No, You Should Never Attempt to Pop Cystic Acne Lesions

The Essential Info
Cystic acne lesions include nodules and cysts, which are large, painful lesions more than 5 millimeters in diameter. Although it is OK to pop less severe types of acne, like pustules (run-of-the-mill “zits” with a white or yellow center), nodules and cysts should never be popped.
Nodules: Nodules are the most common type of cystic acne lesion. They are fibrous lesions with no pus, so there is nothing to “pop.” If you do attempt to pop a nodule, it will only result in more inflammation, skin damage, and more extensive scarring.
Cysts: Cysts are much less common than nodules, but do contain pus. However, they are not “poppable.” If an attempt is made to pop a cyst, it will likely cause the pus to be expelled deeper into the skin, instead of onto the surface, and this will result in more inflammation, skin damage, and scarring.
Instead of squeezing cystic acne lesions, it is better to see a dermatologist for a quick cortisone shot directly into the lesion. This will quickly reduce inflammation and help prevent scarring. Your doctor may also opt to apply extreme cold to the lesion (cryotherapy), which can also help it heal. For stubborn cysts in particular, your doctor may need to cut into it and drain it, but never try this at home.
A proper benzoyl peroxide regimen can prevent most cystic acne from developing. However, for severe, widespread, and scarring acne, isotretinoin (Accutane®), is sometimes prescribed, and can be combined with oral steroids.

The Science
Cystic acne, also called nodulocystic acne, consists of large, severe lesions called nodules and/or cysts. This type of acne should never be popped because it can damage the skin and make the acne lesion worse.
