Pyoderma Faciale Is a Rare and Severe Form of Acne in Females

The Essential Info
Pyoderma faciale, also known as rosacea fulminans, is a rare, severe form of acne that occurs exclusively in females.
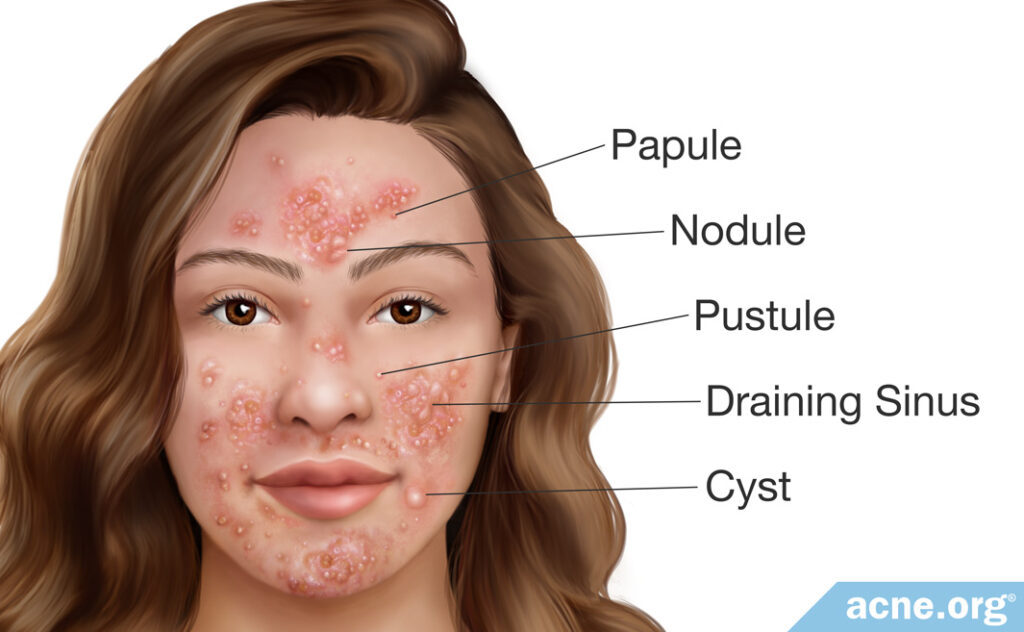
Symptoms are always limited to the face and include intense redness of the skin and a mixture of nodules, cysts, papules, pustules, and draining sinuses.
Treatment takes at least three months and usually consists of oral prednisolone (an oral steroid to reduce inflammation) and isotretinoin.

The Science
- Definition
- Incidence
- Causes
- Symptoms
- Pyoderma Faciale vs. Other Severe Forms of Acne
- Treatment
- Are Drugs That Suppress the Immune System an Option?
Definition
Pyoderma faciale, also known as rosacea fulminans, is a rare, severe form of acne occurring exclusively in females. It falls under the umbrella term nodulocystic acne, which refers to acne that features, but is not necessarily limited to, large, red, painful acne lesions called nodules and/or cysts. Pyoderma faciale in particular comes with numerous merging nodules and/or cysts on the face accompanied by intense inflammatory redness.
Incidence
It is rare. A typical patient is a woman in her twenties, but cases in females from 15 to 59 years of age have been reported.1-3 Males almost never develop pyoderma faciale.
Causes
Little is known about the causes of the disease, and it remains nearly as mysterious as it was when it was discovered almost 80 years ago. Scientists speculate that the following factors might contribute to its development:
- Underlying problems with blood vessels: People with pyoderma faciale have increased blood flow to the skin and widened blood vessels, which suggests that issues with the blood vessels might be one of the contributing causes.
- Hormonal fluctuations: Since the disease occurs almost exclusively in females and sometimes develops during pregnancy, fluctuating hormone levels are a logical suspect.
- Stress: In some patients, pyoderma faciale seems to begin after a stressful event or a period of chronic stress.
- Taking high doses of vitamins B6 and B12: In some patients, pyoderma faciale might be triggered by taking high doses of these vitamins.
- Treatment with ribavirin: Ribavirin is an antiviral medication that might trigger pyoderma faciale in some patients.
- Genetics: Some people’s genes might predispose them to developing pyoderma faciale.4,5
In addition, doctors notice that people who have pyoderma faciale are also more likely to suffer from inflammatory bowel disease, thyroid disease, or liver disease. However, the reason for this association is unclear.4
Symptoms
The onset of pyoderma faciale can be compared to a torrential rain that hits suddenly. The disease may emerge from healthy skin in patients who have never had a problem with acne.
In some patients, pyoderma faciale resolves spontaneously within a year, while in others it may persist for over a year and alternate between becoming more or less severe over that time.6 Consequently, some degree of scarring likely will occur, even with adequate treatment.
Pyoderma faciale is a form of nodulocystic acne that gives rise to a mixture of nodules, cysts, and draining sinuses (several cysts fused together under the skin). Whiteheads, blackheads, papules, and pustules may be present as well, but they are never a dominant feature. Lesions are accompanied by intense redness of the skin and, often, swelling.
