndrome.
CONCLUSION:
To our knowledge, this was the first study that demonstrated moderate/severe ED in almost 50% of cases of a rare autoimmune disease. This alteration was linked to arterial events and longer disease duration.
Association between isotretinoin use and central retinal vein occlusion in an adolescent with minor predisposition for thrombotic incidents: a case report
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2649144/
An otherwise healthy 17-year-old white man who was treated with systemic isotretinoin for recalcitrant acne was referred with central retinal vein occlusion in one eye. Although a detailed investigation was negative, DNA testing revealed that the patient was a heterozygous carrier of the G20210A mutation of the prothrombin gene. Despite the fact that this particular mutation is thought to represent only a minor risk factor for thromboses, it is probable that isotretinoin treatment greatly increased the risk of a vaso-occlusive incident in this patient.
the drug appears to act on the coagulation process by a still unexplained mechanism.
This is quite interesting too i believe.
You will recall that one of the Genes selected by the Network Analysis i provided has selected MERTK. I added to string-db the term MERTK in order to find associated Genes :
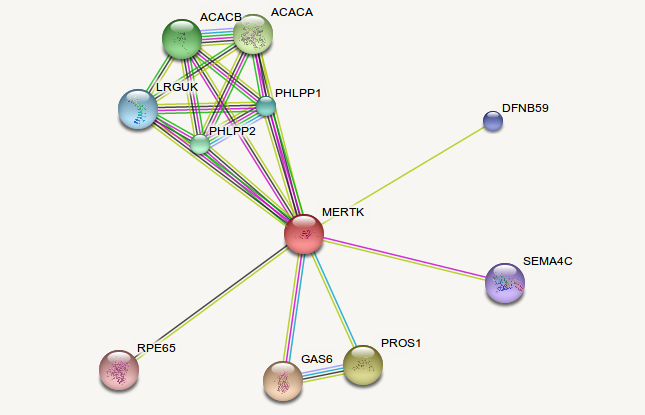
You may also see GAS6 (also selected by the Network Analysis i provided)
Next we have the following :
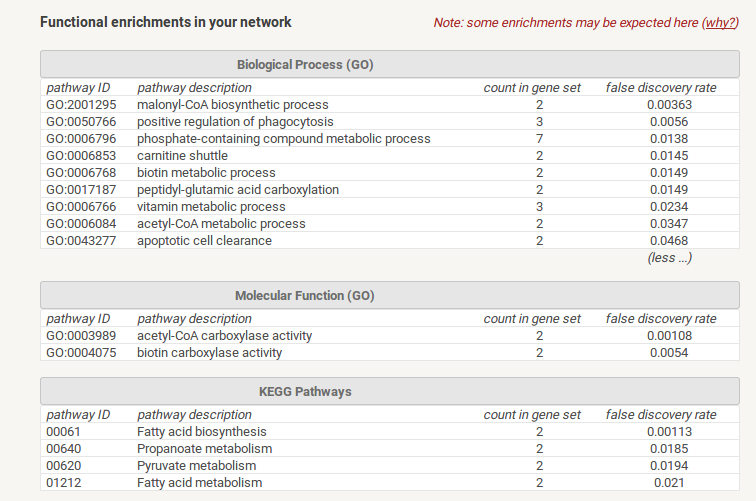
Notice the lines having as entries :
1) Biotin
2) acetyl-coa Metabolic Process
3) Fatty acid biosynthesis
4) Fatty acid Metabolism
5) Pyruvate Metabolism (...!!!)
Then we have the CFS Study by Fluge mentioning impaired Pyruvate Dehydrogenase function!
QuoteMetabolic profiling indicates impaired pyruvate dehydrogenase function in myalgic encephalopathy/chronic fatigue syndrome
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5161229/
@mariovitali Good stuff. I've been following the gist of your recent posts and wanted to mention that I went years believing I may have CFS before making a solid connection to using Accutane when the nightmare began. ...Main reason was simply that I was chronically fatigued and in pain from the time I went on the drug until a few years ago, when these symptoms lifted. There didn't seem to be the large subgroup of CFS patients with sexual symptoms and severe depression, as there are with post-Accutane, but I may have missed them. Either way, thanks for enlightening some of the post-Accutane folks on the CFS forums.
Have been thinking of collecting sets of differentially expressed genes from studies of Accutane, SSRI, and 5-ari drugs, and running them through pathway analysis tools to find possible overlapping effects:
https://david.ncifcrf.gov/
http://pantherdb.org/index.jsp
Have you tried this yet, or have you been focused on starting with symptomatology of the patient groups you are looking at?
Is the software you have been using available as a web-based application?
Thank you for your post. I haven't tried this because -in full honesty- i have no idea how to do it. The tool i use basically generated Hypotheses on the most likely aetiologies of these syndromes. Yet one more tool i use, reads 23andme Data and identifies all relevant SNPs that need to be looked at. As an example , if SUOX/CDO1 SNPs are found then we most likely need to support Sulfation with Low dose Molybdenum and B2.