If performed correctly, other, less severe acne lesions can be popped, but popping nodulocystic acne results in more redness, swelling, pain, and scarring.
- Nodules: Nodules are large (over 5mm in diameter), red, hard, painful lesions that form deep within the skin and can remain there for weeks, months, or even years. They are by far the most common nodulocystic acne lesion. Nodules do not contain pus and cannot be popped, no matter how skillful the attempt. There is simply nothing to “pop.” If an attempt is made to pop a nodule, the surrounding skin will become even more red and swollen. The larger and more swollen a nodule becomes, the greater the chance it will leave a scar on the skin.
- Cysts: Cysts are large (over 5mm, but can be up to 7 – 15mm in diameter), red, painful lesions that form deep within the skin and, as with nodules, can remain there for months or even years. Unlike nodules, cysts do contain pus, and can sometimes leak onto the surface of the skin. However, the pus is deep under the skin, and if an attempt is made to pop a cyst, it will most likely push the pus deeper into the skin instead of onto the surface. If the pus is pushed farther into the skin, it can result in more skin damage, infection, and scarring.
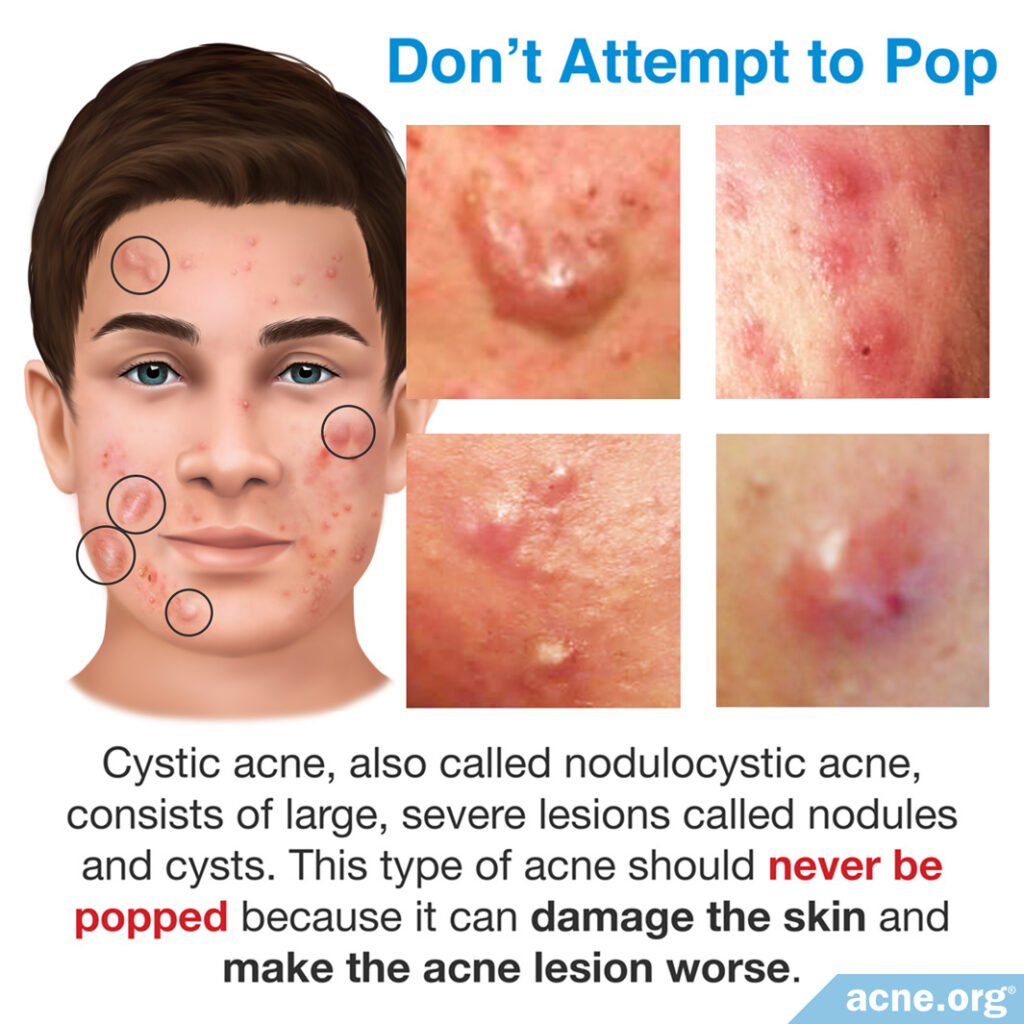
Overall, cystic acne should never be popped because:
- When you try to “force” a lesion to pop, this can wound the skin further.
- When you prick or cut the surface of the skin, you can increase the risk of infection.
- Unsuccessfully popping a severe lesion can increase the risk of scarring.1 – 3
Alternatives to Popping Cystic Acne

