Information and Treatment for Acne on the Back of the Neck

The Essential Info
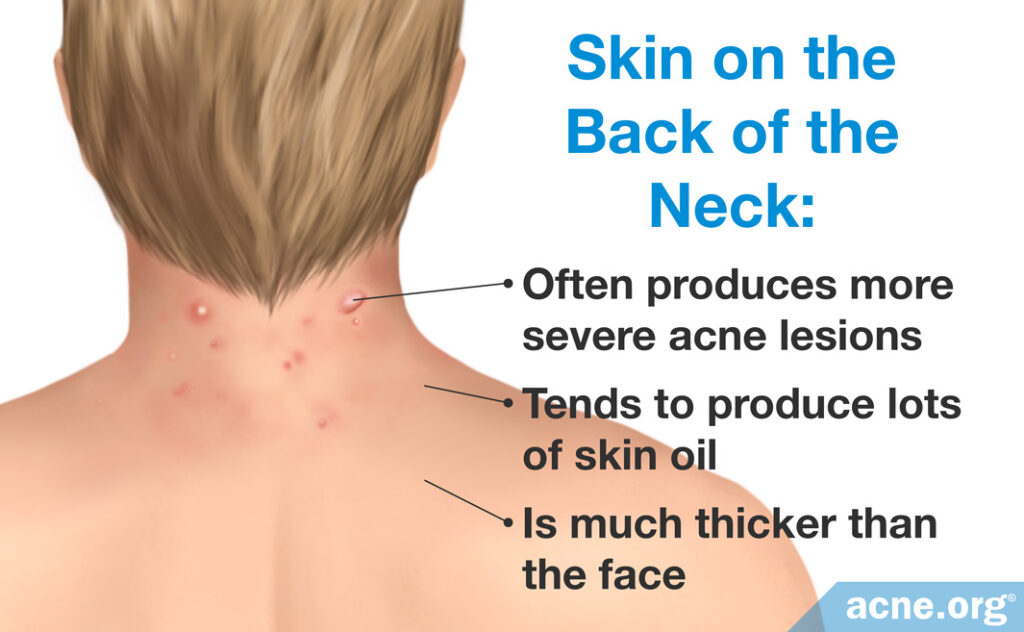
The skin on the back of the neck is thick, with bigger pores and larger skin oil glands compared to the skin on the face and front of the neck. This makes the skin on the back of the neck more likely to produce more severe acne lesions. For purposes of this article, acne on the back of the neck is what we refer to when we say “neck acne.”
More Severe in Males: Neck acne affects both males and females, but may be more severe in males.
Physical Irritation Can Make It Worse: Like body acne, physically irritating the skin can aggravate neck acne, so steps should be taken when possible to avoid irritating the skin of the neck, such as limiting stiff collars and ties when possible.
Treatment: Treatment for neck acne is similar to treatment for body acne since the skin on the back of the neck is similar to the skin on the back and chest.
Acne on the Front of the Neck: Important! Don’t treat the skin on the front of the neck the same way that you treat the skin on the back of the neck. The skin on the front of the neck is much thinner and far more sensitive than it is on the back of the neck. If you have acne on the front of your neck, treat it the same way that you treat facial acne, starting very slowly and ramping up your dosage of medication over time.

The Science
Acne on the back of the neck is more similar to body acne than it is to facial acne and presents unique challenges. Neck acne lesions can be painful and can have an abrupt onset and long lifespan.
The skin on the back of the neck is much thicker than the face and can produce lots of skin oil. Because of this, the skin on the back of the neck can often produce more severe lesions such as cysts and nodules.