I strongly believe that the software #1 repeatedly was able to identify important information (relevant Genes and Pathways) and all results are reproducible. Unfortunately it is not available as a Web-based application.
Also in full knowledge of what i am saying here, the latest case is a 37- year old woman having a mixture of CFS/Fibro, Depression, Constipation, Loss of Libido and many other neurological symptoms and hormonal symptoms (including premature menopause which was slowly reversed) being 90% well after 25 years of disease (Post-Accutane). This happened within 10 weeks. This is why i asked if there is some organization of the Post-Accutane sufferers so we may readily start (=evaluate these Hypotheses by Medical Personnel). Needless to say that this patient does not believe on what she experiences and believes that there may be a relapse.
Very soon i will disclose the main node of the Network Analysis on my Blog so all of this is somehow documented. I wil also post some excerpts from-probably- one of the most interesting Papers i've ever read.
I will help in any way i can, no compensation involved, but this effort has to be properly evaluated by Medical researchers. Unfortunately this is easier said than done as over and over i hit a wall when it comes to having *any* researcher evaluate the findings of my Research.
@Dubya_B@tanedout
I was in shock to see this. The OMF has appointed Fluge and Mella (both trying to use Rituximab) for CFS/ME patients.
Excerpts from a site i found on Rituximab :
QuoteRituximab is marketed with black box warnings about a number of serious side effects that can cause death and disability. It is given intravenously; infusion reactions are common, and severe infusion reactions have been fatal. Infusions require premedication and special safety precautions. Infusion reactions occur in up to 50% of patients, usually with the first dose; they typically develop within 30 minutes to 2 hours but can be delayed for up to 24 hours. Severe mucocutaneous reactions can also be fatal. Hepatitis B virus can be reactivated. Fatal bacterial, fungal, and viral infections can occur. It can cause cardiac arrhythmias, renal toxicity, bowel obstruction and perforation, and many other side effects.
<SNIP>
QuoteAt the time I wrote, there were two more studies pending, both open label and without a control group.One of those is still ongoing.The other has been completed. It found an improvement in self-reported fatigue scores in 64% of patients. It took an average of 23 weeks to see improvement. 14 patients had a major response lasting an average of 105 weeks; 4 had a moderate response lasting 69 weeks. 18 of the 28 subjects were the same individuals who had participated in the 2008 randomized study. Adverse events included two allergic reactions, two episodes of neutropenia, and eight transient symptom flares. One major responder dropped out after 32 months when he experienced a full relapse. Since there was no control group, its hard to judge what these results mean.
<SNIP>
QuoteWhitney isfeatured in a videothat also features Dr. Kogelnik and his Open Medicine Institute. He posts as Whit on the Phoenix Rising forum. In December 2012 he was able to writean articulate, coherent post. He apparently was started on rituximab by Dr. Kogelnik in January 2013 and rapidly went downhill. By Aprilhe posted Cant read much now
The treatment costs $40K
https://sciencebasedmedicine.org/chronic-fatigue-syndrome-rituximab-revisited/
7 hours ago, mariovitali said:Also in full knowledge of what i am saying here, the latest case is a 37- year old woman having a mixture of CFS/Fibro, Depression, Constipation, Loss of Libido and many other neurological symptoms and hormonal symptoms (including premature menopause which was slowly reversed) being 90% well after 25 years of disease (Post-Accutane). This happened within 10 weeks. This is why i asked if there is some organization of the Post-Accutane sufferers so we may readily start (=evaluate these Hypotheses by Medical Personnel). Needless to say that this patient does not believe on what she experiences and believes that there may be a relapse.
What protocol did she follow Mario? Is there a thread on PR where she has posted the details of what she did to recover? Great to hear she is 90% better!
Her regimen is personalised. This means that if a person is given -say- Molybdenum for supporting Sulfation, for another individual it may be toxic.
This is why i insist that this Research should be investigated under controlled conditions and under the supervision of Medical Personnel. My Goal is to gather around 20 people that became symptom-free and then -as a group- ask for Research done on the specific kind of regimen and Hypothesis on what is going on.
She is not on PR but she is ready to talk to a Research team with her real name if i ask her to do so.
Im thinking some of what's going on here could be cardiovascular related. Maybe even at the root of CFS? Chronic fatigue syndrome as a legitimate medical term is relatively new and that im sure a lot of doctors still don't recognize or even acknowledge it exists.
I wonder if there is a shortened life expectancy associated with chronic fatigue?You would almost think there would have to be, with all the extra physical and mental stress.
Some studies are pointing to Accutane being capable of cardiovascular remodeling. With so many possibilities its hard to find a traceable cause.
I guess thats why process of elimination (at least for what can be tested) makes the most sense to me.
