A Common Genetic Condition that Normally Goes Away on Its Own

The Essential Info
Keratosis pilaris is a very common genetic skin condition that affects people of all ethnicities.
It presents as tiny, hard bumps, closely resembling goosebumps or chicken skin, typically on the back of the upper arms and/or the front of the thighs.
It is usually harmless and does not require medical attention. The bumps usually clear on their own over time.
Skin with keratosis pilaris is dry. So, here are a few things you can do about it:
- Apply moisturizer 2-3 times a day
- Avoid soap – use only gentle cleansers instead
- Avoid long, hot showers because hot water can lead to dryness
If it’s really bothering you, treatments that may help are:
- Topical exfoliating products containing glycolic acid, lactic acid, or salicylic acid can help
- Prescription retinoids (tretinoin, adapalene, or tazarotene) can also help
Different from Acne: Keratosis pilaris is unrelated to acne. In fact, research shows that if you have keratosis pilaris, you are less likely to develop acne – that’s how different the two conditions are.

The Science
- Symptoms of Keratosis Pilaris
- Causes of Keratosis Pilaris
- Diagnosis
- Treatment
- Keratosis Pilaris and Acne
Symptoms of Keratosis Pilaris
Keratosis pilaris may develop at any age but usually starts either before the age of 2 or in adolescence.1 The condition is very common: it occurs in up to 70% of adolescents and 40% of adults.2 People of all ethnicities are equally at risk.
The signs and symptoms may include:
- Painless hard bumps 1-2 mm in diameter, which are often the same color as your skin but can also be red, white, pinkish, or brownish black (on darker skin).
- Dry, rough skin in the areas where the bumps occur.
- Deterioration during winter, when humidity is low and the skin tends to be drier.