Symptoms are always limited to the face, particularly the cheeks, nose, chin, forehead, and temples. The central portion of the cheeks is almost always involved.3
Nodules and cysts
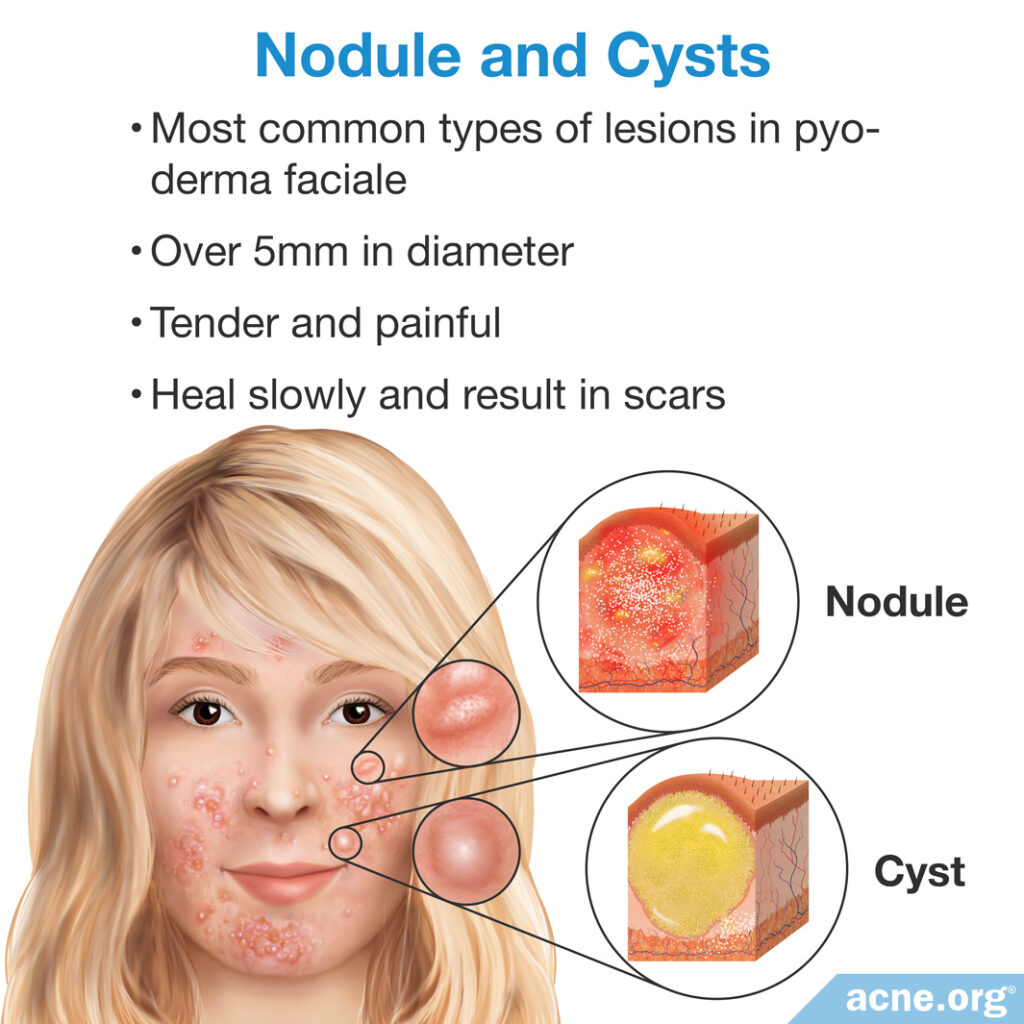
Nodules and cysts in pyoderma faciale are plentiful. Both types of lesions are over 5 millimeters in diameter and are tender and painful. The difference is that nodules are fibrous lesions that do not contain pus, whereas cysts contain “foul-smelling” pus-like material. Healing of both nodules and cysts can be extremely slow, often resulting in scars.
Draining sinuses
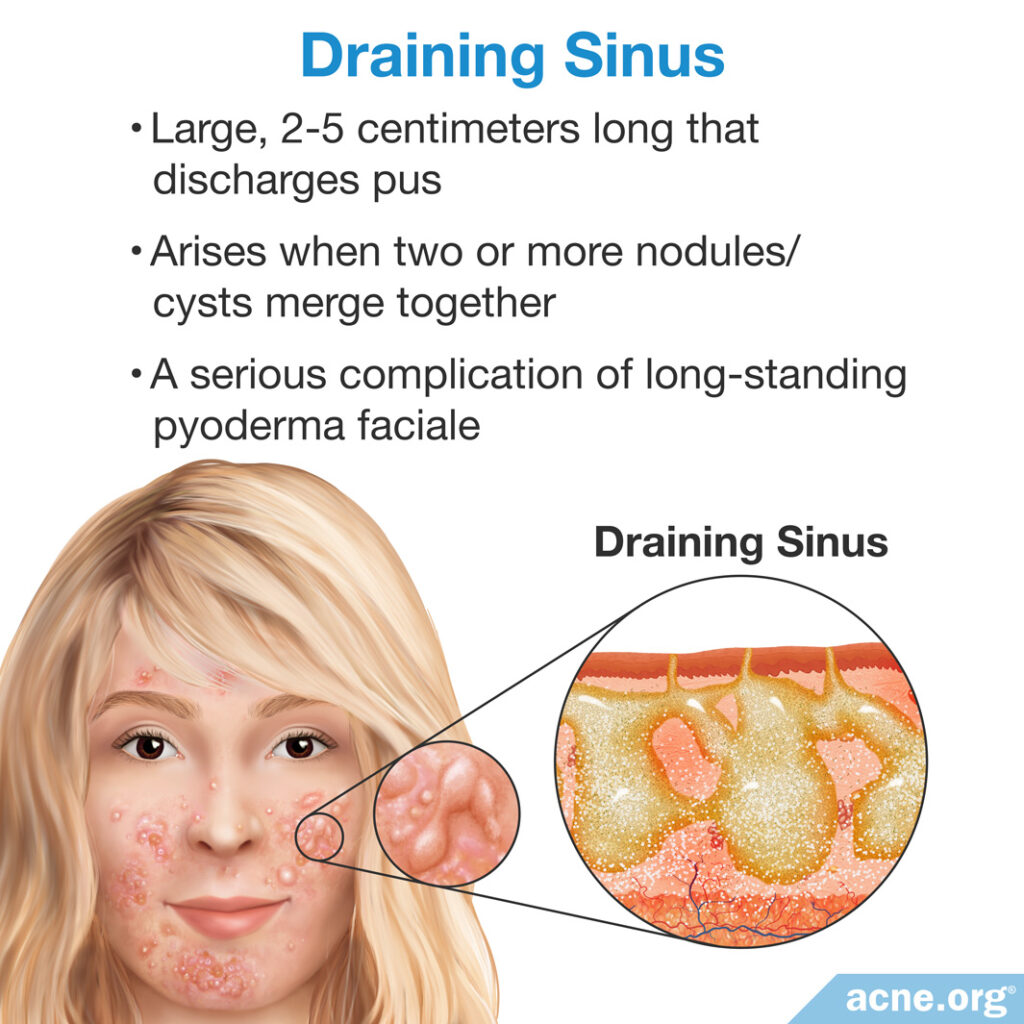
Draining sinuses arise when 2 or more nodules/cysts merge together under the skin to form a large, inflammatory lesion. They are a serious complication of chronic (persisting for a long time) pyoderma faciale. From the surface, a draining sinus is a large, 2 – 5 centimeter-long red bump that periodically discharges pus.