Here is just one example of probably thousands of possibilities. So you start to see some organ dysfunction, it could literally be a blood flow issue.
this would im sure affect the smallest blood vessels first. the ones that are hardest to test.
Zinc: an important cofactor in haemostasis and thrombosis.
Abstract
There is mounting evidence that zinc, the second most abundant transition metal in blood, is an important mediator of haemostasis and thrombosis. Prompted by the observation that zinc deficiency is associated with bleeding and clotting abnormalities, there now is evidence that zinc serves as an effector of coagulation, anticoagulation and fibrinolysis. Zinc binds numerous plasma proteins and modulates their structure and function. Because activated platelets secrete zinc into the local microenvironment, the concentration of zinc increases in the vicinity of a thrombus. Consequently, the role of zinc varies depending on the microenvironment; a feature that endows zinc with the capacity to spatially and temporally regulate haemostasis and thrombosis. This paper reviews the mechanisms by which zinc regulates coagulation, platelet aggregation, anticoagulation and fibrinolysis and outlines how zinc serves as a ubiquitous modulator of haemostasis and thrombosis
^but i can tell you zinc is capable of raising blood pressure as well.
Not much to it. Someone showed me how to use several bioinformatics tools, and they have proven invaluable. Briefly, I will explain how to use DAVID and KOBAS. You will surely understand it once you see it in action.
Here is a list of genes with >2.0 fold-change from a study called "Temporal changes in gene expression in the skin of patients treated with isotretinoin provide insight into its mechanism of action":
- Go to DAVID Functional Annotation Tool: https://david.ncifcrf.gov/summary.jsp
- Select "Upload" on the left-hand side of screen.
- Copy/paste the above list into input box and select "Official_Gene_Symbol" from "Select Identifier" drop-down list. Tick "Gene List" radio button as "List Type"
- You will be prompted to select species. Choose "Homo sapiens" from combo box
- Select "Background" on the left-hand side of screen.
- Choose "Homo sapiens" from list and click "Use"
- Click "Start Analysis" on navigation bar or select "Functional Annotation Clustering" buttons
You should see different biological pathways associated with the differentially expressed genes. If you set it to the highest stringency, you can see the cholesterol, sterol, and steroid biosynthetic pathways are strongly associated with the list of genes.
I like the reports generated by KOBAS 3.0 better: [Edited link out]
...but you have to convert the list of gene ID names to Entrez or Ensemble IDs using a tool like this: http://biodb.jp/
I ran the converted list of Ensemble IDs through KOBAS and only used the disease databases. This showed the FADS1 and FADS2 genes, that were both decreased ~3.5 fold in the "Temporal Changes" study, are associated with Crohn's, Ulcerative Colitis, and Inflammatory Bowel Disease. Looking at the literature, decreases in metabolism of these enzymes and decreases in their transcription are strongly associated with IBD sand Crohn's, both supposed side-effects of Accutane/Isotretinoin. The MUC1 (mucin) gene, that promotes maintenance of the mucus-lining of intestinal tract was also associated with these diseases and decreased many-fold in the "Temporal Changes" study.
I really tried but couldn't go through this and spend too much time (DAVID didn't seem to be working) . Could we set up a Skype call ?
PM me when you can. Thanks!
I have also used Malacards, here is an example for FADS2
http://www.malacards.org/search/results/FADS2
This looks like a good website to report sides, and it looks like at least some people are paying attention.
One hundred and twenty cases of enduring sexual dysfunction following treatment.
Abstract
BACKGROUND:There have been reports for over a decade linking serotonin reuptake inhibitors, finasteride and isotretinoin with enduring sexual dysfunction after treatment stops.
OBJECTIVE:To explore the clinical pictures linked to all 3 drugs.
METHODS:We have selected 120 reports to RxISK.org reporting the problem and mined these for data on age, gender, drug of use, and impact of the problem.
RESULTS:The data make it clear that the three drugs show extensive overlap in symptom profile, regardless of sex or country of origin.
CONCLUSIONS:The availability of 120 reports from over 20 countries add to the case for the validity of the syndrome. This is severe and enduring condition can result in death. An understanding of its physiology and an approach to treatment are needed.
PMID
24902508 [PubMed - indexed for MEDLINE]
Possibly some useful information here. I've mentioned in the past ive seemed to feel pretty good at times just taking something like claritin and even a h2 blocker like zantac.
Put that on your list of tests. Histamine. I remember someone posting they had high levels of histamine in the blood, but they didnt have allergies.
Histamines and Anticoagulants areview
https://cfsremission.com/2014/03/23/histamine-and-anticoagulants/
A good friend is testing theexcessive histamine modelas a significant vector for CFS. This model does fit with the dysfunctional microbiome model because gut bacteria changes histidine into histamine. The friend is showing significant signs of improvement (with a lot of symptom changes).