There are several nodulocystic acne treatment options that can help clear it without permanently damaging the skin.
Prescription Medications
Prescription medication options for nodulocystic acne include:
- Accutane® (isotretinoin) is the most aggressive treatment option for people with widespread and severe nodules and cysts, but comes with severe side effects, including birth defects, and works by permanently changing the body. It is a serious decision that must be considered carefully alongside a trusted physician.
- Oral steroids can be prescribed to nodulocystic acne patients for the first 2 – 4 weeks to reduce inflammation quickly before beginning isotretinoin treatment.
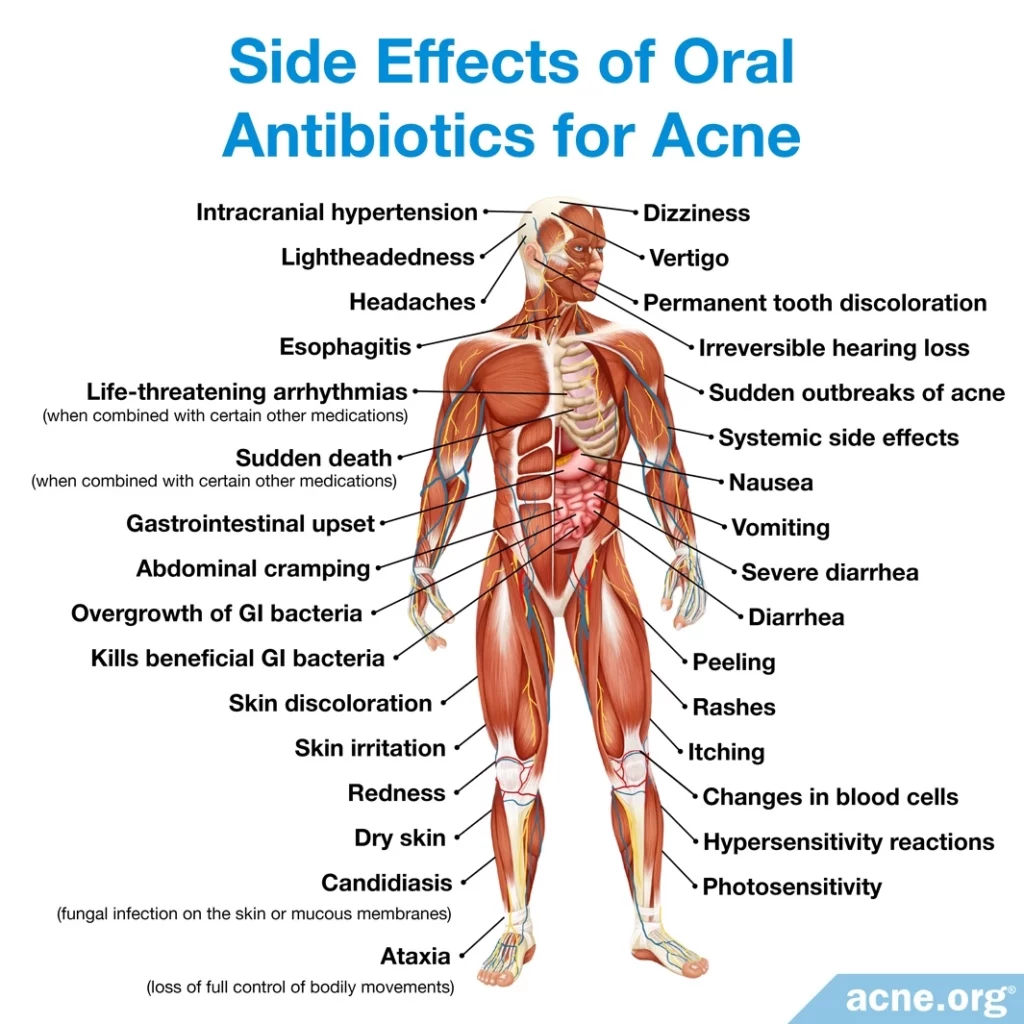
- Oral antibiotics are a less effective treatment option for people with nodulocystic acne, but may be somewhat effective for such patients with only a few nodules or cysts. Oral antibiotics are only a short-term treatment approach, as they can only be used for 3 – 6 months. Unfortunately, nodulocystic acne may redevelop after the antibiotic usage is stopped. Oral antibiotics cannot be taken with isotretinoin because this combined therapy may cause a buildup of pressure inside the skull, which can be damaging.4,5
Intralesional Steroid Shots (Cortisone Shots)
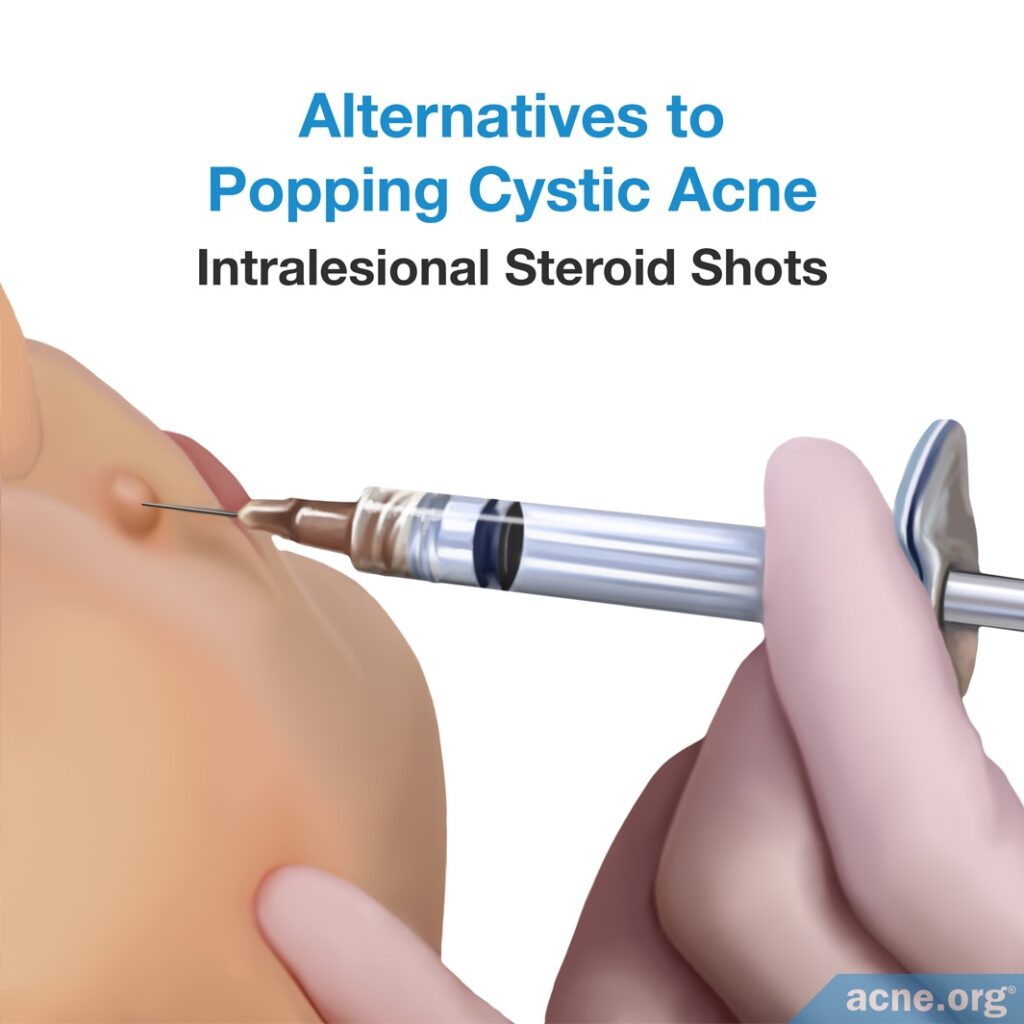
For a single nodule or cyst, an injection of steroids, such as cortisone, directly into the lesion can almost immediately reduce inflammation and begin healing. These shots, although not the best option for widespread nodulocystic acne, are effective at clearing one lesion or a small number of acne lesions. Further, intralesional steroid shots can reduce the risk of developing acne scars.