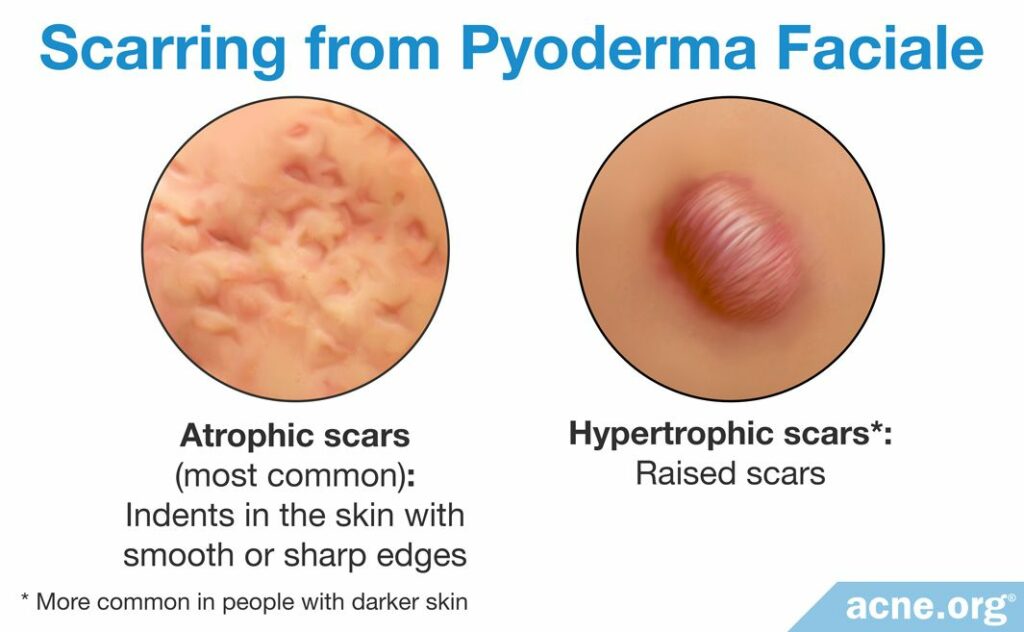
Scars
Scars in pyoderma faciale are often widespread and can be indented (atrophic) or raised above the skin (hypertrophic).

Pyoderma Faciale vs. Other Severe Forms of Acne
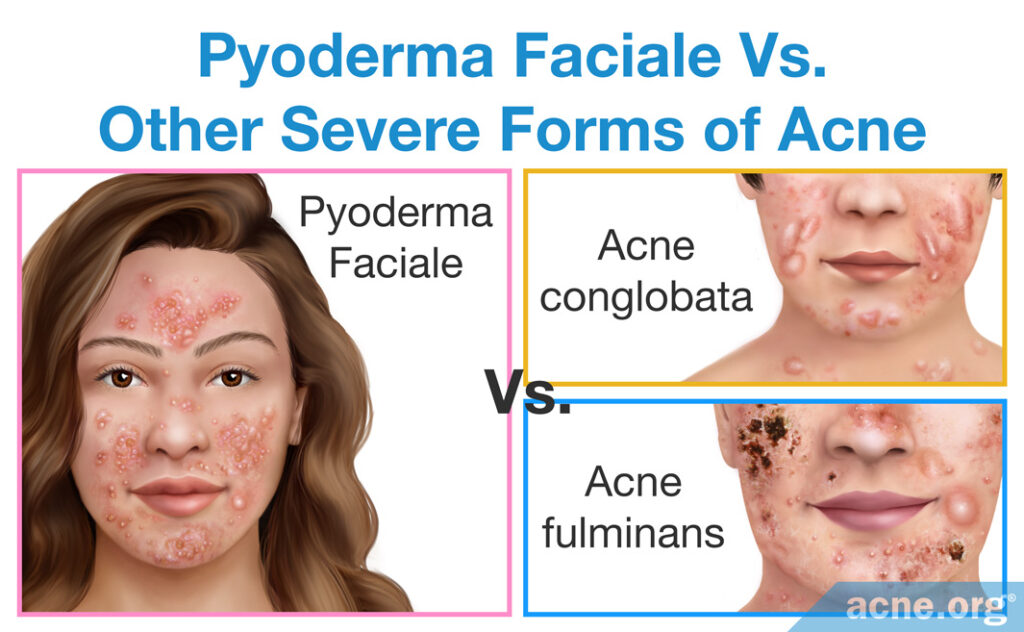
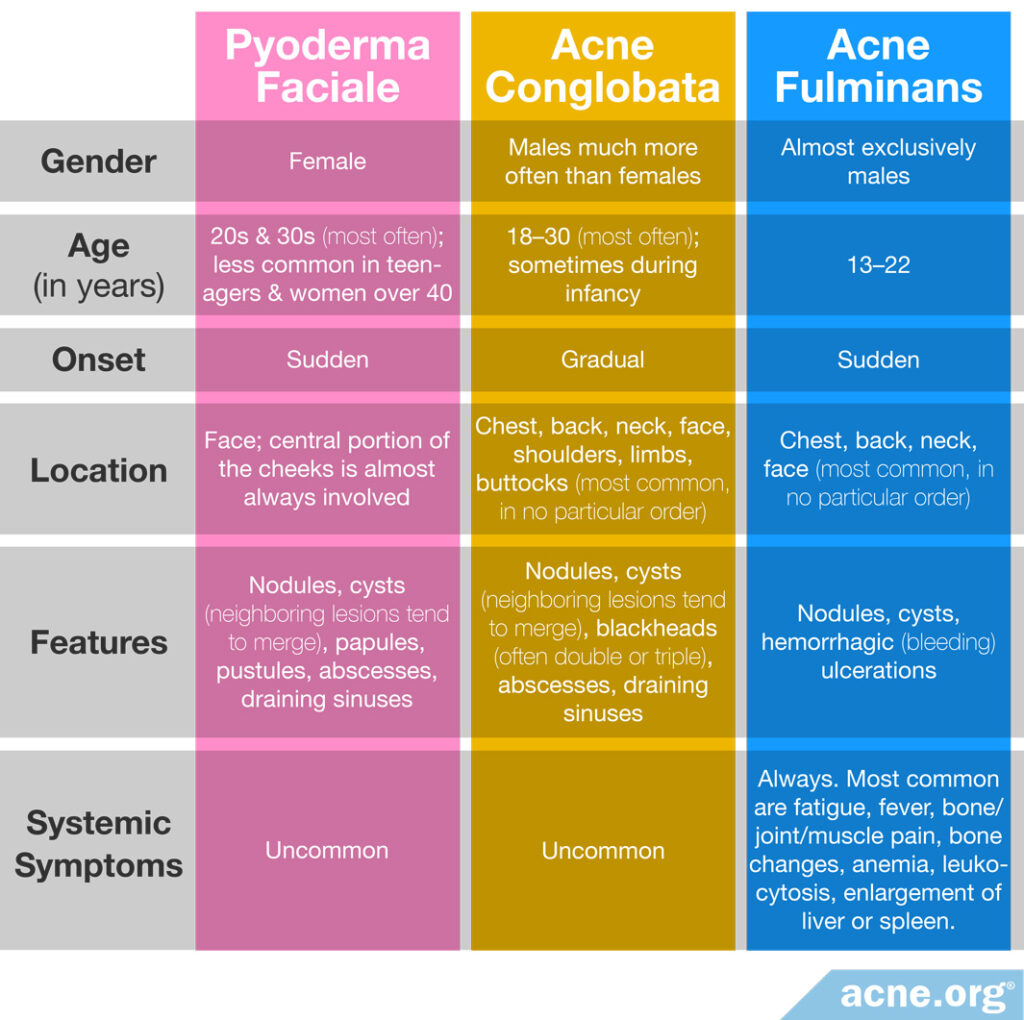
Pyoderma faciale should not be confused with other severe forms of acne–acne conglobata and acne fulminans.
Expand to read more about acne conglobata and acne fulminans
Acne conglobata
Acne conglobata patients present with lesions of all kinds, most notably nodules, cysts, blackheads, abscesses, and draining sinuses. In acne conglobata, lesions are never limited to the face and cover large areas of the chest, back, neck, face, shoulders, limbs, and buttocks. The disease typically affects young males.
Acne fulminans
Acne fulminans is rare–only about 100 cases have been documented so far.7 The disease features numerous painful nodules and/or cysts on the upper