I was asked to double check my usual list of anti-coagulants against histamine influence. These are notes that I extracted my reference book and PubMed review.There are three supplements that appear to reduce histamine levels, improve cognitive function and reduce coagulation (thick blood):
- Alpha Lipoic Acid
- Turmeric
- Vitamin D3
Choline
In CFS patients this is important because it impacts cognitive function:
- Relatively high inoccipital cortexof the brain
- Abnormally high in general
- Improves with viral clearance, resulting insignificant improvements in verbal learning, memory, and visual-spatial memory
- Normalizes withTurmeric(curcumin reduces histamine levels [2014] [2013])
- Normalizes withAlpha Lipoic Acid(reduces histamine levels [2010] [2010])
Alpha Lipoic Acid
- Decreases CD62P platelet expression
- Decreases CRP levels by 19%
- Decreases fibrinogen, factor VII, vWF, and triglycerides
- Decreases plasma levels of free fatty acids, triglyceride, total cholesterol, low density lipoprotein-cholesterol, small dense LDL-cholesterol, oxidized LDL-cholesterol, very low density lipoprotein-cholesterol
- Decreases symptoms of neuropathy and neuropathic deficit
- Decreases TNF, IL-6
- Improves blood flow and nerve function
Turmeric
The active ingredient of this kitchen spice is curcumin. Turmeric may be more effective than curcumin, the extract. Curcumin has anti-inflammatory, anti-oxidant, pro-apoptotic, chemo preventive, chemotherapeutic, anti-proliferative, wound healing, anti-parasitic, anti-malarial and anti-bacterial activity. Although inexpensive, apparently well tolerated and potentially active, curcumin has not been approved for the treatment of any human disease.
- Benefits IBS
- Bioactivity is increased by adding 1% black pepper
- Increases fibrinolytic activity
- Inhibits platelet aggregation, increases coagulation time
- Inhibits EBV, antiviral
- Inhibits H. pylori
- Inhibits inducible nitric oxide synthase (iNOS)
- Neuroprotective
- Reduces high level of fibrinogen
- Reduces IL6, IL8, TNF
Vitamin D3
- 22% 65% of CFS patients are deficient (less than 20 ng/mL)
- 61% 80% of Fibromyalgia patients are deficient (less than 20 ng/mL)
- Associated with headaches, hypersomnia
- Associated with orthostatic intolerance
- Hypersomnia eliminated with supplements
- Improvement became more significant with FM when blood level of 25(OH) D exceeded 50 ng/ mL (125 nmol/L)
- Moderately to severely sub-optimal in CFS patients
- Remission seen with 200010000 IU/day (with magnesium and phosphate)
- Treatment with high-dose vitamin D resulted in clinical improvement in all FM patients
- With myalgia in statin-treated patients, 92% were resolved when levels reached 50 ng/mL (125 nmol/L)
- Patients with 25-OHD less than 20 ng/ml (50 nmol/L) are more likely to have
- impaired short memory
- confusion
- mood disturbance
- sleep disturbance
- restless leg syndrome
- palpitation
- Inhibits thrombus formation[2014]
- Attenuates platelet activation [2011]
- Low levels seen with antiphospholipid syndrome (APS) with thrombotic disease[2012] (a variation of APS is Dave Bergs Hemex model of CFS)
- Reduces histamine levels [1996] [1995] [2014]
- A dosage to discuss with you health profession may be 15,000 to 20,000 IU/day for a few months.
To Be Avoided Anticoagulants
Aspirin (I would question this to some extentbecause baby aspirin/aspirin has been extensively studied as therapeutic or necessaryin some vascular diseases)
- aspirinenhancedhistaminerelease [2013]
Bromelain
- AVOID: allergic reaction is known to happen with this [Edited link out] which implies histamine release.
Other OTC anti-coagulants
Serrapeptase
- Anti-inflammatory
- Effective for inflammatory venous disease
- Improves antibiotic concentration up to 850%
- Inhibits the formation of biofilms
- No information on Histamine or Mast Cell impact
Nattokinase
- Anti-hypertensive
- Cleaves cross-linked fibrin
- Decreases red blood cell aggregation and shear-viscosity of blood cells
- Inactivates plasminogen activator inhibitor type 1 and then potentiates fibrinolytic activity
- Increases activated factor VII levels
- No information on Histamine or Mast Cell impact
Lumbrokinase
- Anti-thrombotic
- Digests fibrinogen and inhibits platelet adhesion
- Decreases fibrinogen significantly. Inhibition of intrinsic coagulation pathway and the activation of fibrinolysis via an increase of t-PA activity
- No information on Histamine or Mast Cell impact
Grape Seed Extract
Grape seed extract is rich in proanthocyanidins. Proanthocyanidins are available from other supplements (cranberry juice, cider). There are contradictory reports on whether it increases or decreases IL6, IL8, TNF. It may or may not offer protection for glutamate excitotoxicity (depends on grapes being used)
- Decrease in uPA and PAI-1 activities and thus decreased fibrinolytic activity
- Decreased fibrinolytic activity, decreased cell-surface plasmin activity
- Decreases fatigue when taken with L-arginine
- Decreases COX2
- Decreases fatigue
- Decreases IL-17, IL-6
- Decreases IL-1-beta,TNF, IL-6 and IL-8
- Decreases platelet activation
- Decreases thrombus formation, inhibitory effect on platelets
- Increases anti-thrombin activity
- Increases TNF
- No information on Histamine or Mast Cell impact.