Incision and Drainage
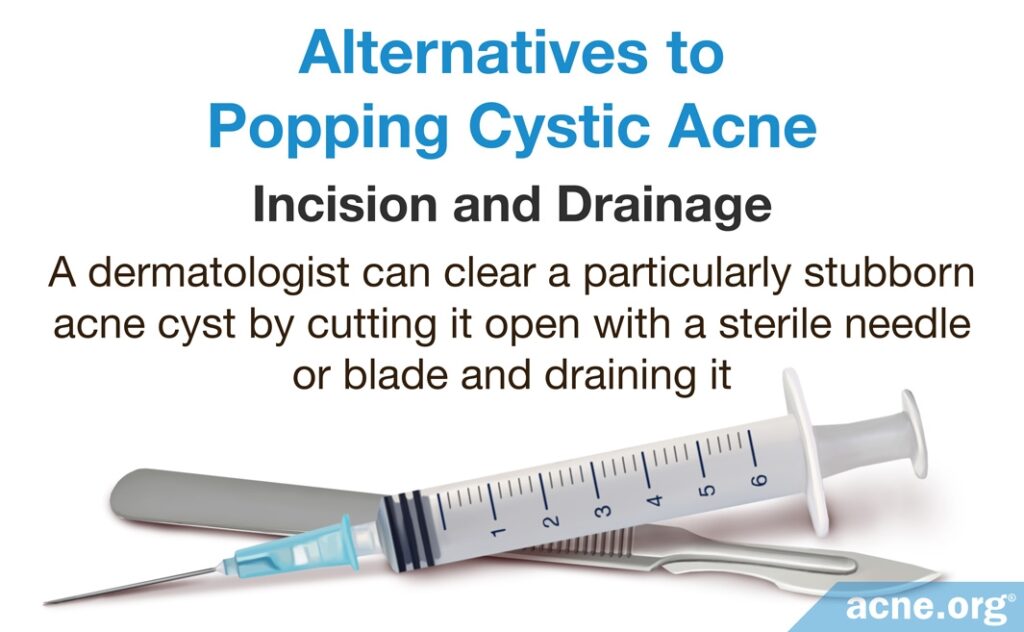
A dermatologist can clear a particularly stubborn acne cyst by cutting it open with a sterile needle or blade and draining it. This procedure cannot be used to clear acne nodules because they do not contain pus. Draining a cyst like this should never be attempted at home.3
Cryotherapy
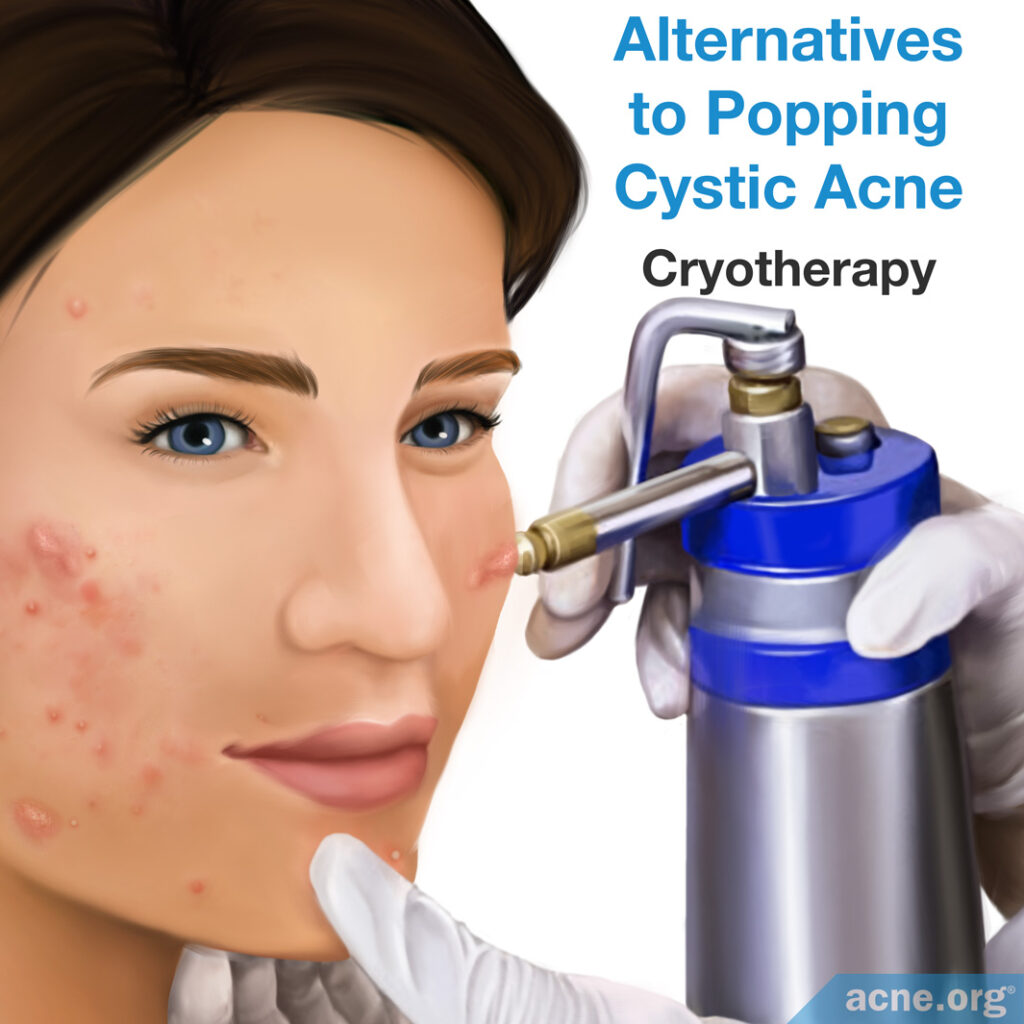
Cryotherapy is a procedure performed by quickly freezing the nodule or cyst without applying pressure.
A 1974 study published in the British Journal of Dermatology investigated the effectiveness of cryotherapy on 25 acne patients with acne conglobata, which is a rare, especially severe form of nodulocystic acne. They found that cryotherapy resulted in clearance of most nodules within 10 days post-treatment. Further, in the treated areas, nodules did not reappear for up to 28 months after treatment.
However, this technique does nothing to prevent future nodules or cysts, so while it may be helpful, it must be combined with other therapies to prevent future acne lesions from developing.
The doctors did not attempt this treatment on cysts, so we do not know whether it would also work on them.6
Photodynamic Therapy

One less common treatment for nodulocystic acne is photodynamic therapy. This therapy is performed by treating the skin with a sensitizing agent and then illuminating the skin with (usually red) light. There is little research on the effectiveness of this treatment, so until scientists perform more studies, photodynamic therapy should not be used as a primary treatment for nodulocystic acne.