chest, back, neck, and face and systemic symptoms (symptoms that affect the whole body) like fever, fatigue, and muscle pain. Notably, nodules and cysts in acne fulminans fill with blood and rapidly turn into open wounds that very often leave massive, disfiguring scars. The disease almost exclusively affects young white males.
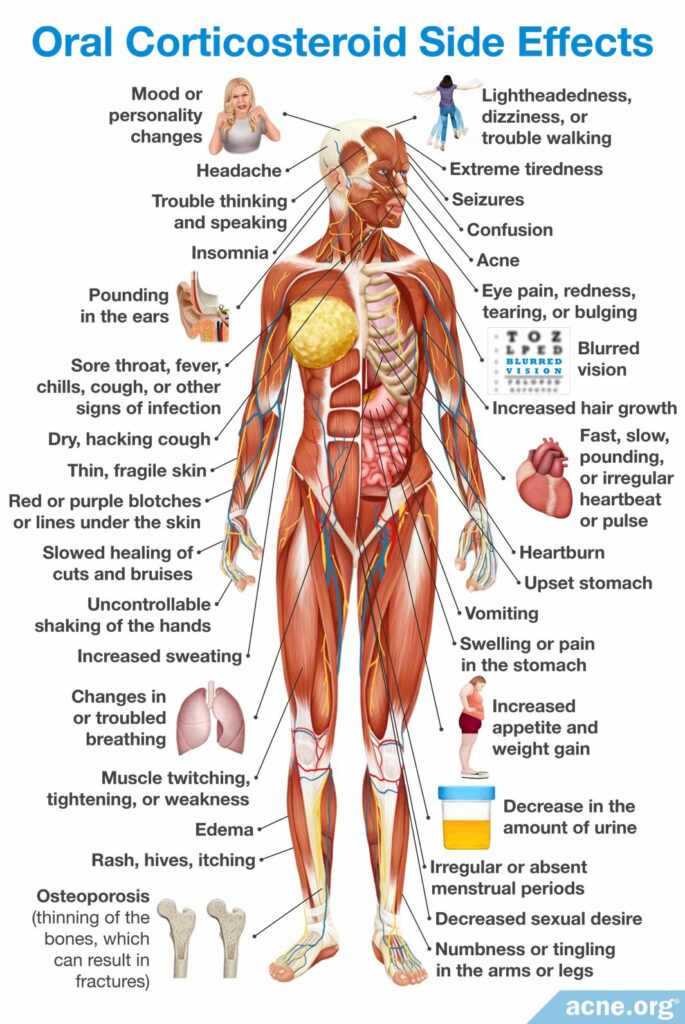
Treatment
Because the condition is so rare, little clinical evidence is available for analysis. Studies with documented treatment regimens for pyoderma faciale, acne conglobata, and acne fulminans show that a combination of an oral corticosteroid (e.g., prednisolone) and isotretinoin is the preferred treatment for severe, nodulocystic acne.6-11 Isotretinoin is a highly controversial drug that must be taken only in close supervision by a doctor and is associated with numerous hazardous health effects. Only the severity of the disease justifies the prescribing of this treatment option.