- Because it is asalicylate (like aspirin and bromelain) probably best to avoid
Check also CoreMine (Link searches for FADS2):
http://www.coremine.com/medical/#search?ids=49995&tt=8191&org=hs&i=49995
I took a break to see if this was stressing me more
im getting fed up with these symptoms and no answers and treatments causing issues or making them worse
i have had lab work
ana was speckled in 2010 since the. It's been normal nevative
was told thyroiditis and tsh 6 in 2012 levothyroxine made me go from 150-119 pounds and tsh of 0.4
now I'm told
tsh Normal and I don't have thyroid issue
yet I'm off the med for years
having another ultrasound done
told it's not sjorgens or lupus
despite dry eyes chronic even with plugs restasis and xxidra
gel before bed
humisifer water fish oil flax supplement
avoid dairy gluten wheat soy since november
all that's doing is causing an eating disorder as I'm scared to get acne
it has not fixed my skin issues at all
i have hives from heat and urticaria water hives and dermatapgropishim can't treat because antihistamines dry u
my skin eyes nose scalo dry
mouth only when waking or anxious
i have anxiety depression OCD anger insomnia all I can't treat becauS they all aggravate symptoms
erectile was worse when I was on ssri
errctions aren't what they were but I can get them depending on if I slept 5 hours or so and have a freak
thats another story
my t levels were 900 high year ago
now they are 500
maybw diet?
my regular t was 12.9 range was 10-50
seems low to me
ny sodium 137 range 135-150
again barely normal
was told iodine zinc magnesium low
so I take supplements
notice no difference
what can I do
i feel trapped
im having flushing coming back due to anxiety
meds helped but the cold hands feet and dry eyes sleep issues get worse
I barely have body hair I'm 28
my body is dehydrated feeling
hot flashes
acne rash rosacea like face
dark bags under eyes
sleep issues
cold feet and hands
eyebrow lashes fall out easy
mental issues worse than before tane
my back pain went away from this drug and constipation
those were two symptoms diet got rid of
I'm waiting for an MRI on pituatry
because my LH hormone was high and now it's normal
but doctor said could mean low t
rhibks my pineal gland was damaged could cause sleep issues
was told sleep apnea
but I have small adnoids
i was 150 5'10
said didn't fit criteria
also machine dries out nasal passages
I'm so sick of not being able to treat these issues
id kill for 6 solid hours of sleep
and to not wake up with my eyes crusty mucus conjunctivitis
this is 10 years post tane
two coursez
had to stop course 2
mid way
because of liver enzymes cholesterol and triglycerides were high
same time this is when all this happened
forgot to mention ultra sound years ago showed fatty liver
told now it's congested and leaky Gut and diet will fix it
but it's been almost a year on diet
if anything I get more acne now
def not as bad before tane
although I only had mild acne not cystic
so fed up
apologixe for errors phone broke
On 5/28/2017 at 9:13 AM, mariovitali said:@Dubya_BI really tried but couldn't go through this and spend too much time (DAVID didn't seem to be working) . Could we set up a Skype call ?
PM me when you can. Thanks!
I have also used Malacards, here is an example for FADS2
DAVID is currently working but a pain in the ass to use and quite a bit antiquated.
PANTHER is easy to use and is maintained by the Gene Ontology Consortium (GO)
If you have another few minutes, paste the gene list into the text box on the homepage, select Homo sapiens, then select the analysis you want to run:
Checked out MALACARDS and COREMINE. Will add these to my little online tool collection. Thanks.
I haven't noticed an option in PANTHER to search such disease association databases as you linked. KOBAS does this.
...A Skype call some time in the next couple weeks sounds good. Will PM you with times that work for me. I can set aside time on a weekend if needed. Just keep in mind, I only learned the basics of using and interpreting bioinformatics tools in the past few months. No expertise here.
About a couple of your previous comments:
Getting ANY researcher to look at something a random layman is presenting was described to me as a Herculean task. I asked around about who I should contact to plant the seed for a pharmacogenetic study of Accutane and was told by two PHDs to just do that as my thesis. I don't have the ten years it would probably take to earn a living and go that far. Probably waving money or some asinine award in the face of a university researcher would work since they are often concerned with status and good will won't buy status. Best case scenario might be to have your idea stolen if it is solid. Really good to hear that the PFSF at least is considering communicating with you further.
