Topical Treatments Can Penetrate into the Skin in Several Ways

The Essential Info
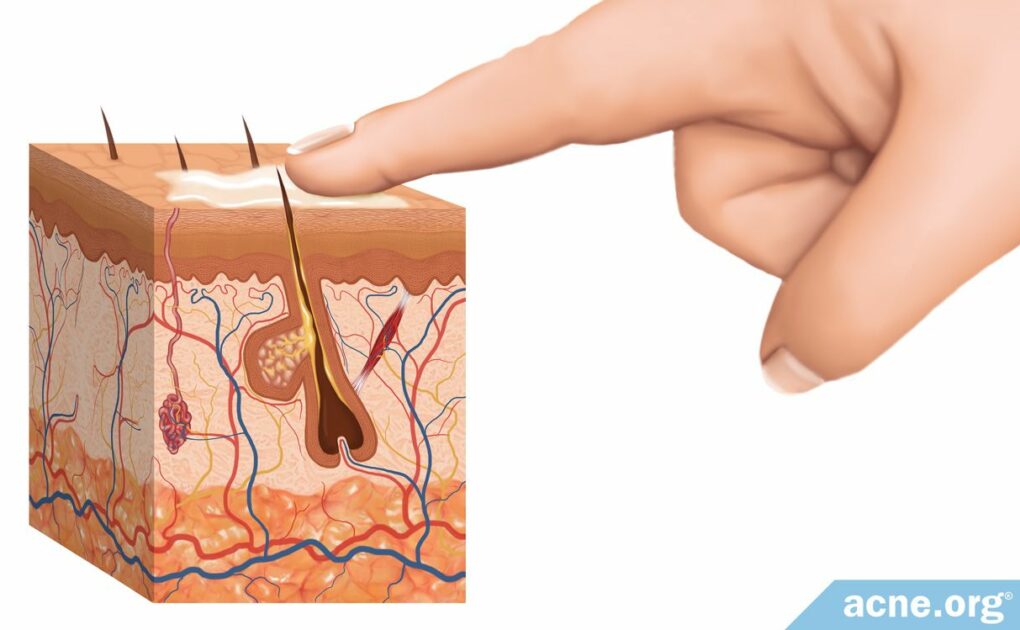
Topical treatments for acne must first pass through the outermost layer of the skin so they can reach the area of the skin where their action is needed.
The 3 ways topical treatments absorb are:
- Directly through skin cells
- Zig-zagging around skin cells (most common)
- Seeping into pores or sweat ducts
Caution – Deep Science Ahead: Continue reading below if you’re a biology nerd.

The Science
Topical drugs, including acne treatments, are effective only when absorbed into the skin. However, a drug has to pass through the outermost layer of the skin to get where it is needed.
To understand how the skin absorbs topical drugs, let’s begin with a quick review of the structure of the skin.
The skin functions as a physical barrier, protecting the body from the external environment and is made of three layers.
- Epidermis – outer layer
- Dermis – middle layer
- Hypodermis – deepest layer
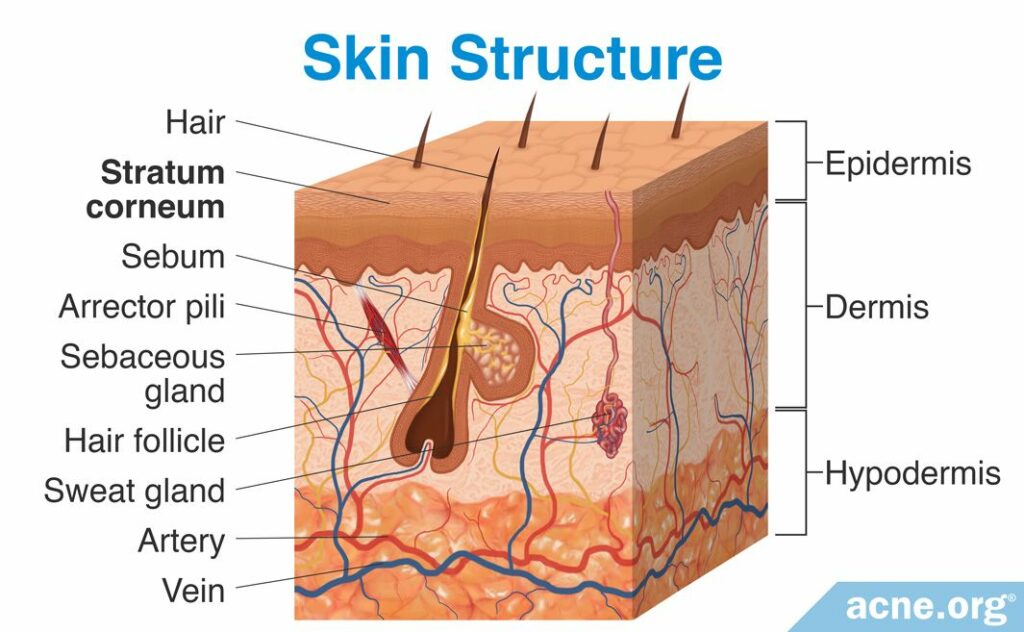
In order to be effective, most topical drugs need to pass through the outer layer of the skin, the epidermis, into the deeper layers of the skin.