Another combination that doctors sometimes prescribe for pyoderma faciale is oral antibiotics plus isotretinoin. However, researchers recently reviewed the evidence from 135 cases of pyoderma faciale and concluded that corticosteroids plus isotretinoin seems to be a more effective combination.12
In rare cases, such as when a patient with pyoderma faciale is pregnant, doctors may prescribe oral antibiotics without isotretinoin.12
Oral corticosteroids and isotretinoin
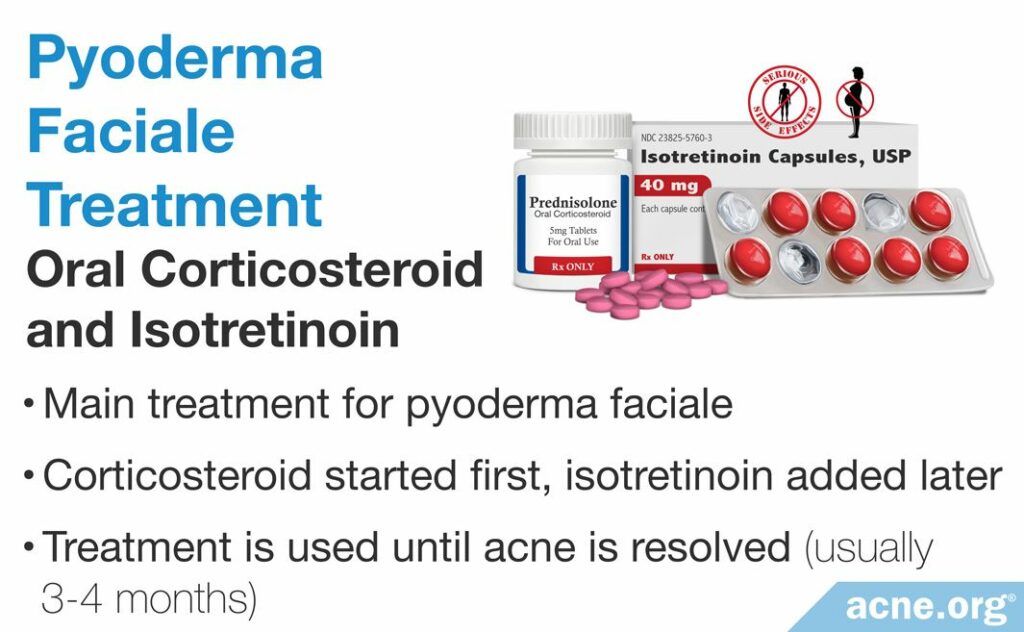
An oral corticosteroid taken in combination with isotretinoin is the mainstay of treatment. Usually, treatment starts with a corticosteroid for around six weeks. After two to four weeks from the start of the treatment with prednisolone, isotretinoin is incorporated. This means that a person takes both prednisolone and isotretinoin simultaneously for some time. The treatment course lasts until all lesions resolve, which usually takes over three months.6
Clinical trial on the effectiveness of an oral corticosteroid plus isotretinoin

In a 1992 study published in the Archives of Dermatology, researchers started treatment of pyoderma faciale patients with 1mg/kg/day of prednisolone for one to two weeks and then added 0.2 – 1mg/kg/day of isotretinoin, with a slow tapering of prednisolone to 0mg/kg/day over the next two to three weeks.6 The participants of the study, 20 in total, continued to receive isotretinoin until all inflammatory lesions cleared, which took three to four months.