The other point you brought up was whether we have an official organization. We don't. There was RoAccutane Action Group in the UK years ago, but their founder was supposedly issued a gag order as a stipulation in a large settlement with Roche over the death of his son. The chairman of RoAccutane Action Group went silent sometime in the 2000s and committed suicide in late 2014. The whole of our organization is what you see here, a small parents group in the UK, and victims (mostly teenagers and young adults) scattered across the internet with little communication.
We may be in luck!
People over at Phoenix Rising start making the connection between Post-Finasteride Syndrome and Post-Accutane Syndrome and a nice lady saying to me that she can connect me with Ron Davis at Stanford!
Check out my new blog post regarding Liver Disease and a patent that uses Vitamin K for mitochondrial disease. This is very interesting i believe.
let me know what you think Guys.
On 2017-5-18 at 4:21 PM, Recreant said:Hi,
Wanted to sign up for this site to post about my accutane experience. I wrote a big long thing about it and came to register but then realized I already had an account that I'd totally forgot about and apparently posted a somewhat similar account of my drug experience 5 years ago. Damnit! Well, new things have cropped up in the past five years and I spent a while on this and want to post it anyway. I'd be very thankful if anyone actually reads through it and has any advice. Thanks.
As an 18 year old in the year 2000 who suffered from moderate acne I was excited about getting on the drug and finally ending my horrible acne affliction. Things were fine at the beginning but I soon lowered my dose on my own because the skin and lip dryness was insane. I think my doctor had prescribed something along the lines of alternating between 80mg and 40mg each day. I think I ended up taking 40mg every other day to give myself some breathing room from the drug. I still wonder what would have happened if I'd stuck to the original dosage my doctor had prescribed. I'd probably be worse off. I think he's dead now.
I was about a month or so into my course when my heart sank at the sight of some hairloss at the corners of my hairline. That's also when I first noticed a thick, whiteish sludge of sebum on my scalp that I'd never had before. As my hairline receded, something else happened: all the hair on my head began to slowly miniaturize. I used to have very, very thick hair but now it was see-through. My head looked like a mountain in winter, when all the leaves have fallen off the trees and you can see right through to the ground. This drove me kinda nuts and I angrily shaved my head bald. That's when I realized the extent of the sebum on my scalp - it was insane. I would drag my nails across my scalp every day and scrape up huge amounts of the stuff.
Shaving my head may have not been the best idea though, because it triggered one more horrible situation: folliculitis. Not only was my hair now see-through, but I was starting to develop a severe case of folliculitis that was now easily visible! Hats became my friend and unfortunately have been my friend for 17 years. I'm the weird hat guy at all the parties.
Anyway, the folliculitis got really bad and I stupidly agreed with my derm to go on minocycline. I didn't last long on the antibiotic because it gave me horrible dry eyes. Any winter wind would make me look like I was crying. While I kind of hate having dry eyes and still have them, they weren't my worst side and I only saw one optometrist about it a very long time ago. I vaguely remember him claiming I had oily eyes or something. I don't know. After quitting cold turkey the folliculitis came back worse, obviously. The answer? Stupidly agree to go on Doxycycline. Doxycycline took two weeks to give me permanent eye floaters so I dropped it cold turkey too. I still remember the day after quitting. It was about 4 in the afternoon when I could feel the first hints of the folliculitis storm coming. I actually felt feverish. The folliculitis hit me the hardest it ever has and my scalp basically turned into one giant scab. I couldn't sleep it hurt so bad. I'm pretty sure my derm is dead.
My derm then prescribed me topical clindamycin to attack it. I basically soaked my scalp in the stuff, so of course it got into my system. It didn't take too long before it gave me jaundice and I stopped. I then went on Tetracycline which I'd taken previous to Accutane but it eventually gave me jaundice, too. I resorted to giving up on antibiotics and after a while the folliculitis did calm slightly. I was also using a shampoo called Sebulex which really helped. Of course it's now discontinued because life is unfair. He's definitely dead because he was super old and this was all 17 years ago.
Anyway, I finally ended up doing a ton of research in 2006 and began to realize intestinal permeability and food allergies were the culprit behind my aggressive folliculitis. By cutting out dairy, excess sugar, and wheat, while taking supplements like L-Glutamine, I was able to really keep my scalp clear. Unfortunately I had to stop the L-Glutamine after I upped my dose one night and woke up the next morning with Multiple Sclerosis type symptoms. Terrible balance, speech stuttering and involuntary muscle spasms that lasted a year. So... I may have MS since L-Glutamine is something that would be very bad for someone with MS to take.