The bumps may appear anywhere on the skin except for the palms and soles. The most common locations include:
In children:
- Upper arms (back)
- Thighs (front)
- Cheeks
In adolescents and adults:
- Upper arms (back)
- Thighs (front)
- Buttocks
The condition usually fades on its own by the fourth decade of life or sooner.
Causes of Keratosis Pilaris
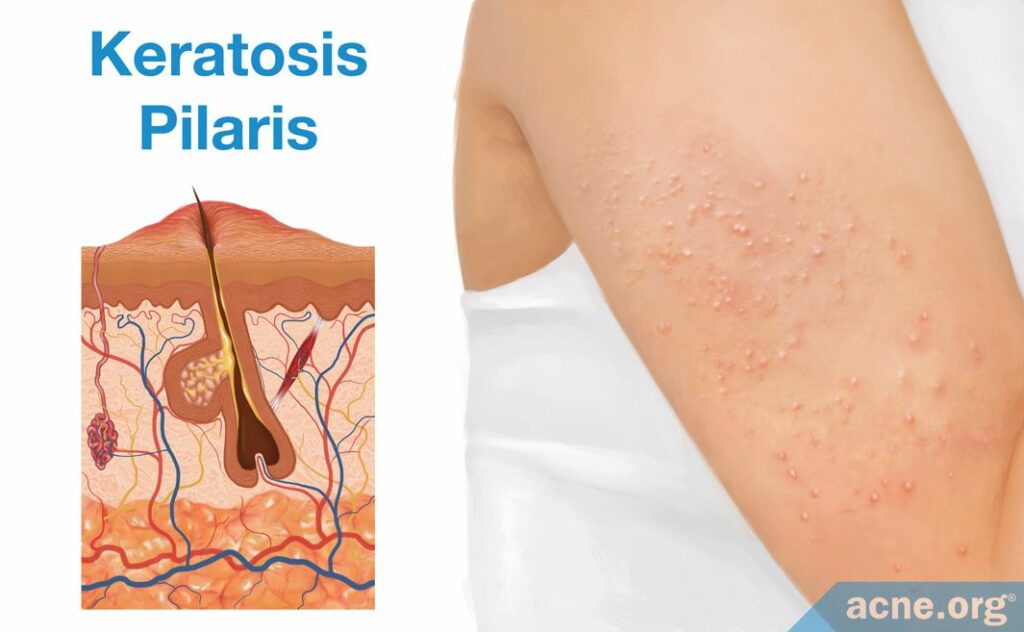
Keratosis pilaris develops due to the buildup of keratin around the top of skin pores. Keratin is the main protein of the epidermis (the uppermost layer of the skin) that performs a barrier function, preserving skin integrity and warding off bacteria, viruses, and harmful chemicals.
Normally, old skin cells containing keratin shed off and get replaced by new cells. However, in keratosis pilaris, cells containing keratin overproduce and/or shed off slower than usual, causing keratin to build up around the top of skin pores. We do not know why this happens.
Keratosis pilaris is a genetic condition that usually occurs in more than one family member. The way it is inherited is still being studied, but most likely it is passed on from a parent to child in an autosomal dominant pattern.2 In other words, there is a 50% likelihood of inheriting the condition if one of the parents has it and 75% likelihood–if both.
Many individuals with keratosis pilaris also tend to have one or several of the following conditions:
- Asthma
- Ichthyosis vulgaris (a condition causing extremely dry, thickened skin)
- Atopic dermatitis (red and itchy skin)
Diagnosis
Normally, you do not need to visit a doctor for keratosis pilaris. If you do want to consult a doctor, he or she will easily identify the condition by closely looking at the affected skin. No tests are required.
Treatment
You cannot cure keratosis pilaris, nor can you prevent it. The good news is that you do not need to–it is usually harmless and will fade away on its own over time. If the appearance it gives your skin disturbs you, try some of these self-care measures:
- Apply moisturizers at least 2-3 times a day. Dry skin worsens the symptoms. Moisturizers will help to keep it moisturized throughout the day.
- Avoid soaps. Soaps are known to dry the skin. Opt for gentle, moisturizing cleansers instead.
- Avoid long, hot showers. Hot water causes your skin to lose moisture after a shower more quickly.
If self-care measures do not help, your doctor may recommend a topical medication, such as:
- Over-the-counter exfoliating creams: Creams containing glycolic acid, lactic acid, and salicylic acid help by dissolving dead skin cells. Because they contain acids, exfoliating creams may cause burning and stinging and are not recommended for children.
- Prescription topical retinoids: These are creams containing derivatives of vitamin A (retinol, hence–retinoids). Examples of topical retinoids include adapalene, tretinoin, and tazarotene. Topical retinoids work by speeding up cell turnover and preventing pore clogging. Side effects of topical retinoids include skin dryness and irritation.
Keratosis Pilaris and Acne
Keratosis pilaris and acne are unrelated conditions. Acne is a disease that often requires treatment, while keratosis pilaris is a harmless condition that disappears over time.
The two conditions share similarities, however. Both in acne and keratosis pilaris, keratin builds up around the top of skin pores and causes the skin pores to clog. Hence, some medications used in the treatment of acne, such as over-the-counter exfoliating creams that dissolve dead skin cells and prescription topical retinoids that promote cell turnover, can also help in keratosis pilaris.
On the other hand, increased keratin production is not enough for acne to develop. Other key factors that must be present are the elevation of androgens, which are male hormones that are present in both males and females, and inflammation. At present, we have no evidence to say that hormones and inflammation are in any way related to keratosis pilaris. In fact, one study suggests the opposite: that your chances of developing acne may be lower if you have keratosis pilaris, and if you do happen to develop both conditions, your acne may be less severe compared to people who just have acne by itself.3
Expand to read details of study

The study was published in the Brazilian journal Anais Brasileiros de Dermatologia in 2014. The researchers examined 158 patients at a dermatology clinic for the presence of keratosis pilaris and/or acne. The patients were between the ages of 14 and 35. The researchers found that 26% of the patients had keratosis pilaris, while 66% had acne. Interestingly, the researchers found that the patients with keratosis pilaris were less likely to suffer from acne. If they did develop acne, it tended to be less severe compared to patients who did not have keratosis pilaris. The study authors wrote, “The presence of moderate to severe keratosis pilaris on the arms was associated with lower prevalence of acne vulgaris and lower severity of facial lesions in adolescents and young adults.” However, the researchers stressed that this study was small, and more research on the topic is necessary.3
Acne and keratosis pilaris are not mutually exclusive, which means you can have both simultaneously. For instance, you can have acne on the face and keratosis pilaris on the shoulders at the same time.
References
- Keratosis pilaris. American Academy of Dermatology (2018). https://www.aad.org/public/diseases/bumps-and-growths/keratosis-pilaris#treatment
- Keratosis pilaris. British Skin Foundation (2019). https://www.britishskinfoundation.org.uk/keratosis-pilaris
- Schmitt, J. V., Lima, B. Z., Souza, M. C. & Miot, H. A. Keratosis pilaris and prevalence of acne vulgaris: a cross-sectional study. An. Bras. Dermatol. 89, 91-95 (2014). https://www.ncbi.nlm.nih.gov/pubmed/24626653