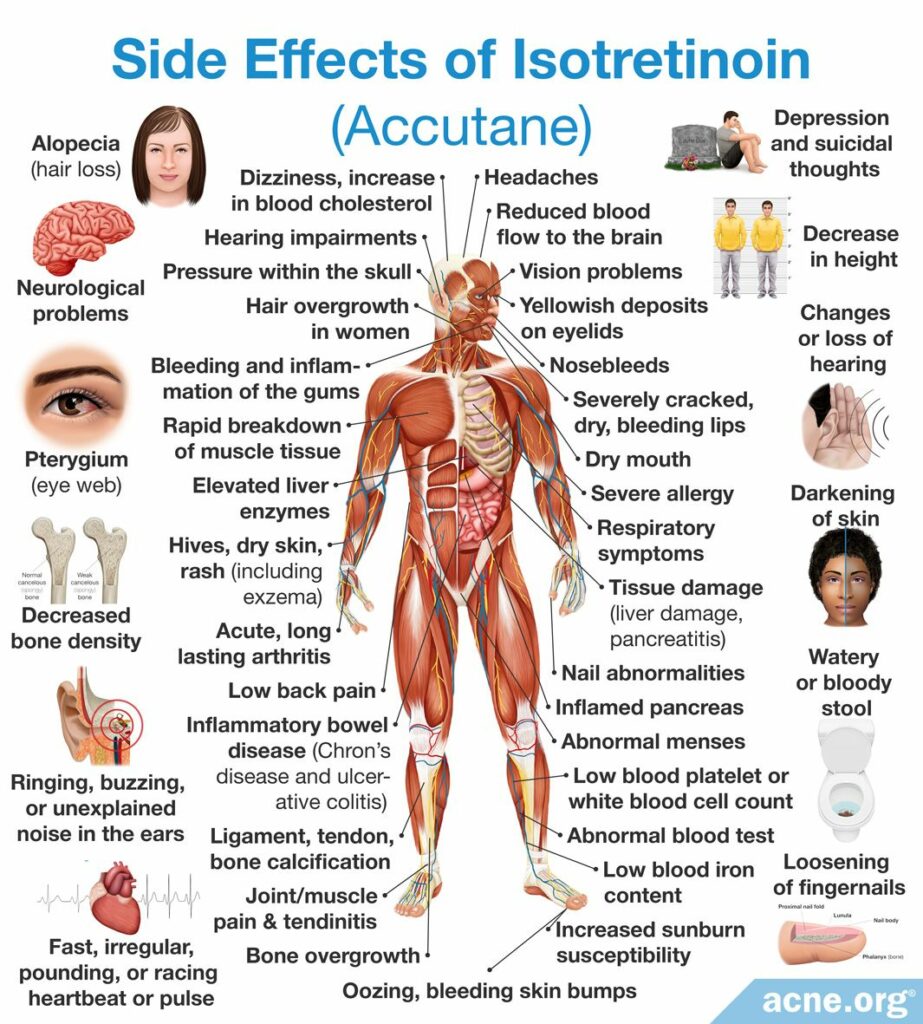
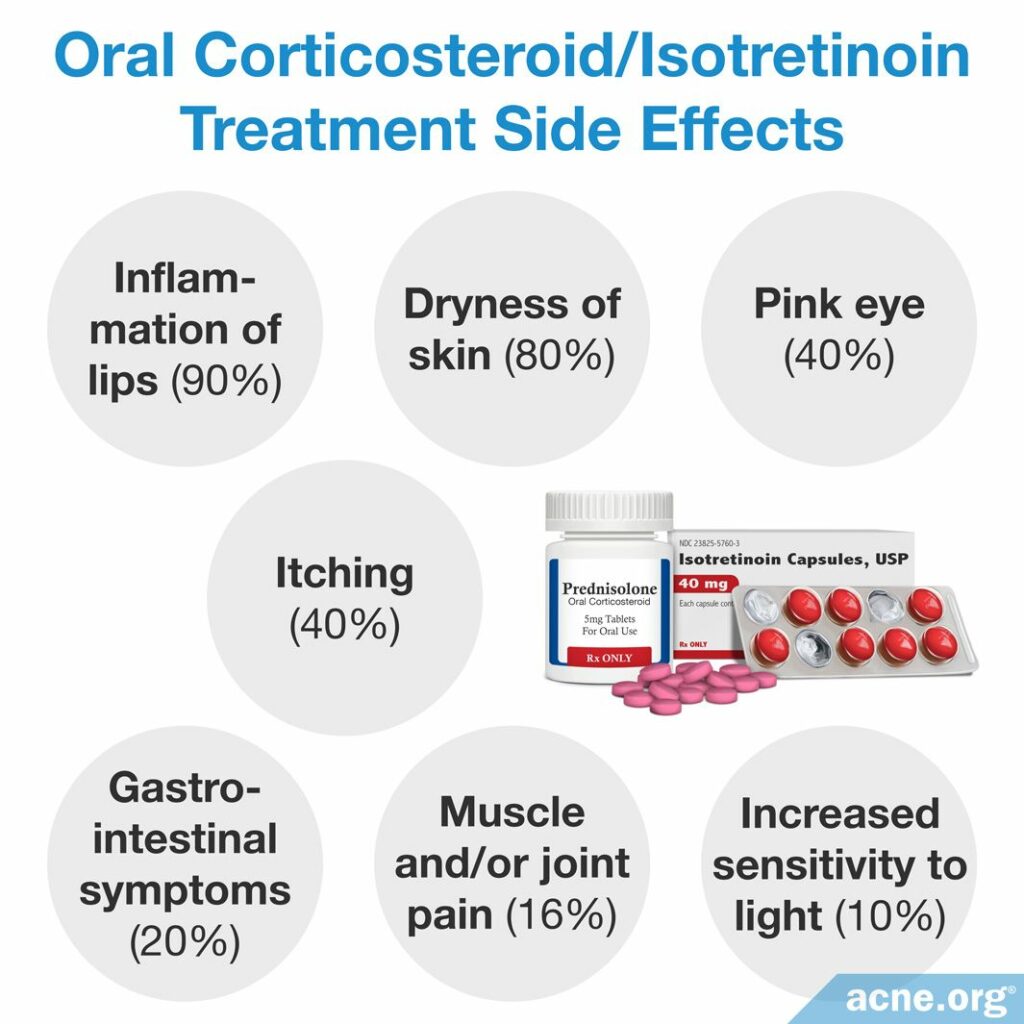
Despite being highly effective for severe acne, isotretinoin often comes with a long list of side effects and, sometimes, even severe, toxic reactions. This is why isotretinoin is approved for use only for nodulocystic acne.