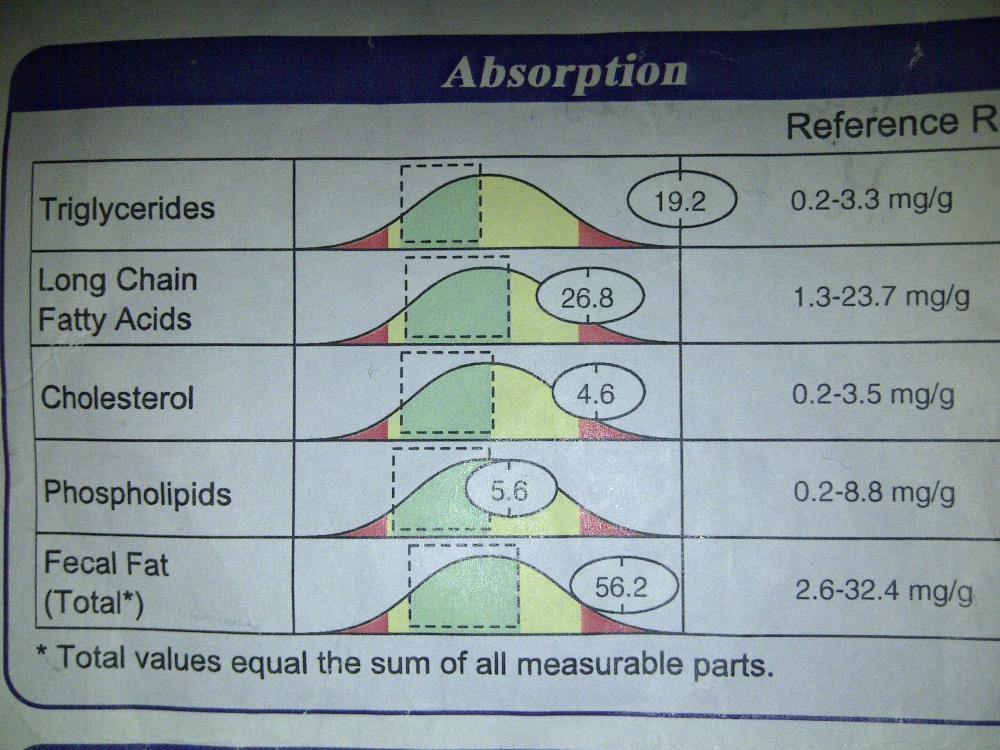
In 2007 I took a stool analysis test that showed bizarre fat malabsorption. The presence of fat in my stool was highly elevated and my triglycerides were literally off the chart.
Despite the knowledge of malabsorption I didn't really do anything about it. I kind of got wrapped up in work and since I'd healed my gut a little I kind of forgot about it all - though I still had the dry eyes, floaters, and hairloss. My sebulex shampoo was working quite well controlling the crazy dandruff I now had. Although I did have, and still do, an annoying amount of seborrheic dematitis around my nose and in my beard area.
Fast forward to the past couple of years where I started experiencing GERD and IBS. My stomach would make the most insane gurgling sounds when I'd drink a can of coke. My stool changed. It started to become looser and looser until one day I saw a bit of blood and freaked out a little. Despite my concern I really procrastined in getting it checked out. I'd also moved to a new province (I'm in Canada) and didn't have a health card so it took a long time to see a doctor and by then my stool was mostly blood and mucus. I had to start wearing extra pairs of underwear to bed in case of accidents. 😡I got a colonoscopy done last month and was diagnosed with Colitis. Doctors aren't sure if it's Ulcerative Colitis or Crohn's. I was prescribed Mesalamine but stopped due to fear of side effects. I'm prone to permanent sides and at this point rarely risk adding to my collection. I've managed to normalize my bowel movements relatively well without the drug via diet and supplements. No more blood and my bowel movements are sort of formed. Just not quite what they used to be. Although I still often get stool that is pale and floats on the surface.
This whole colon thing was a real nuisance, but something else has cropped up in the past month: acne.
I mean, I still had some acne over the years since Accutane but it was never that hard to control. But something happened about a month and a half ago that made it much worse. I don't really get regular pimples but mostly whiteheads around my nose and at the edges of my lips. I'll wake up with 8 new tiny whiteheads each morning. I also recently had an instance of deep cystic acne all around my chin and jawline. The only thing I can think of that happened a month and a half ago is I very stupidly drank vodka like 5 days in a row. I've never done that before and it's a long story. Actually the past couple years where my bowels have gone down hill correlate with when I started drinking more. Most of the past 17 years I drank about 3 times a year but in the past 2 years or so I started drinking at least once a week. Hmmm.
So now I'm wondering if my recent drinking impaired my liver more than it already was. While on accutane I never got my liver enzymes tested. Then there's all that jaundice I got and the fat malabsorption. Feels like my bile isn't flowing.
Also, in the past week I've been closely monitoring my skin and how it reacts to what I eat and I've noticed a clear correlation with eating fruit and the acne, particularly apples. Then I read about fructose malabsorption and FODMAPS. I realized on those nights I ate apple for dessert I had a tendency to eat a bunch of onion rings with my dinner - a big nono for the FODMAPS diet. These symptoms seem to also point to a liver problem.