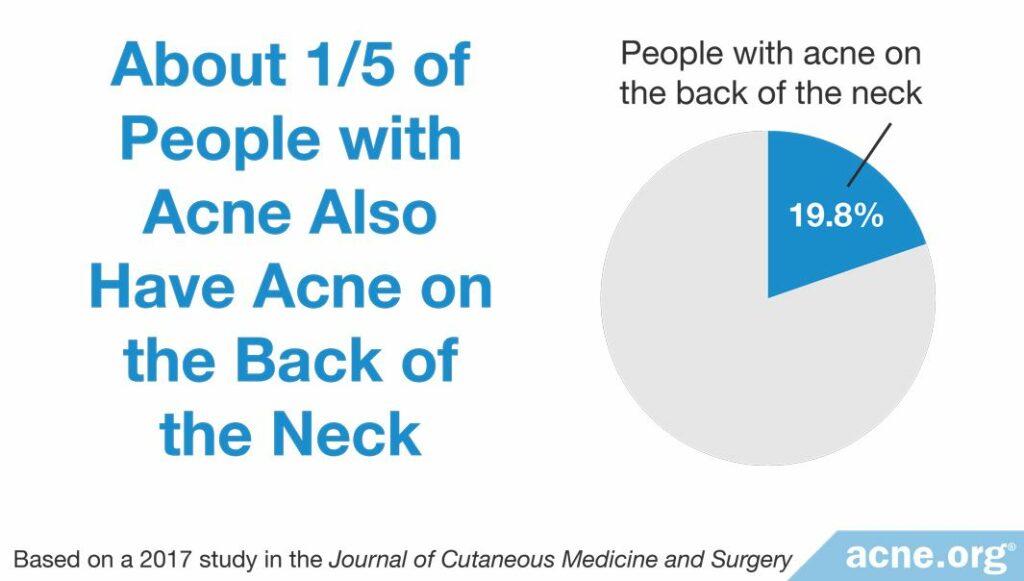
Neck acne is common and afflicts both males and females, but males may experience more severe neck acne, as noted in a study published in the Journal of Cutaneous Medicine and Surgery in 2017:

The researchers examined 79 male and female volunteers between the ages of 13 and 52. They found that approximately half of the volunteers had acne somewhere on the body. Of the people with acne, 19.8% or about one-fifth had acne on the back of the neck. The researchers noted that most cases of neck acne were mild, but “males presented with a higher severity than females.”1
Neck acne is caused by the same mechanisms that cause facial and body acne.2-18 Pores become clogged due to a build-up of cells which stick together and cause a plug. Then bacteria and skin oil, which would normally drain to the surface, get caught inside, causing redness and pus to develop.
Avoiding Irritation
Physical irritation can aggravate neck acne. For instance, stiff collars can rub the skin and make neck acne worse. This often creates a vicious cycle. Neck acne develops, and the sufferer will wear collared shirts to cover it. The collared shirts then cause irritation and aggravate acne, and so on. Here are a few tips to make sure you don’t get caught in this cycle:
- Try wearing crew neck shirts or shirts without collars.
- If you must wear collared shirts, as most of us must from time to time, try wearing soft cotton shirts which will be less harsh when rubbing against the skin.
- Do not pick or fiddle with your neck. Leave it as untouched as possible.
- Try to stay aware of anything that might irritate the back of your neck and take action to stop the irritation if possible.
A Special Case – AKN: Sometimes males develop a special form of acne on the back of the neck called acne keloidalis nuchae, or AKN for short. AKN is most common in African-American males and can lead to the formation of keloid (raised) scars. This type of acne occurs due to repeated physical irritation of the neck, often due to shaving the back of the neck, getting a very short haircut, and/or using greasy hair products that come in contact with the back of the neck.19 If you think you may have AKN, consider doing the following:
- Ask your barber to be super gentle and not go over any area more than once if possible.
- Ask your barber not to shave the hair closer than ¼ inch.
- Treat the area with benzoyl peroxide followed by glycolic acid. You can view a treatment regimen for the back of the neck here.
Treating Neck Acne
Treatment for neck acne is similar to treatment for body acne.20-24
The Neck Regimen: The most effective topical treatment is The Neck Regimen, which uses the combination of 2.5% benzoyl peroxide and 10% glycolic acid. This powerful combination can clear up even tough to treat cases of neck acne. However, the process of The Neck Regimen is just as important as the products. It must be followed precisely to be effective.
Accutane (isotretinoin): For severe, widespread, and potentially scarring acne, Accutane (isotretinoin) is an option. Isotretinoin is a systemic oral treatment which is taken for 15-20 weeks and produces long-term remission of acne symptoms in about 2/3 of people, but comes with a large range of side effects including causing severe birth defects, and must be administered in close partnership with your physician.23-24
Acne on the Front of the Neck

The skin of the front of the neck is much thinner and far more sensitive than the skin on the back of the neck and should be treated similarly to facial acne. Trust me, don’t start an aggressive treatment regimen on the front of the neck! Take it slow.
References
- Desai, K., Frey, M. P. & Tan, J. The utility of assessing neck acne. J. Cutan. Med. Surg. 21, 82-83 (2017). https://www.ncbi.nlm.nih.gov/pubmed/27698089
- Titus, S. & Hodge J. Diagnosis and treatment of acne. Am. Fam. Physician 86, 734-740 (2012). https://www.ncbi.nlm.nih.gov/pubmed/23062156
- Bataille, V., Lens, M. & Spector, T. D. The use of the twin model to investigate the genetics and epigenetics of skin diseases with genomic, transcriptomic and methylation data. J. Eur. Acad. Dermatol. Venereol. 26 1067-1073 (2012). https://www.ncbi.nlm.nih.gov/pubmed/22243446
- Kligman, A. M. & Plewig, G. Acne and Rosacea, (Springer, Berlin, 2000). https://www.springer.com/gp/book/9783642640964
- Chen, W. C. & Zouboulis, C. C. Hormones and the pilosebaceous unit. Dermatoendocrinol. 1, 81-86 (2009). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2835896/
- Thiboutot, T., Gilliland K, Light, J. & Lookingbill, D. Androgen Metabolism in Sebaceous Glands from Subjects With and Without Acne. Arch. Dermatol. 135, 1041-1045 (1999). https://www.ncbi.nlm.nih.gov/pubmed/10490108
- Dessinioti, C. & Katsambas, A. D. The role of Propionibacterium acnes in acne pathogenesis: facts and controversies.