The most frequent side effects of isotretinoin include:
- Inflammation of lips (90%)
- Dryness of skin and mucous membranes (80%)
- Pink eye (40%)
- Itching (40%)
- Gastrointestinal symptoms, such as nausea, vomiting, and abdominal pain (20%)
- Muscle and/or joint pain (16%)
- Increased sensitivity to light (10%)
Toxic reactions: Possible toxic reactions associated with the administration of isotretinoin might include inflammatory bowel disease and increased intracranial (in the head) pressure that causes moderate to severe headaches and visual impairments, such as blurred and double vision, difficulty seeing to the side, and brief episodes of blindness.13 The incidence of these events is unknown, but they are uncommon.
EXTREME CAUTION! Isotretinoin is contraindicated in pregnancy due to its severe adverse effect on the fetus.13 In fact, it is the #1 birth-defect -causing medication on the market. Birth defects are often severe, including death. That is the reason that it is strongly recommended for females to obtain two (2) negative pregnancy tests prior to starting therapy. Additionally, women must use two (2) forms of contraception for 30 days both before and after treatment with isotretinoin.
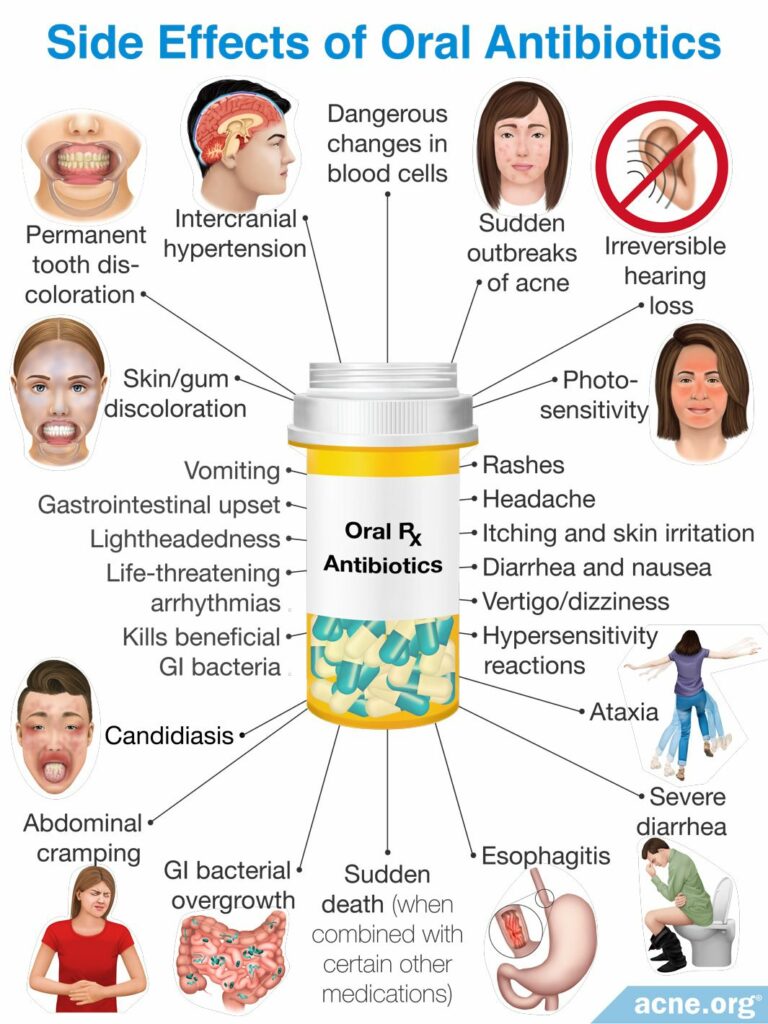
Oral antibiotics
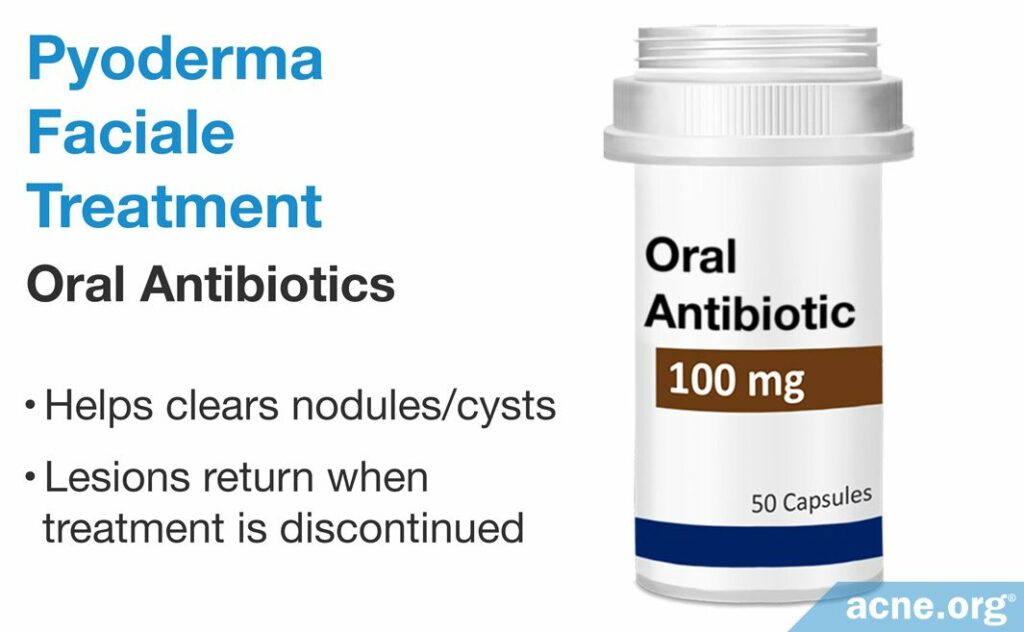
Evidence shows that an oral antibiotic + topical treatment might be able to replace the oral corticosteroid/isotretinoin combination in the treatment of severe acne, including pyoderma faciale, but results may take quite a bit longer to achieve.3,14 Due to the severity of the disease and potential for severe scarring, fast results are important.