It is not easy for most substances to pass through the epidermis, however, because the epidermis has a tough outermost barrier on it. This barrier, called the stratum corneum, is the primary obstacle to the movement of topical drugs through the epidermis into the deeper layers of the skin.1
The stratum corneum consists of tightly-packed, dry, flat cells called corneocytes. These cells are filled with keratin, a sticky protein. In between corneocytes are fats. You can think of the stratum corneum as a brick wall, with the corneocytes being the bricks and the fats being the mortar.2,3
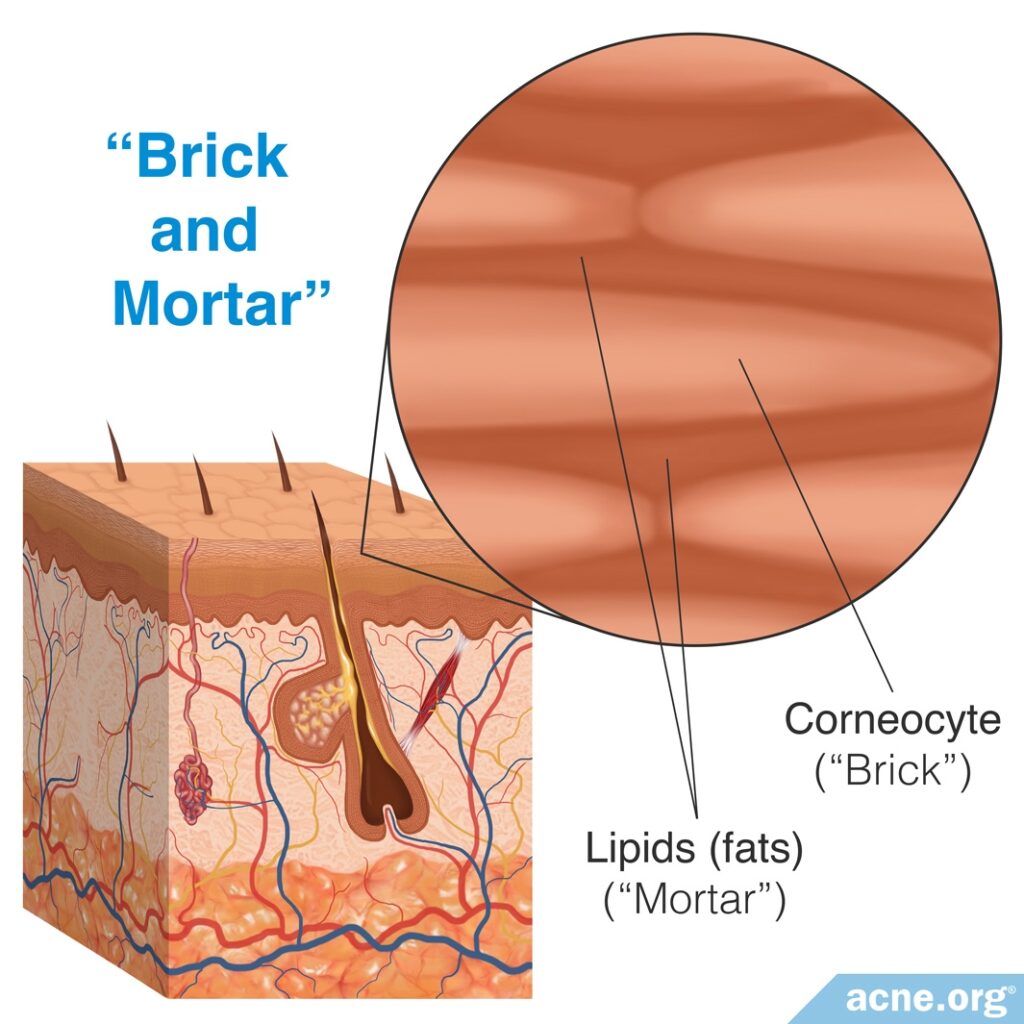
Although the bricks-and-mortar structure of the stratum corneum limits the passage of substances through the skin, some topical medications indeed are able to penetrate it and move into the deeper layers of the skin. These drugs move through the skin by three primary processes.