Clin. Dermatol. 28, 2-7 (2010). https://www.ncbi.nlm.nih.gov/pubmed/20082942 - Zouboulis, C. C. Propionibacterium acnes and sebaceous lipogenesis: A love-hate relationship? J. Invest. Dermatol. 129, 2093-2096 (2009). https://www.ncbi.nlm.nih.gov/pubmed/19809423
- Pappas, A., Johnsen, S., Liu, J. C. & Eisinger, M. Sebum analysis of individuals with and without acne. Dermatoendocrinol. 1, 157-161 (2009). https://www.ncbi.nlm.nih.gov/pubmed/20436883
- Tidman, M. J. Prompt treatment of acne improves quality of life. Practitioner 256 15-7, 2 (2012). https://www.ncbi.nlm.nih.gov/pubmed/22916580
- Kurtalić, N. et al. Quality-of-life of adolescents with acne vulgaris. Acta Med. Croatica 64, 247-51 (2010). https://www.ncbi.nlm.nih.gov/pubmed/21688607
- Alexis, A. F. & Lamb, A. Concomitant therapy for acne in patients with skin of color: A case-based approach. Dermatol. Nurs. 21, 33-36 (2009). https://www.ncbi.nlm.nih.gov/pubmed/19283960
- Shah, S. K. & Alexis, A. F. Acne in skin of color: Practical approaches to treatment. J. Dermatolog. Treat. 21, 206-211 (2010). https://www.ncbi.nlm.nih.gov/pubmed/20132053
- Taylor, S. C., Cook-Bolden, F., Rahman, Z. & Strachan, D. Acne Vulgaris in Skin of Color. J. Am. Acad. Dermatol. 46, S98-S106 (2002). https://www.ncbi.nlm.nih.gov/pubmed/11807471
- Halder, R. M. & Nootheti, P. K. Ethnic Skin Disorders Overview. J. Am. Acad. Dermatol. 48, 143-148 (2003). https://www.ncbi.nlm.nih.gov/pubmed/12789168
- Davis, E. C. & Callender, V. D. A review of acne in ethnic skin: Pathogenesis, clinical manifestations, and management strategies. J. Clin. Aesthet. Dermatol. 3, 24-38 (2010). https://www.ncbi.nlm.nih.gov/pubmed/20725545
- Cunliffe, W. J., Goulden, V. & Stables, G. I. Prevalence of Facial Acne in Adults. J. Am. Acad. Dermatol. 41,577-80 (1999). https://www.ncbi.nlm.nih.gov/pubmed/10495379
- Knaggs, H. E. et al. Post-adolescent acne. Int. J. Cosmet. Sci. 26, 129-38 (2004). https://www.ncbi.nlm.nih.gov/pubmed/18494869/
- Al Aboud, D. M. & Badri, T. Acne keloidalis nuchae. [Updated 2020 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459135/
- Rademaker, M. Isotretinoin: dose, duration and relapse. What does 30 years of usage tell us? Australas. J. Dermatol. 54, 157-162 (2013). https://www.ncbi.nlm.nih.gov/pubmed/23013115
- Mohd, N. H. & Aziz, Z. A systematic review of benzoyl peroxide for acne vulgaris. J. Dermatolog. Treat. 24, 377-386 (2013). https://www.ncbi.nlm.nih.gov/pubmed/22658322
- Savage, L. & Layton, A. Treating Acne Vulgaris: Systemic, Local and Combination Therapy: Benzoyl Peroxide. Expert Rev. Clin. Pharmacol. 13, 563-580 (2010). https://www.ncbi.nlm.nih.gov/pubmed/22111684
- Ganceviciene, R. & Zouboulis, C. C. Isotretinoin: State of the art treatment for acne vulgaris. J. Dtsch. Dermatol. Ges. 8, S47-S59 (2009). https://www.ncbi.nlm.nih.gov/pubmed/20482692
- Rademaker, M. Adverse effects of isotretinoin: A retrospective review of 1743 patients started on isotretinoin. Australas. J. Dermatol. 51, 248-253 (2010). https://www.ncbi.nlm.nih.gov/pubmed/21198520