Evidence on the effectiveness of an oral antibiotics + topical treatment

In a 1982 study carried out by the Mayo Clinic, 28 patients were treated with an oral antibiotic: 18 subjects received tetracycline; 2 were given erythromycin, and 8 were administered various agents, including erythromycin, sulfasalazine, trimethoprim-sulfamethoxazole, penicillin, and oxacillin. The patients also received some combination of topical treatments. At a follow-up after one year, complete remission (returning to the predisease state, with or without the emergence of a few new lesions) was achieved in 23 patients (79%) and in 16 patients (55%) after six months.3 However, the doctors stated, “[a]lthough remission was achieved in most patients…, [15] patients (51.7%) required treatment, usually oral antibiotics in conjunction with…benzoyl peroxide or topical antibiotics for longer than [one] year.”3
In 2011, the journal Clinical and Experimental Dermatology published a case report of a successful treatment of pyoderma faciale with another antibiotic called azithromycin. The case involved a 33-year-old woman who was pregnant. At the initial examination, the patient had papules, pustules, and nodules on the face, without whiteheads, blackheads, or systemic symptoms. The doctors diagnosed her with pyoderma faciale and prescribed azithromycin and a topical antibiotic called metronidazole for 12 weeks. After the end of the treatment period, the patient had no lesions on her face, her blood tests were normal, and her pregnancy ended with a normal delivery.14
Oral antibiotics also come with their own side effects and concerns as well.
Are Drugs That Suppress the Immune System an Option?
Doctors occasionally prescribe drugs that suppress the immune system to patients with very severe acne. These drugs include Otezla® (apremilast), Zyflo CR® (zileuton), Humira® (adalimumab), Enbrel® (etanercept), and Remicade® (infliximab), and work by reducing inflammation throughout the body. Inflammation is a major part of any type of acne, so it makes sense that reducing inflammation should improve symptoms.
Drugs that suppress the immune system might also help with pyoderma faciale, since this is a severe form of acne involving inflammation. However, no studies have tested immunosuppressant drugs on people with pyoderma faciale.
One reason doctors are generally hesitant to prescribe immunosuppressant drugs to acne patients is because by lowering the immune system, these drugs leave a person more susceptible to serious infections. Therefore, these drugs are only worth considering for people with very severe acne, for whom the benefit of improving their acne may outweigh the risk of contracting an infection. Pyoderma faciale may be one of the cases where these drugs might be appropriate.
Using immunosuppressant drugs to treat severe acne is an area of ongoing research, so keep an eye out for any new developments. I will be sure to post any updates here.
References
- Habif, T. Clinical Dermatology: A Color Guide to Diagnosis and Therapy (6th Edition). 231 – 233 (Saunders, 2015). https://www.elsevier.com/books/clinical-dermatology/habif/978-0-323-26183-8
- O’Leary, P. Pyoderma Faciale. Arch Dermatol 41, 451 (1940). https://jamanetwork.com/journals/jamadermatology/article-abstract/554581
- Massa, M. & Su, W. Pyoderma faciale: A clinical study of twenty-nine patients. J Am Acad Dermatol 6, 84 – 91 (1982). https://www.researchgate.net/publication/16983741_Pyoderma_faciale_A_clinical_study_of_twenty-nine_patients
- Coutinho, J. C., Westphal, D. C., Lobato, L. C., Schettini, A. P. & Santos, M. Rosacea fulminans: unusual clinical presentation of rosacea. An. Bras. Dermatol. 91 (5 suppl 1), 151‐153 (2016). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5325025/
- Veerkamp, P., Mousdicas, N. & Bednarek, R. Rosacea fulminans precipitated by acute stress: A case report describing an integrative approach for a patient reluctant to use isotretinoin. Integr. Med. (Encinitas). 15, 32‐35 (2016). https://www.ncbi.nlm.nih.gov/pubmed/28223895
- Plewig, G. Pyoderma faciale. A review and report of 20 additional cases: is it rosacea? Arch Dermatol 128, 1611 – 1617 (1992). https://www.ncbi.nlm.nih.gov/pubmed/1456755
- Zaba, R. Acne Fulminans. Emedicine.medscape.com (2016). https://emedicine.medscape.com/article/1072815-overview#showall
- Schwartz, R. “Acne Conglobata.” Emedicine.medscape.com. 2017. Web. 10 June 2017. https://emedicine.medscape.com/article/1072716-overview
- Karvonen, S. Acne fulminans: Report of clinical findings and treatment of twenty-four patients. J Am Acad Dermatol 28, 572 – 579 (1993). https://www.ncbi.nlm.nih.gov/pubmed/7681856
- Seukeran,D. C. & Cunliffe, W. J. The treatment of acne fulminans: a review of 25 cases. Br J Dermatol 141, 307 – 309 (1999). https://www.ncbi.nlm.nih.gov/pubmed/10468806
- Kunynetz, R. A Review of Systemic Retinoid Therapy for Acne and Related. Medscape (2004). at http://www.medscape.com/viewarticle/472395
- Walsh, R. K., Endicott, A. A. & Shinkai, K. Diagnosis and treatment of rosacea fulminans: A comprehensive review. Am J Clin Dermatol 19, 79-86 (2018). https://pubmed.ncbi.nlm.nih.gov/28656562/
- Hodgson, B. & Kizior, R. Saunders nursing drug handbook 2012. (W. B. Saunders Co., 2014).
- Fuentelsaz, V., Ara, M., Corredera, C., Lezcano, V., Juberias, P. & Carapeto, F.J. Rosacea fulminans in pregnancy: successful treatment with azithromycin. Clin Exp Dermatol 36, 674-676 (2011). https://pubmed.ncbi.nlm.nih.gov/21714808/