Anyway, if anyone has similar symptoms and has found something that helps them I'd be glad to hear about it.Oh and something else interesting: the craziest affect a supplement has ever had on me was Betaine HCL. People love the stuff but I tried it and my folliculitis went nuts. Basically turned me into a scab again. It was super dramatic. My only theories have been it either killed off bacteria growing in my stomach / small intestine and it was "die off" I was experiencing (although why don't antibiotics cause die off?) or my stomach acid has been burning my duodenum due to a lack of bile to neutralize it. And by increasing my stomach acidity I burned myself worse than usual. I especially know my folliculitis is tied to intestinal mucosal wall integrity because it's on a permanent cycle where it gets worse and better like clockwork that seems to match the cycle of intestinal wall replacement that happens every 4 days or so.
Hey man, have you thought about pro-biotics? They might hurt in the short run, but in the long term might be a big help. Some people they are life-savers, but others (like me)don't notice much of a difference. For me it stopped a bit of constipation I was getting ![]()
You won't know until you try, or if you have let us know how it went ![]()
Taurine can stimulate bile production, and some people think it helps with eyes as well. went on it for serveral months and I think it helped a bit. Taurine also helps regulate retinoic acids, personally I think its a very good drug to help with the immediate accutane, as many people post accutane are deficient.
Good luck, I've made another thread on this forum to what I think causes accutanes side effects and what can be done from that angle, but this is just stuff that I feel might help you specifcally ![]()
Wanted to ask you, have you ever performed a Fibroscan? This test looks at possible Liver fibrosis. To the best of my knowledge, the gold standard for assessing Liver Disease is Liver biopsy then the test i mentioned.
Has anyone else had Liver Biopsy / Fibroscan by any chance?
8 hours ago, mariovitali said:@guitarman01Wanted to ask you, have you ever performed a Fibroscan? This test looks at possible Liver fibrosis. To the best of my knowledge, the gold standard for assessing Liver Disease is Liver biopsy then the test i mentioned.
Has anyone else had Liver Biopsy / Fibroscan by any chance?
Fibroscan isn't available in the United states . I just had a pretty extensive liver panel. Ive also had a full hepatitis panel, which by definition is inflammation of the liver. I think they only start to look into fibrosis if positive for hepatitis c? You can also look at other markers of liver inflammation (that appear to be normal in my case) or serum markers they call a fibro score. Looking at these test results, there doesn't appear to be any reason to check serum bile.
Here is my liver panel.
Protein, Total, Serum 7.7 g/dL 6.0 - 8.5
Albumin, Serum 4.9 g/dL 3.5 - 5.5
Bilirubin, Total 0.4 mg/dL 0.0 - 1.2
Bilirubin, Direct 0.11 mg/dL 0.00 - 0.40
Alkaline Phosphatase, S 53 IU/L 39 - 117
LDH 157 IU/L 121 - 224
AST (SGOT) 15 IU/L 0 - 40
ALT (SGPT) 10 IU/L 0 - 44
GGT 12 IU/L 0 - 65
Cholesterol, Total 183 mg/dL 100 - 199
actually, looking at cholesterol levels reminded me to dig into my records to check this.
See how your cholesterol numbers compare to the table below:
Total Cholesterol Level | Category |
|---|---|
| Less than 200mg/dL | Desirable |
| 200-239 mg/dL | Borderline high |
| 240mg/dL and above | High |
LDL (Bad) Cholesterol Level | LDL Cholesterol Category |
| Less than 100mg/dL | Optimal |
| 100-129mg/dL | Near optimal/above optimal |
| 130-159 mg/dL | Borderline high |
| 160-189 mg/dL | High |
| 190 mg/dL and above | Very High |
HDL (Good) Cholesterol Level | HDL Cholesterol Category |
| Less than 40 mg/dL | A major risk factor for heart disease |
| 4059 mg/dL | The higher, the better |
| 60 mg/dL and higher | Considered protective against heart disease |
and thats funny, out of all my tests, ive never had a full lipid panel. I'll be getting this tomorrow.
Hey @guitarman01 did you ever get results back from that antibodies test or not yet?
19 minutes ago, Colinboko said:Hey @guitarman01 did you ever get results back from that antibodies test or not yet?
I do have some antiphospholipid antibodies. it's considered equivocal or nonspecific. I'll have more info by tomorrow probably.
Equivocal meansjust that you aren't positive but you aren't really negative either.
nonspecific. Story of my life.
31 minutes ago, guitarman01 said:I do have some antiphospholipid antibodies. it's considered equivocal or nonspecific. I'll have more info by tomorrow probably.Equivocal meansjust that you aren't positive but you aren't really negative either.
nonspecific. Story of my life.
I just don't understand how LITERALLY NOTHING shows up on our test results. Like what the fuck...
Then again chronic fatigue doesn't either I guess..
 Acne.org Products
Acne.org Products