The Bottom Line
Never attempt to pop a cystic acne lesion. Instead, make an appointment with your dermatologist for a procedure that can help immediately heal any nodules and/or cysts that you have.
To prevent future nodules and cysts, a properly applied topical regimen should keep them at bay. For especially severe and widespread nodulocystic acne, you may want to have a conversation with your doctor about Accutane (isotretinoin), but be aware that it comes with potentially lifelong side effects.
References
- Zaidi, Z. Dispelling the Myths and Misconceptions of Acne. J. Pakistan Med. Assoc. 59, 264 – 265 (2009). https://jpma.org.pk/article-details/1684
- Hassan, K. & Eltayb, N. Eucalyptus Oil as A Treatment for Acne. Pharmanest 4, 557 – 566 (2013). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3703330/
- Pimple popping: Why only a dermatologist should do it. American Academy of Dermatology (2017) https://www.aad.org/public/diseases/acne-and-rosacea/pimple-popping-why-only-a-dermatologist-should-do-it
- Schwartz, R. Acne Conglobata treatment & management: medical care, surgical care, consultations (2016) https://emedicine.medscape.com/article/1072716-treatment
- Habif, T. P. Clinical Dermatology: A Color Guide to Diagnosis and Therapy (2016). https://www.elsevier.com/books/clinical-dermatology/habif/978-0-323-26183-8
- Leyden, J., Mills, O. & Kligman, A. Cryoprobe treatment of acne conglobata. Brit. J. Dermatol. 90, 335 – 341 (1974). https://www.ncbi.nlm.nih.gov/pubmed/4274644