1. Transcellular Diffusion (Less Common)
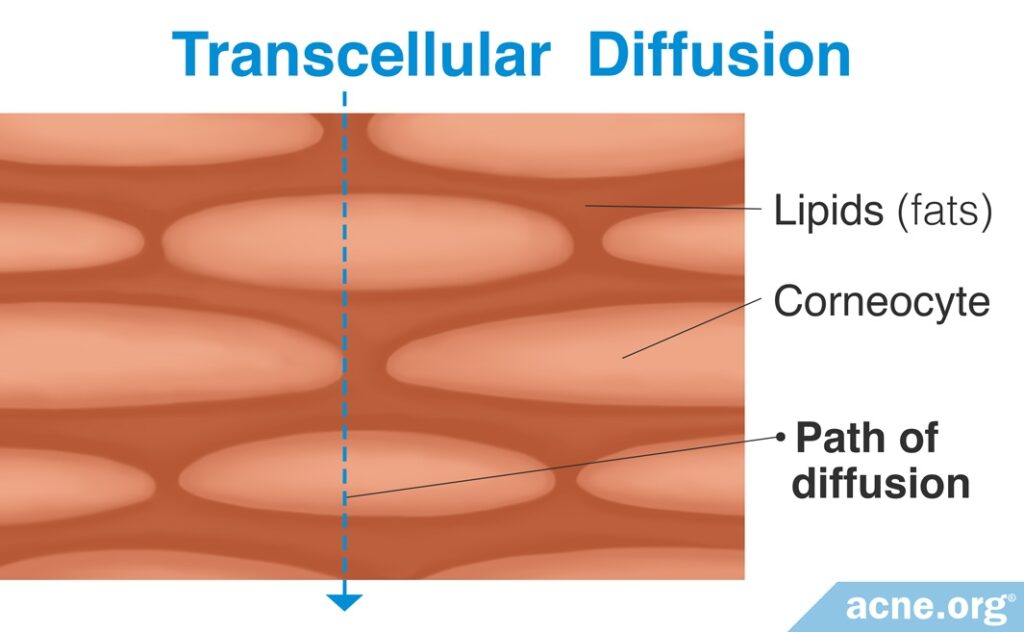
In transcellular diffusion, substances pass directly through both the corneocytes and fat of the stratum corneum. This is the most efficient method for a substance to absorb into the skin, but it also is the most difficult, as the substance must be able to move directly through cell membranes.7
The membrane of skin cells of the stratum corneum is semipermeable, which means that only some substances can pass through it. Each skin cell in the stratum corneum has a cell membrane consisting of two layers of molecules, including:
- Fats
- Proteins
The fat molecules create a central barrier within the membrane that is impermeable to water. These fat molecules can keep water-based substances from crossing the cell membrane. However, the cell membranes also contain certain proteins called integral proteins, which can aid the passage of some water-based substances through the fat molecules. These proteins act as channels through the fat molecules, allowing some substances to move through the cell. The protein channels tend to enlarge when the stratum corneum is well hydrated. Since larger channels enable better movement of substances through the membrane than smaller ones do, a well hydrated stratum corneum may absorb topical drugs more easily than a poorly hydrated one.
Although transcellular diffusion is the most efficient route for drug absorption, and it is possible for some substances to move directly through the cell membrane, as described above, many substances cannot easily pass through it. Therefore, most topical drugs are not absorbed via transcellular diffusion.5-7
2. Intercellular Diffusion (Most Common)
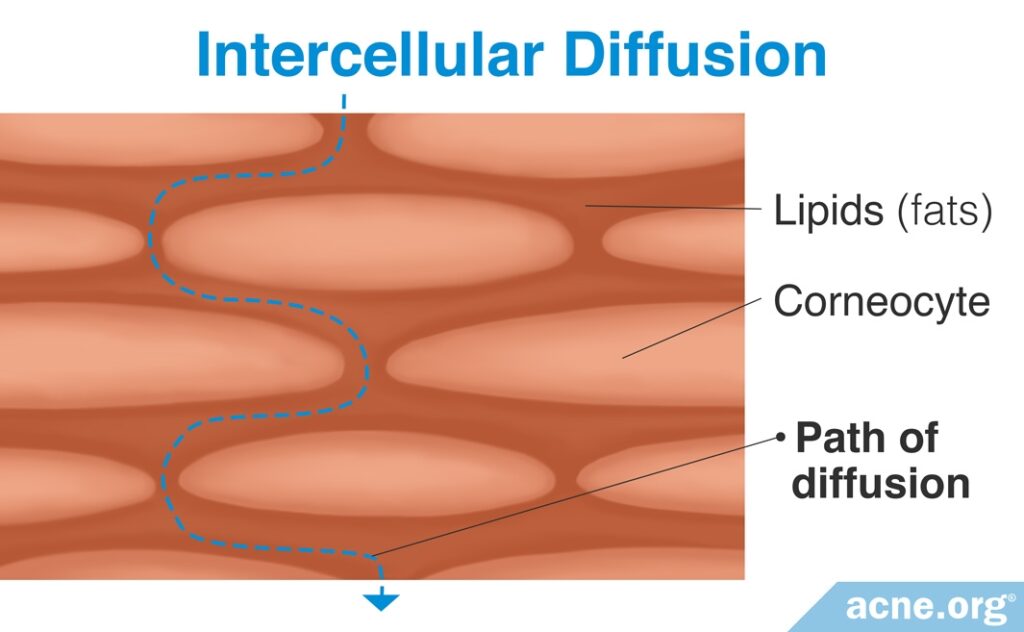
Intercellular diffusion is the most common method by which drugs absorb into the skin.7 Substances pass through the spaces around each skin cell instead of passing directly through the cells themselves.
Because of the bricks-and-mortar architecture of the stratum corneum, this is a less efficient method of transport – instead of moving in a straight line through both the “bricks” and “mortar” of the stratum corneum, substances must wind their way between each of the “bricks.”5
Although less efficient, it is easier for substances to absorb into the skin in this way because they do not have to cross the cell membranes.
3. Trans-appendage Diffusion (Less Common)
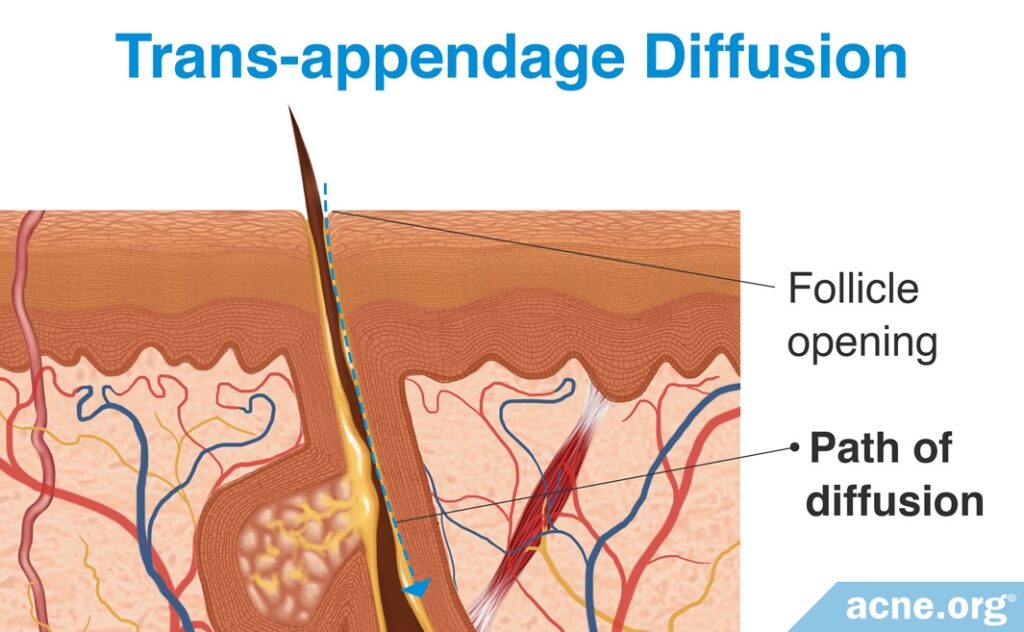
Trans-appendage diffusion is a process by which a substance bypasses the stratum corneum by moving through the hair follicle or sweat duct.
Because hair follicles and sweat ducts account for about only 0.1% – 1% of total human skin surface, not much can be absorbed via this method. Additionally, some research suggests that even where hair follicles and sweat glands exist in high numbers, absorption rates still are low. For example, drug absorption through the hands and soles of the feet, both of which contain a high density of sweat glands, is low.3,4,7
On the other hand, scientists are beginning to wonder whether trans-appendage diffusion might be more common for acne medications than previously believed. That’s because acne starts inside skin pores, a.k.a. hair follicles. Therefore, it makes sense that topical drugs that effectively fight acne might be penetrating the skin directly through hair follicles. In addition, some scientists argue for producing more acne treatments that penetrate the skin in this way.8-10 However, this is still a relatively new area of research, so time will tell whether trans-appendage diffusion might one day become more common for acne treatments than intercellular diffusion.
In Conclusion
Although there are three ways topical drugs may absorb into the skin, most medications absorb via intercellular diffusion, which means the drug penetrates the outermost layer of skin by moving through the spaces between individual skin cells.
References
- Arda, O., Goksugur, N. & Tuzun, Y. Basic histological structure and functions of facial skin. Clin Dermatol 32, 3 – 13 (2014). https://www.ncbi.nlm.nih.gov/pubmed/24314373
- Barrier, S. et al. Stratum Corneum Structure and Organization. In Medical therapy. 2065 – 2073 (2012)
- Benson, H. A. Transdermal drug delivery: penetration enhancement techniques. Curr Drug Deliv 2, 23 – 33 (2005). https://www.ncbi.nlm.nih.gov/pubmed/16305405
- Flynn, G. L. & Stewart, B. Percutaneous drug penetration: Choosing candidates for transdermal development. Drug Dev Res 13, 169 – 185 (1988). https://www.semanticscholar.org/paper/Percutaneous-drug-penetration%3A-Choosing-candidates-Flynn-Stewart/75da559a9392f5f82ddfda2015ff7ab803038891
- Menon, G. K., Cleary, G. W. & Lane, M. E. The structure and function of the stratum corneum. Int J Pharm 435, 3 – 9 (2012). https://www.ncbi.nlm.nih.gov/pubmed/22705878
- Spector, A. A. & Yorek, M. A. Membrane lipid composition and cellular function. J Lipid Res 26, 1015 – 1035 (1985). https://www.ncbi.nlm.nih.gov/pubmed/3906008
- Trommer, H. & Neubert, R. H. Overcoming the stratum corneum: the modulation of skin penetration. A review. Skin Pharmacol Physiol 19, 106 – 121 (2006). https://www.ncbi.nlm.nih.gov/pubmed/16685150
- Verma, A., Jain, A., Hurkat, P. & Jain, S. K. Transfollicular drug delivery: current perspectives. Research and Reports in Transdermal Drug Delivery 5, 1- 17 (2016). https://www.dovepress.com/transfollicular-drug-delivery-current-perspectives-peer-reviewed-article-RRTD
- Meidan, V. M., Bonner, M. C. & Michniak, B. B. Transfollicular drug delivery–is it a reality? Int J Pharm 306, 1-14 (2005). https://www.ncbi.nlm.nih.gov/pubmed/16260102
- Vyas, A., Kumar Sonker, A. & Gidwani, B. Carrier-based drug delivery system for treatment of acne. Scientific World Journal 2014, 1-14 (2014). https://pubmed.ncbi.nlm.nih.gov/24688376/